
Vascular Occlusion in the Lips: The Importance of Rapid Identification and Early Treatment
*Corresponding Author(s):
Fernanda Ramos Franco De SáDermatologic And Vulvar Academy, Brazil
Email:drafernanda.ramos@gmail.com
Abstract
Cutaneous ischemia, caused by vascular occlusion, is one of the most feared adverse events for clinicians resulting from the injection of Hyaluronic Acid (HA). An early intervention with application of Hyaluronidase (HYAL) will lead to the successful reversal of the isquemic condition - which might be severe and brings serious consequences to the patient. The authors report a case of injection of HA in the labial region, which resulted in a sub occlusion of the superior labial artery in which degradation was performed with HYAL at different time points. This study evaluates one of the side effects of using HA fillers in order to enable early diagnosis and treatment, and reduce morbidity and sequelae among patients.
Keywords
Hyaluronic acid; Hyaluronidase; Ischemia; Lip
Purpose
We report a case of vascular occlusion following injection of hyaluronic acid into the lip area with total reversal of the condition after a quick intervention using Hyaluronidase in high doses.
Introduction
Filler injections are the most popular nonsurgical procedure performed to increase the volume and improve the shape of the lips [1]. HA fillers are the most commonly used products for lip enhancement due some points: they are not permanent products, they are reversible with the use of HYAL and they have more natural aesthetic aspects (consistency, hydration and degradation over time) [2].
Cutaneous ischemia is one of the most serious and undesirable complications following injection of dermal fillers in aesthetic rejuvenation procedures. It is occurs by arterial embolism caused by HA or occlusion by compression, often with immediate manifestations. The initial diagnosis must be clinical, and the physician must intervene even without the presence of an ultrasound. Changes range from transient blanching, livedo reticularis, erythema to pallor, blister formation and, more rarely, necrosis and ulceration. Using HYAL in the right concentration and early application to treat occlusion will most certainly lead to the successful degradation and reestablishment of local blood flow [3].
This adverse effect constitutes a potential aesthetic concern and risk of irreversible damage to the patient if early diagnosis and early degradation are not implement [4-6]. The authors of the present paper report a case of ischemia after use of HA in aesthetic procedure to lip augmentation, reversed with HYAL at different time points, aiming for the reversion of the picture, demonstrating that early degradation led to a considerably faster resolution of the vascular event.
Case Report
A 43-year-old female patient, complained about being dissatisfied with the aesthetics appearance of her lips. After an individualized approach, we decided to performed two combined techniques: the Four-point injection Technique and the towering Technique [7].
Four entry points located 5mm below the vermilion border of the lower lip an 5mm above the vermilion border of the upper lip we made using a 27-gauge needle. Small boluses of 0,1 mL of HA (Restylane Kysse, Galderma), were made at each injection area, aspirating before the injection, with no alteration being observed at the moment of the procedure. 30-60 seconds after the fourth part of the lips (left upper lip), we observed a transient blanching and an erythematous-purplish area emerged. She didn´t complain about local pain as she had an anesthetic block.
Hyaluronidase Mesoestetic® (MD Ceuticals) was used immediatly for reverting the picture in a 500 IU application associated with the following drugs: 500mg Aspirin® (Bayer, Barmen, Germany), Injectable BetaTrinta® 5 mg/mL + 2mg/mL (Dipropionato de Betametasona + Fosfato Dissódico de Betametasona) (Eurofarma, São Paulo, Brazil).
After less than 30 minutes, there was a worsening, becoming a blue-gray color, progressing to the course of the right columellar artery and rising to the nasal tip, with a livedoid appearance. We started the High Dose Hyaluronidase Protocol [3], applying 1500 UI every hour, in a total of 4 vials, until the total reperfusion of the path and the improvement of the livedo reticularis. We also use warm compresses for 5-10 minutes, between HYAL applications (Figure 1) [8].
 Figure 1: Sequence of photos taken before each HYAL application: pallor interspersed with live do reticular is areas, compatible with arterial occlusion.
Figure 1: Sequence of photos taken before each HYAL application: pallor interspersed with live do reticular is areas, compatible with arterial occlusion.
Patient went home with the following oral drugs: 500mg/day Aspirin® (Bayer, Barmen, Germany) for 1 week, 500mg 12/12 hours Valacyclovir (GSK, São Paulo, Brazil), for 3 days, as the patient had a history of recurrent cold sores and maintain warm compress recommendation.
Doppler ultrasonography of the site can only be performed the next morning, about 14 hours after the event, showing the presence of flow in the left upper labial artery, with a serrated appearance and absence of flow to superficial communicating arteries (Figures 2&3).
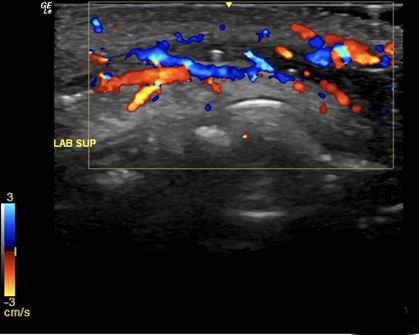 Figure 2: Ultrasound image with Color Doppler of the left upper lip, showing the presence of flow in the left upper labial artery, with a serrated appearance and absence of flow to superficial communicating arteries.
Figure 2: Ultrasound image with Color Doppler of the left upper lip, showing the presence of flow in the left upper labial artery, with a serrated appearance and absence of flow to superficial communicating arteries.
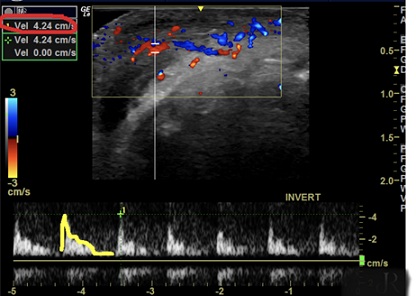 Figure 3: Spectral Doppler: a reduction in the Systolic Peak Velocity (SPV: 4.24 cm/s; reference value is 18.0 to 25.0 cm/s) and a biphasic flow with zero diastole, wich proves low flow tissue.
Figure 3: Spectral Doppler: a reduction in the Systolic Peak Velocity (SPV: 4.24 cm/s; reference value is 18.0 to 25.0 cm/s) and a biphasic flow with zero diastole, wich proves low flow tissue.
We decided to applied 1 more vial of HYAL (1500 UI) along the course of the left supralabial artery and right columellar artery, with complete reperfusion. Two days after, we repeated and demonstrated normal arterial blood flow (Figure 4).
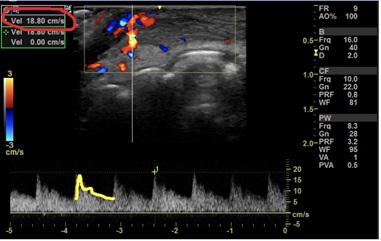 Figure 4: After injection of HYAL, in spectral Doppler we see the artery with normal perfusion and recovery of Systolic Peak Velocity (SPV: 18,8 cm/s).
Figure 4: After injection of HYAL, in spectral Doppler we see the artery with normal perfusion and recovery of Systolic Peak Velocity (SPV: 18,8 cm/s).
Improvement in the coloration was observed the next morning of the degradation, with complete resolution after 1 day (Figure 5).
 Figure 5: 12 hours after last application of HYAL, showing practically all the reversal of the mottled skin appearance; hematoma also in regression.
Figure 5: 12 hours after last application of HYAL, showing practically all the reversal of the mottled skin appearance; hematoma also in regression.
The patient evolved with progressive improvement and complete resolution of the bruise condition after 1 week. She did not present sterile pustules, local ulceration or any other cutaneous alteration except hematoma. For this reason, prophylaxis with antibiotic therapy was not prescribed.
Discussion
The use of minimally invasive cosmetic procedures has gained increasing popularity in recent years, with HA being the first choice for lip beautification. This increase in numbers of aesthetic procedures makes it extremely important to know the possible adverse reactions and respective handling when necessary [1].
The pathophysiology of the embolic process caused by these procedures has not yet been elucidated, nevertheless the decrease in blood flow may be linked to the volume injected and the site of injection of high viscosity fillers [9]. In our case reported, alterations in the blood flow resulting from application of HA were observed, with typical manifestations of ischemia.
The skin stages of vascular occlusion usually follows a relatively standardized trajectory: bleaching or pallor, livedo reticularis, emerging vesicles, pustules and devitalised tissue (necrosis or eschar), meaning it is crucial for the practitioner to recognize them early [10,11].
The use of hyaluronidase is recommended for the degradation of the material, which had a significant impact on the prognosis and normalization of the local blood flow and prevents sequelae [3,12]. The supportive therapy is based on increased perfusion, decreased inflammatory process and prophylaxis of associated infections, and may rely on vasodilators, corticosteroids, antimicrobials and antiaggregants.
Hyaluronidase (HYAL)
It is important to point out that the dosage of HYAL is highly variable, depending on the treated area and volume of HA placed, ranging from 450 to 1,500UI (in case of vascular occlusion) [3,13]. It may be injected slowly and into the site of HA injection [14]. As we do not know exactly where the obstruction is, we need to wet the entire volume of ischemic tissue with HYAL, because we need to hydrolyze the filler throughout the entire block of tissue [15].
Massaging is important for obtaining the therapeutic effect. HYAL treatment should be performed as soon as possible. In a review study, if HYAL were injected within 2 days, full recovery was expected. On the contrary, if injection of HYAL were delayed, there was an increase in the risk of scar and tissue defect formation [16].
Clinicians must work to minimize risks of vascular events by adopting a safer injection technique and must be able to recognize the clinical presentation of ischemia, having clear and effective protocols. The early identification of any complication, as well as swift and decisive treatment, is key to preventing long-term sequelae and improving the safety of the procedure.
Declaration of Participation
Fernanda Ramos Franco de Sá |ORCID 0009-0002-1839-264X
Main author, responsible for reviewing the manuscript and providing guidance to the other authors. Intellectual participation in propaedeutic and/or therapeutic conduct of the case.
Vivian de Carvalho Amaral | ORCID 0000-0002-5379-652X
Responsible for reviewing articles on the subject and writing the report.
Fernanda Aquino Cavallieri | ORCID 0000-0002-9465-3744
Responsible for reviewing articles on the subject and writing the report. Intellectual participation in propaedeutic and/or therapeutic conduct of studied cases.
Juliana Paulos de Rezende | ORCID 0009-0008-3737-9890
Responsible for reviewing articles on the subject and for writing part of the report. Responsible for the imaging tests that prove revascularization after the procedure employing hyaluronidase.
Barbara Bornay | ORCID 0009-0007-6835-5798
Responsible for reviewing articles on the subject and writing part of the report.
References
- Signorini M, Liew S, Sundaram H, De Boulle KL, Goodman GJ, et al. (2016) Global Aesthetics Consensus: Avoidance and Management of Complications from Hyaluronic Acid Fillers-Evidence- and Opinion-Based Review and Consensus Recommendations. Plast Reconstr Surg 137: 961-971.
- Lee A, Grummer SE, Kriegel D, Marmur E (2010) Hyaluronidase. Dermatol Surg 36: 1071-1077.
- DeLorenzi C (2017) New High Dose Pulsed Hyaluronidase Protocol for Hyaluronic Acid Filler Vascular Adverse Events. Aesthet Surg J 37: 814-825.
- Kim DW, Yoon ES, Ji YH, Park SH, Lee BI, et al. (2011) Vascular complications of hyaluronic acid fillers and the role of hyaluronidase in management. J Plast Reconstr Aesthet Surg 64: 1590-1595.
- Park TH, Seo SW, Kim JK, Chang CH (2011) Clinical experience with Hyaluronic acid-filler complications. J Plast Reconstr Aesthet Surg 64: 892-897.
- Rzany B, Becker-Wegerich P, Bachmann F, Erdmann R, Wollina U (2009) Hyaluronidase in the correction of hyaluronic acid-based fillers: a review and a recommendation for use. J Cosmet Dermatol 8: 317-323.
- Sahan A, Tamer F (2018) Four point injection technique for lip augmentation. Acta Dermatovenerol Alp 27: 71-73.
- Parada MB, Cazerta C, Afonso JPJM, Nascimento DIS (2016) Overview and management of fillers complications. Surgical & Cosmetic Dermatology 8: 342-3451.
- 9. Brody HJ (2005) Use of hyaluronidase in the treatment of granulomatous hyaluronic acid reactions or unwanted hyaluronic acid misplacement. Dermatol Surg 31: 893-907.
- Murray G, Convery C, Walker L, Davies E (2021) Guideline for the Management of Hyaluronic Acid Filler-induced Vascular Occlusion. J Clin Aesthet Dermatol 14: 61-69.
- Hirsch RJ, Brody HJ, Carruthers JD (2007) Hyaluronidase in the office: a necessity for every dermasurgeon that injects hyaluronic acid. J Cosmet Laser Ther 9: 182-185.
- Cohen JL (2008) Understanding, avoiding, and managing dermal filler complications. Dermatol Surg. 34: 92-99.
- DeLorenzi C (2013) Complications of injectable fillers, part I. Aesthet Surg J 33: 561-575.
- DeLorenzi C (2014) Complications of injectable fillers, part 2: vascular complications. Aesthet Surg J 34: 584-600.
- DeLorenzi C (2014) Transarterial degradation of hyaluronic acid filler by hyaluronidase. Dermatol Surg 40: 832-841.
- Sun ZS, Zhu GZ, Wang HB, Xu X, Cai B, et al. (2015) Clinical outcomes of impending nasal skin necrosis related to nose and nasolabial fold augmentation with hyaluronic acid fillers. Plastic Reconstr Surg. 136: 434-441.
Citation: de Sá FRF, Amaral VdeC, Cavallieri FA, de Rezende JP, Bornay B (2023) Vascular Occlusion in the Lips: The Importance of Rapid Identification and Early Treatment. J Clin Dermatol Ther 9: 0125.
Copyright: © 2023 Fernanda Ramos Franco de Sá, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

