
Valorization of Erythrocyte Indices in the Neonatal Period - A Pilot Study
*Corresponding Author(s):
Sara FonsecaNeonatology Department, Centro Hospitalar Universitário De São João, Porto, Portugal
Email:sara_fonseca7@hotmail.com
Abstract
Background
Abnormal red blood cell indices are frequently missed among newborns that perform blood tests for any clinical reason. This study aims to follow the newborns referred to the Pediatric Hematology Consultation with abnormal erythrocyte indices, suspected of red blood cell pathology.
Methods
The Mean Corpuscular Hemoglobin Concentration (MCHC), Mean Corpuscular Volume (MCV), and its ratio of all healthy newborns that performed complete blood counts at the Regular Nursery for 2 years (2015 and 2016) were reviewed. Of those, all newborns referred to the pediatric hematology clinic in this period were evaluated and demographics, medical history, laboratory and diagnosis data were collected.
Results
During the study period, 1084 complete blood counts were considered, corresponding to 930 newborns. The MCV was 36.5 g/dl in 280 newborns; 29 newborns had both changes. A total of 514 newborns with an MCHC/MCV ratio >0.36 were identified. Thirty-one newborns were referred to the Pediatric Hematology Clinic. Hereditary Spherocytosis (2 cases) and α-thalassemia trait (3 cases) were diagnosed. Iron deficiency was detected and corrected in 11 cases.
Conclusion
Based only on abnormal erythrocyte indices, newborns were investigated, and pathological conditions (iron deficiency, Thalassemia, and Hereditary Spherocytosis) were detected, with the early diagnosis being emphasized. It is particularly important to carefully review the family history, evaluate the presence of hyperbilirubinemia and/or anemia and analyze the red blood cell indices.
Keywords
Hereditary spherocytosis; Iron deficiency; Newborn; Thalassemia; Red blood cell indices
Introduction
Iron deficiency, hemoglobin defects and red cell membrane disorders may have a variable presentation in the fetus and the newborn.
Abnormal red blood cell indices are frequently missed among newborns that perform blood tests for any clinical reason. Changes in Mean Corpuscular Volume (MCV) or Mean Corpuscular Hemoglobin Concentration (MCHC) can be early indicators of iron deficiency or the presence of hemoglobinopathy or other intrinsic disorder of the erythrocyte, and are often not assessed.
This study aims to follow the newborns referred to the Pediatric Hematology Clinic for the study of red blood cell pathology as well as the associated procedures. This characterization will improve the evaluation of newborns with abnormal red blood cell indices.
Materials and Methods
All healthy newborns that performed complete blood counts at the Regular Nursery for 2 years (2015 and 2016) were retrospectively investigated. We have collected the MCHC, MCV and the MCHC/MCV ratio.
The evaluation criterion was MCHC/MCV ratio >0.36, but the decision to refer to the Hematology Consultation was made individually by each physician in the Neonatology Department. All newborns in this period were retrospectively reviewed. Demographics, medical and family history, laboratory data and diagnosis were obtained.
Results
During the study period, 1084 complete blood counts were considered, corresponding to 930 newborns, as indicated in figure 1. The MCV was 36.5 g/dl in 308 blood samples (280 newborns); 29 newborns had both changes (MCV 36.5 g/dl). A total of 514 newborns with an MCHC/MCV ratio >0.36 were identified.
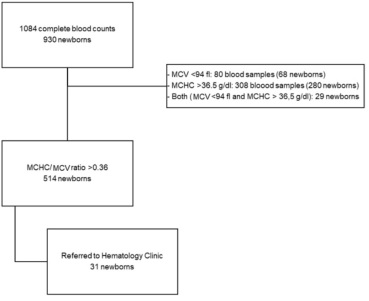 Figure 1: Study Outline.
Figure 1: Study Outline.
Thirty-one newborns were referred to the Pediatric Hematology Clinic due to suspicion of red blood cell pathology. The demographics and clinical characteristics of the newborns referred are shown in tables 1 & 2. There was a predominance of males. The median weight at birth was 3075 g (minimum: 2050 g, maximum: 4435g). Twenty-three (74.2%) had neonatal jaundice, of which 15 (65.2%) needed phototherapy. A positive family history of hematological disease was found in 7 (22.6%). In 5 newborns his mother (4/5) or father (1/5) had a history of iron deficiency anemia; in 2 newborns the mother had hereditary spherocytosis, and in one of them, the father was a carrier of HbS. No family history of thalassemia was known.
|
Indice |
Blood samples (n) |
Newborns (n) |
|
MCV < 94 fl |
80 |
68 |
|
MCHC >36.5 g/dl |
308 |
280 |
|
MCV 36.5 g/dl |
29 |
|
|
MCHC/MCV ratio >0.36 |
514 |
|
Table 1: Red blood cell indices.
|
|
n (%) |
|
Gender |
|
|
Male |
21 (67.7) |
|
Female |
10 (32.3) |
|
Neonatal jaundice |
23 (74.2), of which 15 (65.2) needed phototherapy |
|
History of iron deficiency anemia (parents) |
5 (16.1), mother: 4, father: 1 |
|
Family history of hematological disease (except iron deficiency anemia) |
2 (6.5) |
Table 2: Demographics and Clinical features.
Of the 31 patients, 8 (25.8%) did not complete the study due to missing/abandoned the follow-up. Regarding the 23 cases investigated, in 11/23 (47.8%) was documented an iron deficiency that was supplemented and corrected; 2 cases were diagnosed with Hereditary Spherocytosis (HS) (band 3 and protein 4.2 deficiency); and in 3 cases, alpha-thalassemia trait (heterozygosity for -alpha3.7 deletion (2), and an alpha chain variant c.885C>G [p.(Leu295Gln)] (1) were confirmed). One case is still under study for probable thalassemia.
Discussion
Important data on newborn complete blood counts, including interpretation of the red blood cell indices, in particular the MCHC and the MCV may be underestimated. In addition to carefully reviewing the family history and evaluating the presence of hyperbilirubinemia and/or anemia, the analysis of erythrocyte indices can be very useful in detecting inherited red blood cells pathologies.
In our study, it was possible to review the investigation performed in those newborns referred to the Pediatric Hematology Clinic based on abnormal erythrocyte indices in the neonatal period. In the consultation, all the newborns performed an investigation of iron deficiency and red blood cell pathology if indicated.
It is recalled that the erythrocytes of newborn infants are markedly macrocytic at birth, with an MCV over 110 fl, that drops after the first week and therefore a newborn with an MCV of less than 94 fl should raise suspicion for thalassemia trait or iron deficiency [1-3]. Also, the average MCHC is the same for full-term and premature infants, approximately 33 g/dl [1,2]. Taking into account that in a neonate with an elevated MCHC (MCHC >36,5g/dl), clinicians should consider that HS is likely [4,5]. Furthermore, if we calculate the neonatal HS ratio (MCHC/MCV) and obtain a value >0.36, the probability of being HS greatly increases and cannot be neglected [4].
In our study, of an initial sample of 930 newborns who had a complete blood count performed, 68 (7%) had MCV <94 fl, 280 (30%) had MCHC>36.5 g/dl and 514 (55.3%) had an MCHC/MCV ratio >0.36. Of those who had this suspicious ratio, 31 (6%) were referred for consultation, and afterward about a quarter of them abandoned or missed the consultation and only 23 cases were investigated. It should also be noted that this study included only newborns from the Regular Nursery, excluding patients who were admitted to the Neonatal Intensive Care Unit, namely cases with severe hyperbilirubinemia or anemia. Even so, in this small sample, it is important to highlight that diseases impacting on own and the families were diagnosed - HS (2) and α-thalassemia trait (3). Thus, we are concerned with cases that may have been missed. In this context, the importance of early diagnosis of these pathologies is highlighted, for adequate follow-up and also in the context of genetic counseling.
Reviewing our population of children followed in the Consultation, it should be noted that the majority had jaundice in the neonatal period, which is quite common, and that it may be the only precocious clinical manifestation of some hematological diseases, including HS.4 However, the underlying cause of jaundice frequently remains unidentified [4,6].
In our sample, the newborns had a family history of iron deficiency, anemia or another hematological disease in 16.1% and 6.5%, respectively. These data reveal the importance of reviewing family history, sometimes not mentioned by parents, remembering that intrinsic disorders of the erythrocyte represent some of the most common inherited genetic diseases [7].
As an example, it is estimated that 65% of neonates with HS have a parent with HS [4,7-9]. In this series, the mothers of both children who were diagnosed with HS, also had this disease.
We therefore consider that MCV, routinely used in adults and children to evaluate anemia, is still undervalued in newborn blood tests and can be particularly useful. In addition to inherited hematological pathologies in which early diagnosis is important and can prevent further diagnostic workup and unnecessary interventions, the importance of detecting iron deficiency is emphasized. Interestingly, in our series, in about half of the cases that completed the investigation, iron deficiency was detected and corrected. The prevalence of microcytosis and possible iron deficiency was also high (17.1% and 25% in preterm and term newborns, respectively) in another study by Guo R et al, which included 4915 infants admitted to the NICU, although it should be noted that in this study sick infants were included [10]. Although other important factors were not analyzed in our study (intrauterine growth restriction, birth weight for gestational age, maternal iron status, serum ferritin at birth, or type of feeding when iron kinetics was performed), it is important to consider that iron deficiency was found in apparently healthy children. The association between iron deficiency and neurodevelopment impairment and the importance of early supplementation, make it important for physicians [10].
This study has some limitations such as its retrospective nature. Moreover, the sample size is relatively small. Also, other factors that may influence erythrocyte indices, such as gestational age, were not analyzed. Nevertheless, only newborns from the Regular Nursery were included, where only the term/late-preterm newborns are admitted.
Conclusion
This study reinforces the importance of carefully review the family history, evaluate the presence of hyperbilirubinemia and/or anemia and analyze the red blood cell indices and accordingly, the importance of early suspicion and diagnosis is emphasized.
Only a very small fraction of newborns with abnormal red cell indices was evaluated and referred for further investigation.
In a sample of 23 newborns investigated at the Pediatric Hematology Clinic, HS (2 cases) and α-thalassemia trait (3 cases) were diagnosed. Also, in about half of these children, iron deficiency has been documented, and corrected.
Conflicts of Interest
The authors certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript.
Funding
The authors report no involvement in the research by the sponsor that could have influenced the outcome of this work.
Authors’ Contributions
All authors contributed equally to the manuscript and read and approved the final version of the manuscript.
Congresses
This paper was presented at the 49th Portuguese Congress of Neonatology that was held in Figueira da Foz, Portugal, in April 8 and 9, 2021.
References
- Jacob EA (2016) Hematological differences in newborn and aging: A review study. Hematol Transfus Int J 3: 178-190.
- LH (2015) Pediatric and geriatric hematology. Hematol Oncol Palliat Med.
- Beutler E, Lichtman MA, Coller BS (2011) General Hematology. Williams Hematology.
- Christensen RD, Yaish HM, Gallagher PG (2015) A pediatrician’s practical guide to diagnosing and treating hereditary spherocytosis in neonates. Pediatrics 135: 1107-1114.
- Christensen RD, Henry E (2010) Hereditary spherocytosis in neonates with hyperbilirubinemia. Pediatrics 125: 120-125.
- Johnson L, Bhutani VK, Karp KSE, Shapiro SM (2009) Clinical report from the pilot USA Kernicterus Registry (1992 to 2004). J Perinatol 29: 25-45.
- Steiner LA, Gallagher PG (2007) Erythrocyte Disorders in the Perinatal Period in Adverse Pregnancy Outcomes and the Fetus/Neonate. Semin Perinatol 31: 254-261.
- Sheffield MJ, Christensen RD (2011) Evaluating neonatal hyperbilirubinemia in late preterm Hispanic twins led to the diagnosis of hereditary spherocytosis in them, and in their sibling and in their mother. J Perinatol 31: 625-627.
- Perrotta S, Gallagher PG MN (2008) Hereditary spherocytosis. Lancet 372: 1411-1426.
- Guo R, Neumann D, Lafferty M, Boelig R, Bell-Carey B, et al. (2020) Prevalence and Utility of Low Mean Corpuscular Volume in Infants Admitted to the Neonatal Intensive Care Unit. J Pediatr 227: 108-113.
Citation: Fonseca S, Ferreira S, Teles MJ, Ferreira MF, Rodrigues M, et al. (2021) Valorization of Erythrocyte Indices in the Neonatal Period - A Pilot Study. J Neonatol Clin Pediatr 8: 083.
Copyright: © 2021 Sara Fonseca, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

