
What Does Joy in Living Mean to Elderly Residents of Nursing Homes in Singapore? - The Full Study
*Corresponding Author(s):
Swapna DayanandanS R Nathan School Of Human Development, Singapore University Of Social Sciences, Singapore 599494, Singapore
Email:swapna002@suss.edu.sg; srswapnaram@gmail.com
Abstract
This secondary publication is based on a full study to explore the meaning of Joy in Living to elderly residents of nursing homes in Singapore, the enabling and disenabling conditions to Joy in Living in nursing homes and how Person-centred Care can support Joy in Living in nursing homes. The first publication was in May 2022 based on partial data of 16 semi-structured interviews with elderly residents and six participant observations of three nursing homes (pre and post interviews) between July 2021 and November 2021. The full study is based on 25 in-depth semi-structured interviews with elderly residents and eight participant observations of five nursing homes (pre and post interview observations for first three nursing homes and post interview observation for the last two nursing homes) between July 2021 and May 2022. The concept of Joy in Living is used in the study as it is unique to an individual’s experience; The study employed hermeneutical phenomenological research methodology to allow for the exploration of Joy in Living lived experiences of elderly residents through in-depth interviews and participant observations. Seven themes for Joy in Living experiences to flourish identified in the initial analysis of the partial data remains unchanged in the full study. There is a re-ordering of the themes in the full study as follows: ‘supportive nursing home environment and practices’, ‘meaningful daily living’, ‘connectedness through meaningful relationships’, ‘fulfil the need for spiritual care’, ‘personal control’, ‘adapting to changes’ and ‘desire to be free from worries’, each of which explains a facet of Joy in Living experiences of the elderly residing in nursing homes. There is a new subtheme ‘support for forgiveness and reconciliation’ under the theme “fulfil the need for spiritual care” in the final study. These themes include the enabling and disenabling conditions to Joy in Living in nursing homes. By focusing efforts and resources on enabling the seven themes, Joy in Living experiences of elderly will flourish in nursing homes. This in turn promotes better psychosocial well-being of the elderly and better living environments where nursing home residents may enjoy satisfactory accommodation while spending their remaining years in joy.
Keywords
Adapting to changes; Elderly; Free from worries; Hermeneutical phenomenology; Joy in living; Meaningful daily living; Meaningful relationships; Nursing homes; Personal control; Supportive environment and practices; Spirituality
Introduction
Medical advancements and higher living standards have resulted in longer average life spans. These factors, combined with declining fertility rates, have resulted in an ageing population both globally and Singapore. In 2021, 16.03% of Singapore’s total resident population (citizens and permanent residents) were 65 or older: the elderly population growth increased by 7.23 per cent from 8.80% in 2009 [1]. We expect that by 2030, one in every four Singaporeans will be 65 or older [2]. The expected burden on public health care expenditure in the Intermediate and Long-Term Care Sector (ILTC) of an ageing population is exacerbated by rising chronic diseases among the elderly [3]. Several initiatives are in place to alleviate this and allow older people to ‘age-in-place’ and within their communities. However, the rush to increase capacity may not have put the elderly resident at the centre of nursing home service design and delivery. Basu [4] noted that the elderly residents are cramped in the living quarters. Singaporeans have a negative perception of nursing home services. A qualitative study was conducted in 2015 among people aged 50 years and above on perceptions and attitudes regarding ILTC. It entailed one-on-one interviews with care recipients and their primary caregivers using various eldercare services available in Singapore, including nursing home services. Based on 30% of the interviews, the study discovered that nursing homes “neglect patients and restrict freedom cut across the responses of both users and nonusers of nursing homes, and their caregivers”. People mostly used nursing homes when their primary caregivers were unavailable. Despite this, the quality of care in nursing homes has improved dramatically since 2016 because of several initiatives by government agencies, Agency for Integrated Care (AIC) and the Ministry of Health (MOH), such as the Licensing Terms and Conditions on Enhanced Nursing Home Standards under the Private Hospitals and Medical Clinics Act.
A review of gerontological literature shows a gap in studies that focus on the joy experienced by elderly nursing home residents. Despite this, key findings indicate that holistic care models such as Person-centred Care [5], variations of person-centred care like Person-directed Care [6], Eden Alternative Model [7], and the Biopsychosocial Model of Health and Illness [8], have a positive impact on the well-being of the elderly in nursing homes. The impact of the care models on quality of care, quality of life, well-being, elderly satisfaction with services, and staff satisfaction working in nursing homes, is ‘measured’/assessed, with some reference to concepts of happiness and a Good Life, but little attention is paid to the joy experienced by care recipients.
Quality of life is defined as a “multi-dimensional construct with objective and subjective constructs, although the latter is often given greater priority” by Wang et al., [9]. Functional status is an example of an objective construct that can be measured using assessment instruments such as the Barthel scale. There is no consensus on a common definition for the subjective construct of quality of life, comprising but not limited to autonomy, enjoyment, employment and income, family relationships, meaningful endeavours, spiritual well-being and social support, according to Chaturvedi and Muliyala [10]. Well-being, compared to the quality of life, looks only at subjective attributes and has been measured by ‘happiness’ i.e., emotional reaction and ‘satisfaction’ i.e., cognitive evaluation of life, in studies on well-being [11]. According to Rinnan et al., [12] (p. 1469), “Well-being corresponds to processes where people perceive a good life based on their own merits and might be described as comprising joy, enjoyment, fulfilment, pleasure, satisfaction, happiness, involving elements as relationships with family and a sense of community”.
Is it possible to live a good life in old age? Do we have to say goodbye to the positive emotions of happiness as we age? Carstensen et al., [13] used “experience-sampling to examine the developmental course of emotional experience in a representative sample of adults spanning early to very late adulthood” (p. 21) for a one-week period that was repeated five and then ten years later in a Stanford study. Participants were given pagers and were required to respond to questions as soon as they were paged during the one week. They were asked how happy, satisfied, and comfortable they were. A key study finding is an improvement in emotional experience from early adulthood to old age, which, while contradicting common stereotypes about ageing, is consistent with the Selection, Optimisation, and Compensation (SOC) model of adult development [14]. The dynamic SOC model is a successful ageing theory that views ageing from early adulthood to old age as a life course of developmental change. The elderly can be content and live happy lives by being ‘selective’ in investing time and resources in goals and leveraging their expertise to ‘optimise’ performance in specific areas to ‘compensate’ for losses or limitations brought on by the ageing process.
Life course theory allows for the analysis of people’s lives within structural, social, cultural, and historical contexts across the four stages of the life course: childhood, adolescence, adulthood, and old age [15], and Erikson's [16] eight psychosocial stages of lifespan development, with a crisis of ‘integrity versus despair’ at the final stage of life, are invariably mentioned in studies on ageing. Two qualitative studies, one in the United Kingdom and one in Australia, have been conducted to investigate the Good Life concept of seniors living in care facilities [17-19]. According to Minney and Ranzijn [19], Good Life “encompasses both the value of one’s life and well-being in general” (2016, p. 919). Both well-being and Good Life, which are subjective constructs, have a value component, i.e., the person evaluates his life and provides an assessment of it. The quality of life construct, on the other hand, has both objective and subjective attributes that are independent of an individual's assessment of ‘quality’.
So, what about Joy? Joy stems from things that have more intrinsic value (for example, the belief that one has a purpose in life) and being happy in the face of losses such as loss of physical functioning, which results in poor health, loss of income from retirement, and even loss of a loved one. For those over the age of 70, the integrative process is critical for inner contentment, harmony, and joy based on one's values, life purpose, meaning and religious beliefs [20]. Because of the impending reality of death, people frequently ask existential questions as they grow older. In this sense, Joy can be seen as a step beyond Good Life.
A qualitative study was carried out to determine the essence of Joy of Life for elderly residents of Norwegian nursing homes [12]. In that study, the researchers employed the concept of Joy of Life, a multidimensional construct “that appears more closely related to subjective well-being commonly defined in social science as the absence of negative emotions, the presence of positive emotions, and life satisfaction, all of which corresponding to the concept of flourishing” [12]. Inspired by these studies in other countries, and the findings of local quantitative studies on nursing homes that psychosocial well-being is not being addressed, I have modified and narrowed down on a concept that I believe is relevant to the Singapore context. In this study, the concept of Joy in Living is used instead of Joy of Life because it has a strong applied focus and, in my opinion, a concept that is ‘dynamic’ and operationalised in concrete terms would be easier for Singapore nursing home residents to understand. So, I developed the concept of Joy in Living, which is rooted in the present and includes physical, psychosocial and spiritual dimensions. By researching this concept, I hope to add another dimension to holistic approaches to care in Singapore nursing homes.
There are no hypotheses for this study, instead there are four research questions to guide the study as follows:
- What does Joy in Living mean to elderly residents of nursing homes in Singapore?
- What are the enabling conditions that are conducive for Joy in Living in nursing homes?
- What are the disenabling conditions that are not conducive for Joy in Living in nursing homes?
- How does Person-centred Care support Joy in Living in nursing homes?
Materials and Methods
Design
The hermeneutical phenomenological research methodology is used for the study that depends heavily on research participants -the elderly in nursing homes- recalling their lived experiences in those homes and reflecting critically on the meaning they ascribe to Joy in Living [21]. The researcher conducting this study is part of the study to interpret and identify the essences of each lived experience, the meaning ascribed to Joy in Living, and find the language to convey the essences of the data collected and analysed. There are six research activities that provide the methodological structure of phenomenological research studies [22]. This qualitative study was conducted between July 2021 and May 2022. This study is based on 25 in-depth semi-structured interviews with elderly residents and eight participant observations of five nursing homes (pre and post interview observations for first three nursing homes and post interview observation for the last two nursing homes).
Participants
A total of 25 elderly participants were selected from five nursing homes: two homes with more than 300 beds but less than 500 beds and the other three homes with more than 100 beds but less than 300 beds. Inclusion criteria were participants being 65 years and above of age, residing in the nursing home for at least one year, a Singapore citizen or permanent resident in Singapore, ability to understand and speak in basic English. Bed-bound and residents with dementia, as assessed by the nursing home, were excluded.
Data collection
The data collection methods in this study are in-depth individual face-to-face interviews with elderly research participants using semi-structured interview guide and running records of onsite observations as a participant observer. The concept of Joy in Living was introduced to the participants at the start of the interview and in the Participant Information Sheet given to all participants. The following topics were covered in the interview:
- Participants’ background and why they are in a nursing home
- Participants’ day-to-day living experience in the nursing home
- Participants’ religious/spiritual beliefs, their belief system and purpose in life
- Participants’ understanding of Joy in Living, their views whether Joy in Living is possible in a nursing home and why if their answer is either yes or no
- If participants are living a joyful life in the nursing home, what are the things contributing to it and vice versa
Eight onsite participant observations were conducted at the five nursing homes. Only one observation session was conducted at the last two nursing homes each due to the evolving COVID-19 situation during the data collection phase of the study. Each observation session was eight hours that was either conducted over one day with an hour’s break in between the am and pm sessions or half days over two days. There was an interruption to data collection through face-to-face interviews and onsite observations for about two months from mid-September 2021 to mid-November 2021 and January 2022 to March 2022 due to development of COVID-19 clusters in a few nursing homes and the national policy response to suspend in-person visits to nursing homes. To allow for operational flexibility given the evolving COVID-19 situation and emergence of ‘Omicron’ new COVID-19 variant detected in December 21, interviews were conducted over ‘Zoom’ online platform with video function from middle of September 2021 onwards.
Data analysis
Data analysis was conducted after collection of data from each nursing home, where Joy in Living was used as the analytical concept for the analysis of the data to identify ‘significant statements’ and ‘clusters of meaning’ about Joy in Living from the transcripts of interview and observation audio records. The thematic statements chosen were those phrases that seemed to particularly allude to the Joy in Living experiences [22]. In hermeneutical phenomenological studies, van Manen [22] offered three methods: (i) wholistic approach; (ii) a selective approach; and (iii) the detailed or line-by-line approach for identifying themes during data analysis. These approaches can be used to discover themes or facets of a pattern of the phenomenon across datasets. As the wholistic and selective methods do not detail out the step-by-step process to conduct data analysis, the first author applied the phases of Reflexive Thematic Analysis [23,24] to guide the process.
Reflexive Thematic Analysis (RTA) is compatible with hermeneutical phenomenological studies as it is “about the researcher’s reflective and thoughtful engagement with their data and their reflexive and thoughtful engagement with the analytic process”, and the first author has conceptualized themes “as patterns of shared meaning underpinned or united by a core concept (we later conceptualized this as a ‘central organizing concept’ . . . ” ([25], pp. 593-594). Before commencement of data analysis, the transcripts were read several times to aid recall and familiarity with the content by immersing in the data. During data analysis, NVivo-Windows January 2022 Release 1.6 (NVivo) software was used. NVivo was used to document the ‘significant statements’ as ‘codes’, i.e., a short phrase to describe what is said in the elderly interview and the observation transcripts, gather all the quotes that were carefully tagged to the codes, and identify ‘clusters of meaning’ as higher-order conceptual ‘themes’ to answer the research questions [22,23,26]. NVivo was used to handle and analyse the different types of data from the research study, e.g., field notes, transcripts of the interview, and the observation audio recordings and photographs of objects, environment, and activities with faces of people obscured.
To strengthen research rigour, the interview and observation guides were piloted in a nursing home that was not included in the study, and data were collected and analysed through methodological triangulation. In the pilot study, where the elderly participant required clarification, prompts were added to the interview questionnaire (e.g., prompts were added to the questions on belief system and purpose of life).
Results
|
Name of Resident |
Gender |
Ethnicity |
Length of Stay |
|
Nursing Home A |
|||
|
A1 |
Female |
Indian |
3 - 5 years |
|
A2 |
Male |
Chinese |
1 - 2 years |
|
A3 |
Male |
Chinese |
1 - 2 years |
|
A4 |
Male |
Chinese |
1 - 2 years |
|
A5 |
Male |
Chinese |
>5 years |
|
Nursing Home B |
|||
|
B1 |
Female |
Chinese |
3 - 5 years |
|
B2 |
Female |
Chinese |
>5 years |
|
B3 |
Male |
Chinese |
3 - 5 years |
|
B4 |
Male |
Chinese |
1 - 2 years |
|
B5 |
Male |
Eurasian |
3 - 5 years |
|
Nursing Home C |
|||
|
C1 |
Male |
Chinese |
Over 5 years |
|
C2 |
Male |
Chinese |
1 - 2 years |
|
C3 |
Male |
Chinese |
1 - 2 years |
|
C4 |
Male |
Indian |
3 - 5 years |
|
C5 |
Male |
Indian |
3 - 5 years |
|
C6 |
Male |
Malay |
3 - 5 years |
|
Nursing Home D |
|||
|
D1 |
Male |
Indian |
3 - 5 years |
|
D2 |
Male |
Chinese |
3 - 5 years |
|
D3 |
Female |
Chinese |
1 - 2 years |
|
D4 |
Female |
Chinese |
3 - 5 years |
|
Nursing Home E |
|||
|
E1 |
Male |
Indian |
3 - 5 years |
|
E2 |
Female |
Indian |
1 - 2 years |
|
E3 |
Female |
Chinese |
3 - 5 years |
|
E4 |
Male |
Chinese |
>5 years |
|
E5 |
Male |
Chinese |
>5 years |
Table 1: Profile of the 25 participants.
Seven themes emerged as important for Joy in Living experiences of elderly to flourish in nursing homes: (i) ‘supportive nursing home environment and practices’ that includes adopting person-centred care, (ii) ‘meaningful daily living’, (iii) ‘connectedness through meaningful relationships’, (iv) ‘fulfil the need for spiritual care’, (v) ‘personal control’, (vi) ‘adapting to changes’ and (vii) ‘desire to be free from worries’. These themes include the enabling and disenabling conditions to Joy in Living in nursing homes and, are the common essences of participants lived experience in a nursing home, as narrated by them through reflection of their day-to-day personal experiences [27]. These themes, when enabled, promote Joy in Living experiences of the elderly residing in nursing homes as illustrated in figure 1. The themes and sub-themes are elaborated in table A1 in appendix A.
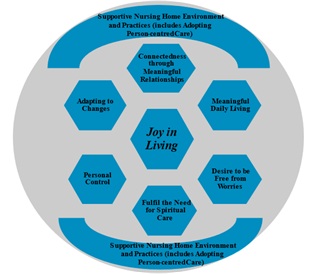 Figure 1: Themes for Joy in Living experiences in nursing homes.
Figure 1: Themes for Joy in Living experiences in nursing homes.
The hierarchy chart in figure 2 shows the frequency of reference to the themes, subthemes, and codes in the transcripts of the interview and the observation audio recordings in the NVivo software. The subthemes within each theme are as illustrated in the concept map in figure 3.
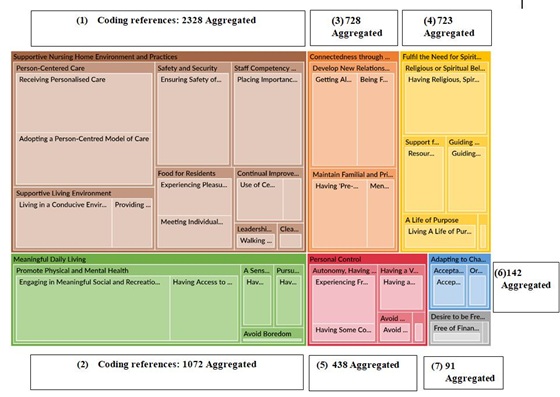 Figure 2: The hierarchy chart shows the frequency of reference to the themes, subthemes, and codes in the transcripts of the interview and the observation audio recordings.
Figure 2: The hierarchy chart shows the frequency of reference to the themes, subthemes, and codes in the transcripts of the interview and the observation audio recordings.
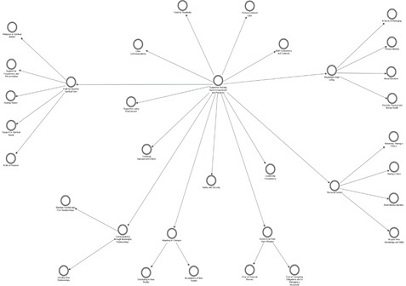 Figure 3: Concept map of the themes and sub-themes for Joy in Living experiences in nursing homes.
Figure 3: Concept map of the themes and sub-themes for Joy in Living experiences in nursing homes.
Results of theme 1 - Supportive nursing home environment and practices
The foundational theme that provides the conducive ecosystem for Joy in Living experiences to flourish is a ‘supportive nursing home environment and practices’, which include the adoption of Person-centred Care approaches such as the Person-centred Care Model or its variations in Person-directed Care or Eden Alternative Model. This ecosystem theme contains eight sub-themes, which are presented in descending order of coding frequency: (i) person-centered care; (ii) supportive living environment; (iii) safety and security; (iv) staff competency and capability; (v) food for residents; (vi) continual improvement efforts; (vii) leadership competency; and (viii) clear communications. The sub-themes address various aspects of the ‘supportive nursing home environment and practices’. This theme has the most coding references, as shown in figure 2 on the coding references in the NVivo software hierarchy chart. All participants emphasised the significance of at least one of the sub-themes in creating an environment conducive to Joy in Living experiences flourishing. This was also supported by the observational data.
Person-centred care
Person-centred Care’s psychosocial dimensions are covered in the following themes: ‘meaningful daily living’ and ‘connectedness through meaningful relationships’. This section discusses individualised nursing care for residents. Personalised nursing care for residents was observed in all five nursing homes, including grooming, medication administration, monitoring, assisted feeding, and support at group activities and exercises. However, staff engagement with residents is patchy across the five nursing homes and appears to be dependent on the personal qualities of the staff involved and their ability to communicate in vernacular languages: rather than a consistent practice across all staff interactions.
The Therapy Assistant is sitting next to her and stroking her hair. She speaks to the resident in a Chinese dialect. The Therapy Assistant, who is a local Chinese and a mature staff in either her late forties or fifties, smiles at me and says she is speaking to the resident in (1st Observation at Nursing Home A)
Staff who are assisting to feed the residents are patient and they encourage the residents to finish their dinner. Beyond this, staff do not engage in small talks with the residents. Their focus is on the task of feeding the residents safely. Staff 4 speaks to the residents in dialect and these residents interact and engage with her more when compared to residents assisted by foreign staff… Staff 3 is an Indian PR staff. She speaks Tamil and English. She engages the Indian residents by speaking to them in Tamil (Post-interview Observation at Nursing Home E)
A total of 20 out of 25 participants, or 80%, reported receiving personalised nursing care in the aforementioned areas. One resident expressed her confidence in the nursing home's care.
“Because I feel that I come here is suit for me. I got the thinking that somebody can look <after> me until old.” (B1, Length of Stay: 3-5 years, Female, Chinese)
Two residents expressed dissatisfaction with the personalised nursing care they received.
“Sometimes they neglect or extend the time for changing the diapers. It is not done correctly at the correct timing. They delay for 30 minutes, 40 minutes. Like this morning for example I tell you, my diaper was changed at 12.30 and now it is 5 o’clock. So, I have been wearing this for the last 7 hours or 6 and a half hours. It is quite uncomfortable you know.” (D1, Length of Stay: 3-5 years, Male, Indian)
“Sometimes they see you, I call to help me. They just walk away. Some say, “I don't know.” (E3, Length of Stay: 3-5 years, Female, Chinese)
According to the other three residents, because they are not wheelchair-bound, their nursing care needs are minimal: only medication and health monitoring. Showers being too short were mentioned in interviews with three participants from the last two nursing homes. The preliminary data collected from the first three nursing homes did not reveal this.
“The shower is too... too short you know. They... just... they should know that we are not happy about the shower. They should know by now…” (D1 Length of Stay: 3 - 5 years, Male, Indian)
“Because sometimes they shower me so quickly like that 10 minute like that quickly. Sometimes I put soap haven’t finish here they want to say okay, okay, finish, finish. How can like that? My body got soap some more how can.” (E1, Length of Stay: 3-5 years, Male, Indian)
Another insight that came up in interviews with four participants from the last two nursing homes (especially in Nursing Home D) was the over-reliance on use of adult diapers to assisted toileting. Adult diaper users reported no attempts by the nursing home to wean them off diaper use.
“At home, I go toilet. Here I wear pampers. Wear diapers, there are advantages and disadvantages. You wear pampers; you don’t need to walk to toilet. The disadvantage, there is no exercise. Life is like that, there are advantages and disadvantages. Like ten fingers, some short, some long, they are all not the same. There are advantage and disadvantage.” (D4, Length of Stay: 3-5 years, Female, Chinese)
“Even before I go to toilet, they already have diapers. And they tell you what for go to toilet, you are wearing diapers? To me no difference ‘lah’ <simplest and most common Singlish expression like ‘yeah mate’ in Australia>. Yeah, I say I use the diapers ‘lah’ like everybody. Because in the room there is only five of us, they say there is no need to tell, no need to tell us whether to go to toilet or not.” (E5, Length of Stay: >5 years, Male, Chinese)
During a post-interview observation session at Nursing Home E, one of the assistant nurse managers hinted that there is still room for improvement in this area of nursing care. She told the first author in an impromptu conversation that with the relaxation of COVID-19 safety protocols, which will free up staff time, the home will proactively identify residents who are ready to be weaned off diapers in the coming months.
Supportive living environment
A well-designed physical environment can ensure the elderly’s safety and independence in either the community or nursing homes, which has a positive impact on their well-being. Environmental aspects of supporting Person-centred Care delivery, conducting social and physical activities, and creating a home-like ambience must be considered when designing nursing home living spaces. In their pioneering work on the ecological model of ageing, Lawton and Nahemow [28] emphasised the importance of having physical spaces that fit the needs of the occupants for optimal functioning. Several studies over the last two decades have also emphasised the importance of physical environment accessibility on senior functioning [29-31].
The living environment was mentioned as an aspect of the nursing home that nine out of 25 participants, or slightly more than one-third of the participants, liked. One of them chose the nursing home based on her impressions of the living environment and amenities when she visited it before making a decision.
“…peaceful. I don’t how when I see the picture I know I want. My friend gave me the picture of the building. I went to other homes, but I cannot suit, then I see this I like. My sister also say better, this one also nice…They got proper place. All the sleeping place they have water, put water for drinking at hall.” (B1, Length of Stay: 3-5 years, Female, Chinese)
“I like the garden… I feel happy in my heart when I hear the water, birds and <see> fish swimming... I also pray there, give me joy.” (C6, Length of Stay: 3-5 years, Male, Malay)
Two residents expressed dissatisfaction with their living environment.
“This building is not properly maintained. It’s dirty. Look at all the fence, never clean. Compared to the old place, every week somebody will come clean all the fence.” (A4, Length of Stay: 1-2 years, Male, Chinese)
“…usually at night in the morning about 3 am the sleep is disturbed because, yeah, they’re changing. The staff is changing all the patients’ diapers because the diapers got too much urine and they are, it becomes soggy and wet. So, they start changing. So, when they start changing, there's quite a bit of noise… Dementia, and some of them are making noise at night. Some of them making noise at daytime, shouting at times.” (D1, Length of Stay: 3-5 years, Male, Indian)
At the second observation session at Nursing Home A, the first author encountered rodent infestation problem in one of the bedrooms during an impromptu conversation with a resident in his six-bedder ward. She saw a rat trap kept at the foot of the cupboard. The cupboard was not in a good condition. Rat infestation is a safety concern too.
“This is not as bad as the rats... I got a lot of things, so they say you cannot put on the floor and all that, so they gave but they gave one that’s broken <they gave him a cupboard>. And rats used to go in what from the back. Now they say they fix it.” (A5, Length of Stay: >5 years, Male, Chinese; during an Impromptu Conversation at the 2nd Observation Session at Nursing Home A)
The first author also observed a hygiene problem with birds flying in during mealtimes and in the wards of three nursing homes. These nursing homes are set in open garden compounds that are popular with birds. This is a concern because birds’ droppings can spread diseases. Staff is constantly on the lookout for birds and promptly clean up food waste and spills. The rest had nothing negative to say; however, seven participants, or slightly more than a quarter of them, wished for the temporary COVID-19 safe distancing measures to be lifted as soon as possible. The zoning has limited their access to the nursing home's entire compound and amenities, as well as group activities with other residents from different zones, volunteer-led activities, outings, and frequent visits from family and friends.
“Yeah. It’s downstairs. There’s a fishpond and everything. Before we used to go down every day. We’ll go down, see the fish, then we all cannot...Now cannot because the COVID-19. We are not supposed to go down, leave our dormitories.” (C5, Length of Stay: 3-5 years, Male, Indian)
“Last time ‘ah’ before this Covid, last time got drawing class ah, got singing ah, go down ‘ah’. Now all don't have, so quiet.” (D3, Length of Stay: 1-2 years, Female, Chinese).
Safety and security
Observation sessions were primarily used to identify safety and security practices. One caveat is that many of the observed safety practices are Covid-19 temporary safety measures in place during the observation data collection phase. Staff at all five nursing homes were observed following internal safety protocols when administering medication, supervising residents during group exercises or mealtimes, feeding special diets, and transferring residents from bed to wheelchair/geriatric chair and vice versa. In Nursing Homes A, B, C, and D, I observed that fall prevention is a key focus, and there is an over-reliance on the use of restraints on several elderly in beds, wheelchairs and geriatric chairs. Only Nursing Home E reported using restraints as a last resort, which was corroborated during the observation session.
“No restrain here, only hand mittens if they scratch themselves. But they move and follow us sometimes, look at the work nurses do. Keep them occupied, until they quiet. Sometimes, give them something to do to keep them occupied. But must ensure environment is safety.” (Impromptu Conversation with a staff at Post-interview Observation at Nursing Home E)
She asks the residents for their names, refers to a medical records ‘IMR’ folder with residents’ names and their laminated photographs, before giving the medicines. The medication trolley is a mobile cabinet with mini drawers. The mini drawers have names and photos of the residents. The medicines are kept in the mini drawers. (1st Observation at Nursing Home A)
A consistent practice in all the meal observations is having dedicated staff moving around and watching over residents who are eating on their own in both the living and dining rooms. Staff also go around with a pair of scissors to cut the vegetables and meat to smaller pieces for those who ask for assistance or look like they are struggling with their meals. (2nd Observation at Nursing Home B)
Four participants reported falls in the nursing home that fortunately did not result in bone fractures. Two participants reported falls by other residents: one of which resulted in the resident’s death.
“The other day one man died, he fell off the wheelchair and hit his head. This man, I predicted a long time ago. So, nurse ask me why you talk like that. I said if you look, he goes to the toilet 20 times. So, he’s putting himself in danger. You as nurses need to make sure he keeps safe; they don’t lock the wheelchair. I said I fall never mind, but when he falls and there’s nobody around. That’s the danger.” (A4, Length of Stay: 1-2 years, Male, Chinese)
Staff competency and capability
19 of the 25 participants, or slightly more than three-quarters reported both positive and negative experiences with various staff members. Negative experiences occurred as a result of staff lacking the necessary knowledge, soft skills, and language barrier (for foreign staff) to carry out their duties effectively. This was exacerbated further by staff workload and/or inadequate staffing.
“Some nurses are very observant. Some, not so... I speak frankly, sometimes they are very busy and some of them, they don’t bother.” (A4, Length of Stay: 1-2 years, Male, Chinese)
“A few is very good. They really do the job, they very follow the procedure. Like from bed transfer to this, they really take care of you. Some they just stand down there, like for my case I used to use slide board and slide to my wheelchair. Some stand behind look at you. Anytime I can miss out and I fell down. They just stand down there. Some really good ‘lah’ they take my two legs then I slide over very fast. One second. I think less than 20 seconds I go there already. Some they sit down there and slowly do. Some of the nurses they really use their heart to work, some they just are not really nice.” (A3, Length of Stay: 1-2 years, Male, Chinese)
“… like I said, a lot of staff cannot communicate, and different mentality… most of them are quite busy… So, they have to be more relaxed to be able to talk to us, at the same time, it is a balance that they cannot be too relaxed and not get things done.” (B4, Length of Stay: 1-2 years, Male, Chinese).
“Do long hours, they must also rest. Every morning come to work, can see the face look tired, not enough sleep... Yeah, yeah. They can look after us properly <if they are rested>. (E2, Length of Stay: 1-2 years, Female, Indian)
“There are some nurses, they didn’t do properly. Although they say they very good to me, but anyway, there are too many here didn’t do properly, say “wait, wait”, then wait very long didn’t do. So, if there are things I can do on my own, I do. Although they are friendly.” (E4, Length of Stay: >5 years, Male, Chinese)
Three of the participants expressed their dissatisfaction with staff turnover. One of them mentioned how he misses the staff who used to do his physiotherapy sessions but are no longer with the nursing home. Another resident reported frequent staff changes because of attrition.
“They got their problem about the work. How many people go out, already don’t work here.” (B1, Length of Stay: 3-5 years, Female, Chinese)
During two nursing home observation sessions, I observed daily shift handover meetings to share updates with the care team taking over. Staff at all five nursing homes were observed following internal protocols when carrying out their duties. For example, only nursing aides, enrolled nurses, and above feed pureed food to residents at risk of choking and do nasogastric tube feeding for bedbound residents. During one observation session at a nursing home, I observed that staff do not intervene to defuse sporadic arguments among residents. I struck up an impromptu conversation with another resident who had witnessed the incident.
“Some can, some they will leave them. Because ‘aiya’, I don’t want to say anything because it’s not good. Sometimes nurse and all got visitors, special visitors, if no visitors, then you can see shouting.” (Impromptu Conversation during 2nd Observation Session at Nursing Home C)
Observation data were collected in the last two nursing homes when COVID-19 measures were significantly eased. During one of these post-interview observation sessions, a senior nursing staff member shared that the increased workload of the nursing team from implementing COVID-19 safety protocols had left little time for the nursing department to work on improvement projects over the last two years. She believes that with the relaxation of COVID-19 measures, there will be more room to strengthen core nursing practices and implement progressive ones.
“During these 2 years with Covid, we are very constrained. So, frankly speaking, we also need to tighten our nursing care. A lot of staff is down with Covid, isolated, we are very short. So certain things we are neglect, so it is a lack. Now slowly we must ‘die die’ <Singlish phrase that it is a must have even if you have to die for it> even if like war zone like that. Our environment, we are very keen in learning, but just open only our lockdown and busy with the NOK visits. We have this programme but somehow just dropped, so must pick up now. Some of our residents are mobile and shouldn’t need to wear diapers. We should encourage them to wean off.” (Impromptu Conversation with an Assistant Nurse Manager at Post-interview Observation at Nursing Home E)
Food for residents
There is a wealth of literature on nutrition for the elderly in hospital and nursing home settings, with a focus on the risks of malnutrition and the causes of decreased appetite in the elderly [32-35]. There is, however, less literature and research on the association of food with memories in the elderly. It is not uncommon for someone to eat food at a party and be transported back to a pleasant or unpleasant memory associated with that particular dish eaten in the past. Chinnakkaruppan et al., [36] conducted an intriguing neurological study on laboratory mice and discovered a link between the brain regions responsible for taste memory and remembering the time and location when the taste was experienced. In addition to this individualised preference and enjoyment of food, elderly people from various ethnic communities have different palates shaped by their cultural heritage and unique dietary restrictions such as consuming only halal or vegetarian meals or being vegetarian on certain days of the week. Because of food allergies and dietary restrictions, some elderly people may need to avoid certain foods.
12 of the 25 participants, or approximately 50%, complained about the quality of the food or food served that did not meet their dietary preferences.
“The Chinese one cancelled already. Sometimes got babi <pork>, don’t want. “Now, Malay food. Sometimes can, sometimes cannot. I mean, last time one, the Tuesday 'ah', the Muslim food, they give me chicken. I vegetarian Tuesday and Friday. Eat rice and vegetable only. Last time I like, one staff Indian cook ‘resam’ <a spicy Indian soup dish>, curry in kitchen give me. Missy <nurse> say cannot, my sugar, eat food they give, cannot special.” (A1, Length of Stay: 3-5 years, Female, Indian)
“But I like meat, not fish. When I’m outside I always want some meat. When I’m here I got no choice.” (A2, Length of Stay: 1-2 years, Male, Chinese)
“Not quite like. Chinese food or any food must be hot. Cold, cold <now>”. (D3, Length of Stay: - 1-2 years, Female, Chinese)
Sometimes the food is very tasty. But sometimes, I don't know why the xxx nursing home give me like this kind of food, I don't like. Yeah, I think the meat I must say all, certain meat, I like pork but too hard. And then sometimes, some food, the rice all hard then I eat potato to help me substitute the rice. Difficult to chew, difficult to bite. The chicken also no taste, hard to bite. (E4, Length of Stay: >5 years, Male, Chinese)
Two participants expressed dissatisfaction with the amount of food served. When I asked if they had asked for a second helping, one participant said he was embarrassed to ask “Shame”, and the other said staff would be upset if she used the call bell unnecessarily to request more breakfast.
Four participants reported being “okay with the food” or having “no complaints”, with one participant sharing that, in addition to being okay with the food, he is grateful to God for the food received. Two participants made no remarks about the food. Five participants stated that the food is good and that they enjoy it.
“We all have ‘uh’, three, three meals a day. So that's enough for us what. I don't need much”. (D2, Length of Stay: 3-5 years, Male, Chinese)
“<Mee Tai Mak - a Chinese dish> Too watery; when I eat the water all come out. I like they fry here… Pork. Mostly is pork. Chicken also give. Fish is very good, there is no bone, else we have to be careful of the bone.” (D4, Length of Stay: 3-5 years, Female, Chinese).
Continual improvement efforts
All five nursing homes were found to have implemented centralised services such as central kitchens for in-house meal preparation and a central laundry service for all wards. Nursing Homes A and D have implemented technologies such as an automated guided vehicle (i.e., an autonomous robot) for food delivery, while Nursing Home C cleans the dining hall floors with an automated steam machine. To increase staff productivity and protect them from back injuries, Nursing Home E uses a ceiling hoist to transfer bedbound residents to bath trolleys for showers.
Nursing Home E also employs technology to improve the service delivery experience for its residents, such as the use of an ambulatory hoist and forearm rollator for wheelchair-bound residents' walking exercises and specially designed ‘Gym Tonic’ low-intensity strength training exercise equipment for residents’ use. During an observation session at Nursing Home A, I observed an innovative programme for dementia residents called ‘Mini Mart’ in one of their residential living areas. Residents earn fake money by participating in exercise activities, which they can then use to redeem snacks like potato chips and cup noodles on their ‘shopping trip’ to a ‘mini-mart’. Residents must count the counterfeit money and coins to pay the exact amount indicated on the food items displayed on the shelves in the ‘mini mart’ room. The ‘mini mart’ room is styled after a supermarket.
I observed a group of ten residents, each with a ‘maracas’ musical instrument, exercising, singing along, and shaking their ‘maracas’ to music videos being played on TV during an observation session at Nursing Home E. Residents are rewarded with a fake currency that they can keep in their wallets and use to ‘buy’ snacks and other grooming necessities at fun fairs/‘Bazaars’ (which have now become mobile ‘Bazaars’ because of COVID-19 safety measures). Playing online digital games on tablets, playing ‘Bingo’, and learning to play the keyboard are all examples of ‘Hope Kee’ activities.
Leadership competency
Positive leadership role modelling was observed at Nursing Homes B and E and gleaned from impromptu conversations at Nursing Homes A and D.
At the briefing at the female ward, staff nurse informed the Chief Executive (CE) that there was a new resident who was a little unhappy and having adjustment problem. CE walks over to the ward to speak to the new resident. CE returns shortly after her chat with the new resident. Apparently, according to the home protocol, the resident needs to be isolated for seven days before she can mingle with the rest of the residents at the common areas. She is bored. CE asks staff to give her an iPad to let her watch whatever shows she wishes to watch. A staff quickly follows up on this. (1st Observation at Nursing Home B)
“I know about this one <referring to the vacancy at Nursing Home A> because of the certificate course that * xxx <CE> teach. The trainer is xxx <CE> herself…Yeah, she trains us hopefully we’ll join this company but not all will join ‘lah’.” (Impromptu Conversation at 2nd Observation at Nursing Home A)
* To protect the identity of CE, name of CE is replaced with xxx
After updating on residents’ progress, the Assistant Nurse Manager briefs all present on AIC <Agency for Integrated Care> project updates on wound management and enabling identified residents to wean off diaper use. Project team members take turns to provide updates on the progress of their projects and next steps planned. The Assistant Nurse Manager wrapped up the meeting by asking staff for feedback. Overall, there is good interaction and participation from staff present. (Post-interview Observation at Nursing Home E)
Two residents expressed satisfaction with management’s support for feedback and gathering residents’ wishes beyond daily nursing needs to include preferred funeral arrangements.
“Some more the management is a support me. Support by need anything they are going to help me. Because they interview me. Sometimes they got interview me. They ask anything, anything I want. Then I tell them, I want this, I want that.” (E1, Length of Stay: 3-5 years, Male, Indian)
Five residents, or 20% of the residents expressed strong opinions that management does not provide direction and leadership for the organisation and its staff.
“…the food, all you need to do is to get somebody to do quality control. You’re paying for the food …But if you don’t bother about it, they will just give you the same and this is exactly what is happening.” (A5, Length of Stay: >5 years, Male, Chinese)
“They understand, most of the nurses very intelligent. They understand, the only thing is they got no power to say must have this, the patient must have that.” (D3, Length of Stay - 1-2 years, Female, Chinese, a former nurse)
“They don’t agree ‘lah’ <for a slightly longer shower>. I think it’s the boss’s idea. Yeah. Because they have to get back to work.” (E5, Length of Stay: >5 years, Male, Chinese)
The study did not include any staff interviews or focus groups. However, during an impromptu conversation with a staff member during an observation session, the staff member alluded to a culture in which staff are not encouraged to express their opinions and provide feedback for improvement.
Observer:
“Have you given this feedback to the management?”
Staff:
“I’m not sure cos I just joined here. But I don’t like to highlight, this is not my portfolio I mean the <*xxx designation> is the lowest level here. Because we cannot understand that, we cannot do.” ( Impromptu Conversation at (2nd Observation at Nursing Home A)
*To protect the identity of staff and organisation, designation is replaced with xxx
Clear communications
There appears to be miscommunication and misunderstanding of COVID-19 restrictions on next-of-kin visits and certain nursing home policies based on the sharing of seven participants at interviews, i.e., slightly more than a quarter of them, and an impromptu conversation at an observation session.
Resident:
“How long, when can I see family? When allow from MOH side?”
Observer:
“I think soon because it’s been too long already. The government intends to allow visits to hospitals and nursing homes from 21st Nov onwards. This is what is announced in the newspapers and TV news.” The resident is relieved to hear this. (Impromptu Conversation during (2nd Observation at Nursing Home C)
“I think have <books, magazines> but I never know that there is got newspaper. Hospital have <communications gap as resident is unaware whether newspapers are available>. (D3, Length of Stay: - 1-2 years, Female, Chinese)
“What can I do <when asked if there are opportunities for her to volunteer her services>? So many people work here, I do what, right?” (E3, Length of Stay: 3-5 years, Female, Chinese; from the post-interview observation session, it was observed that there are opportunities for residents to volunteer in the home. It is likely a communication gap as resident is unaware)
Two previous incarcerated residents shared that the nursing home does not allow visitors; only family members are permitted to visit them. This is not the lived experience of other nursing home residents who have reported having friends visit them. This could be a request made to the nursing home by family members to prevent access to friends from their ‘shady’ pasts.
“Have a friend but they never come and visit me. The Nursing Home E no allow, not allowed to visit me, anybody. Nobody can visit me. Except my brother and sister-in-law. Because the Nursing Home E is a very strict place. Yeah. Correct <covid restrictions>. Second thing Nursing Home E, they got some law here. Sometimes they <his friends> not allowed to see me. Other residents I don’t know. But the law is same. Same law. Everybody. Not just for me.” (E1, Length of Stay: 3-5 years, Male, Indian)
Two residents stated that they were aware of the COVID-19 restrictions and their implications.
“Yeah, of course. Only now only cannot. Now, there are some restrictions. I just cannot move around, and food is definitely not allowed. Before no problem, I am allowed to bring food, but not now.” (D2, Length of Stay: 3-5 years, Male, Chinese)
Results of theme 2 - Meaningful daily living
Participation in social and group recreational activities for seniors has been shown in studies to facilitate the development of new relationships, keep them meaningfully engaged, and promote physical and mental health [12,18,19,37].
Promote physical and mental health
The vast majority of participants, 20 out of 25 (or 80%), reported that there were very few meaningful activities in nursing homes other than structured physical and occupational therapy exercises for residents.
“I go swimming you know. Here in the home.” (A1, Length of Stay: 3–5 years, Female, Indian)
“I do join the group exercise. It is good for my strength. I like the individual therapy better.” (A4, Length of Stay: 1-2 years, Male, Chinese)
The activities include stacking and rearranging cups, identifying matching items in 3-d game sets, completing jigsaw puzzles and colouring pre-printed drawings. One staff… walks around and supervises the residents…. For selected residents, he works on the range of motion of their upper limbs: the arm, forearm, and hands, while they are working on their assigned tasks. (1st Observation at Nursing Home C)
Nursing Home E is home to four of the five participants who reported meaningful activities organised for them (including opportunities to volunteer their services). This was also supported by the Nursing Home E observation data.
“Play carrom, uno, card, got so many ‘lah’ I forget. We start after drink coffee already 2 o’clock. Dinner time is four o'clock. Before dinner, ten minute, half hour like that we stop ‘lah’, 3.45 like that… Here got the cloth folding all I like… Here, okay ‘lah’ they all close that's why I say fold the cloth, fold plastic bag, game also passing time. So never think the family, missing them, rest the mind. And give coloring they give picture, I get first prize.” (E2, Length of Stay: 1-2 years, Female, Indian)
“Okay. I'm happy, I am happy with all the things here. As you can see, I like ‘Hope Kee’ very much… singing, sing songs, I like to sing, then after exercise, they play game. Then after everything over okay, playing each one get two dollar. We got many currency…through the fun fair they give us fun fair we buy things use the xxx <name of the nursing home> currency. Then the money whatever we want from whatever we have, they let us buy.” (E4, Length of Stay: >5 years, Male, Chinese)
Many residents spend a significant amount of time sleeping or watching television. Those who are fluent in English and Mandarin have limited access to newspapers in these two languages. Residents who can read Malay or Tamil do not have access to newspapers in those languages. Two Nursing Home D residents expressed their regret that the nursing home no longer provided them with English and Mandarin newspapers. One resident whose length of stay is within 3-5year timeframe in the nursing home spoke about not having his reading glasses with him as he left it in his home. Two residents shared that they are unable to read or watch TV due to poor eyesight.
For most of the residents, except for Nursing Homes D and E, the first author observed that staff bring them, including several bedbound residents in geriatric chairs, to the common dining hall for lunch and dinner. Most of the residents at Nursing Home D receive their meals at their bedside/in bed. Nursing Home E has a cluster-style family unit concept, with each family unit having a living room. Each family unit has about ten residents, and they are encouraged to eat together as a family in the living room. There are group exercises or occupational therapy activities in small groups following the COVID-19 restrictions on the number of people in group activities.
Sense of belonging
Residents who feel connected to the nursing home and volunteer their services are meaningfully occupied and experience Joy in Living. 4 out of 25 participants, or less than 20%, reported volunteering their services in the nursing home. During two observation sessions at Nursing Home C, six male residents were observed assisting with nursing home tasks such as folding washed laundry, towels, and unused trash bags. During an observation session at Nursing Home B, a staff member mentioned a female resident who assists them with tasks such as drying medicine cups and encouraging fellow residents to take their medication. A male resident was observed folding washed laundry and towels during a post-interview observation session at Nursing Home E.
“I can pour water for the plants.,. So, if you have a sincere heart, pour water for the plant…Because I came into this place; and I thank God.” (C5, Length of Stay: 3-5 years, Male, Indian)
A male Chinese resident sitting nearby is busy folding plastic trash bags. He is the only one doing this.
Observer:
“Why are you folding the trash bags?”
Resident:
“I like to do. I like work, not boring.” (Impromptu Conversation during (2nd Observation at Nursing Home C)
“Then I see so boring ‘ah’ if sitting down. Last time, cooking washing, sweeping all everything do, come here nothing to do, sit down 'makan' <eat food> only. Then I say, “auntie I help you”. She say, she say “your wish, can, can” …. I fold plastic, then cloth, our ‘makan’ cloth, towel all wash and come, then the next room auntie also fold the towels… Here got the cloth folding all I like.” (E2, Length of Stay: 1 to 2 years, Female, Indian)
Pursue interest
Meaningful daily activities organised by nursing homes, combined with time to pursue personal interests, contribute to the elderly residents’ Joy in Living experiences.
“Then the rest of the time I read, I got a lot of books there, and I play ‘Sudoku’ <number game>. You will be surprised.” (A5, Length of Stay: >years, Male, Chinese)
“Because I came into this place, I study more and more <the bible>, I pray every day…cos now I stay in this home even if I don’t go out is a heaven to me.” (C5, Length of Stay: 3-5 years, Male, Indian)
Avoid boredom
Loneliness and boredom can result from a lack of meaningful social and recreational activities. Five residents, or 20% of the participants, reported feeling bored because of a lack of evening and weekend activities.
“Down here, cannot, nothing. By 5 o’clock I call it a day. I just lie down.” (A2, Length of Stay: 1-2 years, Male, Chinese)
“Yeah, one thing got no night activity like karaoke room. All these very bored ‘lah’ stay here. Everyday don't know what to do. Luckily, I got my own phone. I can see the ‘YouTube’. At nighttime, if you cannot sleep I tell you, you don't know what to do. Every night, middle of the night wake up at least three times. Wake up, why haven't morning yet? Lie down I thought what three, four hours of sleep, wake up ‘wah’ <Singlish expression to profess surprise or shock, like the expression ‘Oh my God!’> one hour only. The more you think about it, you cannot sleep at all.” (A3, Length of Stay: 1-2 years, Male, Chinese)
“Now, down here, there is not much activity. And then we are sort of restricted living here… My closest thing is a newspaper and the television… Plan all these activities that I can participate, I find that it’s very interesting. Because I don’t like to be bored you see. Anything that I can do I like to do. I’m not particular.” (C3. Length of Stay: 1-2 years, Male, Chinese)
“Sleeping ‘lah’ <In the afternoon>. Before, yes, but now because of all these uh, censorship of everything <Covid restrictions>. They don’t do anything else <referring to activities like painting, art and craft etc.>.” (D2, Length of Stay: 3-5 years, Male, Chinese)
“We watch TV. Very very very tired. Nothing to do.” (D3, Length of Stay: 1-2 years, Female, Chinese)
“Nothing. I lie in the bed, daydreaming <in the afternoon>.” (D4, Length of Stay: 3-5 years, Female, Chinese)
There are activities planned in Mandarin for the Chinese ethnic majority residents. During a weekday afternoon observation session, I observed a 1.5-hour online ‘Zoom’ singing session in Mandarin organised by church volunteers at Nursing Home A. When I asked an ethnic minority resident from Nursing Home A if there were such online volunteer activities regularly, she replied,
“Tamil don’t have.” (A1, Length of Stay: 3–5 years, Female, Indian)
D1 and E2, both members of an ethnic minority community, reported that having a personal tablet issued upon admission and access to more TV sets in the family units' living rooms, respectively, allows them to watch TV programmes of interest and in their vernacular language. Loneliness is exacerbated by the limited interactions between residents and their family members, friends, and volunteers because of COVID-19 safety measures that restrict and, at times, prohibit visits or outings for extended periods when COVID-19 community cases increase.
“That time was a group of Christians. They come Sunday then they will pray for you, they sing song, worshipping. Then a lot of activities cancelled because of Covid.” (A3, Length of Stay: 1-2 years, Male, Chinese)
“<Resident’s wish for volunteer visits to resume> Make me happy. Not lonely.” (C1, Length of Stay: >5 years, Male, Chinese)
“Now cannot go out much. First time when I first come here, we one week will all go walk the gardens. Outside go somewhere the gardens. Sometime go eat outside.” (E3, Length of Stay: 3-5 years, Female, Chinese)
Three residents reported that their lives in the nursing home were less lonely than their lives in the community. Because of his debilitating illness, one resident was cut off from external social networks before moving to the nursing home. Because of their limited mobility, the other two residents were confined to their homes. There are a few staff members with whom they can converse at the nursing home.
“I got more people to talk to… More of the staff… They have interesting hobbies and interests that I can talk to them.” (B4, Length of Stay: 1-2 years, Male, Chinese)
“I like ‘ah’ <Singlish expression to express something is already known in a sentence>, to meet many people, have many friends. Talking to each other like friends. Friends with the residents and staff. At home, I am very dull, just my sister. I don’t have friends at home.” (D4, Length of Stay: 3-5 years, Female, Chinese)
Connectedness through meaningful relationships
Several studies on the well-being of seniors have emphasised the importance of developing new relationships as well as maintaining prior personal relationships to be socially included [12,17-19,38].
Results Of Theme 3 - Connectedness Through Meaningful Relationships
All twenty-five participants emphasised the value of establishing new relationships with caregivers and other residents, as well as maintaining existing ones with family and friends to enhance their experiences of Joy in Living.
Develop new relationships
Language barriers are one obstacle to forging new relationships with foreign caregivers.
“Here, you get to meet with them often and get to know them closely... But generally, it probably is a lot of them is from other countries like Myanmar that they can’t talk and understand English well <referring to foreign staff>.” (B4, Length of Stay: 1-2 years, Male, Chinese)
“Another reason which I'm pretty quite reluctant to tell you is that some of the staff they're not very well versed in talking to me in English... Foreigners like Myanmar... Even, even the Indian staff. When they speak English, it’s a bit different from our Singaporean English.” (D1, Length of Stay: 3-5 years, Male, Indian)
One resident talked about how she finds it difficult to build new relationships with caregivers and other residents because she fears being misunderstood and being the target of gossip.
“Because sometimes you talk the words can become, cause problems with other resident, even staff, I don’t talk so much.” (B1, Length of Stay: 3-5 years, Female, Chinese)
Another resident expressed his mistaken belief that staff members shouldn't engage in conversation with residents. This may have been influenced in part by his time spent behind bars in drug treatment facilities from his adulthood to middle age.
“Actually staff, they are not supposed to chit chat with us all. Cos this is a government place.” (C5, Length of Stay: 3-5 years, Male, Indian)
11 out of 25 participants, or over 40% of the participants, mentioned additional difficulties in building relationships with care staff, including staff displeasure at having to perform tasks like cleaning soiled diapers of elderly residents and/or staff fatigue from having to look after all residents.
“Their temperament is bad. Because other things, certain things you cannot complain. You ‘pangsai’ <pass motion> they want to wash you up, is very good. I think most of them are annoyed because of the washing up, they have to wash our backside or shower us, and they’re not happy with that... They talk among themselves and show their face.” (B3, Length of Stay: 3-5 years, Male, Chinese)
“I don’t want to trouble them, all busy. All okay ‘lah’ here. I just watch TV ‘lah’. They put me to sit facing the TV with Chinese shows. Chinese TV also watch.” (C6, Length of Stay: 3-5 years, Male, Malay)
“Not convenient for them if you ask them, they are busy.” (D4, Length of Stay: 3-5 years, Female, Chinese)
“Oh, here got 60 over <residents>. I think so, I not very sure. So many people cannot do any much. I my own also not clever.” (E3, Length of Stay: 3-5 years, Female, Chinese)
A little less than half of the participants-12 out of 25-reported having friendships with care personnel.
“Actually, the staff are quite good. I mean quite good to the residents. They don’t shout around or bully them. They are very gentle to them and always attend to their requests. …Yeah, we get along quite well. I trust them. Nothing very personal.... Just the daily needs and all that. One or two only that are willing to buy for me. Close to me.” (C3, Length of Stay: 1-2 years, Male, Chinese)
“All the nurse(s) are very good... Sometime I talk phone to my daughter, my family. I never talk about family story with the nurse, but they know because they know my daughter come here, children come here.” (E2, Length of Stay: 1-2 years, Female, Indian)
In all five nursing homes, the first author noticed that most staff members were more concerned with getting things done quickly and making sure residents were safe than getting to know them. Several foreign employees in all five nursing homes were shown to be able to communicate with the residents in a few words in Mandarin and Malay. However, this was mostly done to give them orders rather than have a conversation with them.
While the staff is courteous and patient, there is no interaction beyond the task of feeding them safely without choking…The interaction is mechanical. Although the staff uses a few words of Malay, it is mainly to ask what colours the resident wants from the colour pencil set. (2nd Observation at Nursing Home A)
On the other hand, mid-career local hires who assist with non-nursing care and organise social and recreational events can interact and have dialogues with residents in vernacular languages, as explained in section 5.2 on ‘Person-centred Care’.
The situation is worse when it comes to making acquaintances with other residents. Only ten out of the 25 participants, or 40%, claimed to have friends among the inhabitants. Most of the residents face challenges with forging friendships with others, including those from other ethnic communities and the dominant Chinese ethnic population who speak Mandarin and other dialects, include both sexes and have a variety of educational backgrounds.
There are difficulties, including language problems and being on a separate wavelength to others while making acquaintances with people, especially for residents from ethnic minority groups.
“…the residents. They are Chinese educated. The TV is in Mandarin the whole time. Day and night, they want Chinese... So, I hardly have anybody to talk to. I only talk to one…, I’m the bystander, I don’t care. I don’t care but I don’t like it. I mean it’s wrong to scold somebody, somebody’s mother or things like that. What has somebody's mother done to you? People's mother already die. What are you gonna do? But these are the kind of things that these Chinese educated are saying. Truly the nursing home should have educated people, not like all these Chinese educated ‘Jepalang’ <motley crew> cases” (A2, Length of Stay: 1-2 years, Male, Chinese)
“I don't talk to residents here. There's nobody here that I can really talk to. Because the things that I like to talk about would not be things that they would understand or be interested in. We don’t share common interests. Okay, but if you ask them to talk then they use vulgar language at all. I'm not used to using that kind of language.” (A5, Length of Stay: >5 years, Male, Chinese)
“Not like close friends, just say hi… Matter of interest <different interests>. I like to do things that will help me to improve.” (B4, Length of Stay: 1-2 years, Male, Chinese)
“Friend, but they never talk. All Chinese. I don’t know Chinese. I speak Malay, English. I Eurasian.” (B5, Length of Stay: 3-5 years, Male, Eurasian)
“Ah, wow. None of them. No friends. No friends…. Most of them are Mandarin speakers. For example, the one man in front of me and beside me. They're all Mandarin speakers. They can speak one or two, maybe 10 or 20 words, but there's no possibility of communicating.” (D1, Length of Stay: 3-5 years, Male, Indian)
“Yeah, we talk but normally I not very close much. Because I know which, which people are the same. I don’t like in my heart thing to talk to people… Oh yeah, yeah. Hokkien, Teochew, Cantonese, Mandarin, Malay. That’s all. I can talk, maybe deep thing I don't know, maybe ‘ah’… Yes, yes, not much the inside thing...”. (E3, Length of Stay: 3 - 5 years, Female, Chinese)
A member of an ethnic minority community claimed to have experienced racial prejudice.
“I like to join them, but sometimes their character is not good, I don’t want to join. Resident ‘ah’ some resident here very rude, very you know the ‘color-mind’. The skin. Yeah, the old timers here like that old already, the young ‘ah’ now no nothing <referring to the younger generation>. The old ‘ah’ last time people like that <referring to the older generation>, see ‘color’ one. They don’t want to talk; they talk to each other, you know? Then we just sit down like stone. Better we stay in bed 'ah', I don't want to join.” (E1, Length of Stay: 3-5 years, Male, Indian)
Ethnic minority participants who live with other residents who can speak their native tongue are among those who said they had friends in the nursing home.
“Everybody talk to me. One, if he got some extra food, he will always give to me. He give me biscuit. He cannot see well. He is a Malay.” (C6, Length of Stay: 3-5 years, Male, Malay).
“Like me one auntie, like my sister ‘lah’. My friend. She stroke or what, cannot walk. My room only. One year after me only then she come. She got three children, no husband. Husband pass away already. We all talk family story. Talk about me, talk about her <she is Indian, and they speak in Tamil>.” (E2, Length of Stay: 1-2 years, Female, Indian)
Maintain familial and prior relationships
According to the Continuity Theory [39], sensations of Joy in Living can grow when there are opportunities to sustain current relationships for the continuity of prior roles.
“My birthday. My lawyer <friend> will come. Every year he will buy a big cake for me and for the residents... Good friend in the case that I have my friends who bring me stuff. I give them a call.” (A4, Length of Stay: 1-2 years, Male, Chinese)
“My two sons here, I would say they’re very good. This is why I’m blessed. I think among all the residents here, I’m the luckiest… I got a lot of things to talk to them. You know I see a lot of them when the children come, just leave the food and not spend time talking to them. “Okay Pa, then they go out.” So, it’s a very short visit. They just come with some food and all that. The impression I get is as if they come because they are obligated to. My son can sit here for hours… Because there’s so many things, I can talk with them.” (A5, Length of Stay: >5 years, Male, Chinese)
On the other hand, the residents experienced a great deal of anxiety and grief because of the absence of possibilities to address concerns relating to family members’ unilateral decision to place them in a nursing home, bequest, and/or reconcile damaged relationships.
“I want to go outside to eat. I feel homesick. I hope my brother will discharge me. I asked him. He said no. No one to look after you unless you can start walking.” (D4, Length of Stay: 3-5 years, Female, Chinese)
“Morning, morning I cry already. My house. The last one boy, he say, “I want my father house”, he say… My number 1 daughter, her husband say the house sell and then CPF take the money, they give you. You stay in home here… I mean, the boy he don’t like. He want house. I give house to him. I sell already, the boy where go? I stay ‘sini’ <here in Malay>, where the boy go, where?” (A1, Length of stay: 3-5 years)
“That is what people say. What people do is different. Well, I don’t know why they think this way. I always look after the family. I’ve never been disloyal. When I go back to my home in Melbourne, I’m afraid I don’t know how to say why are you this way. I’ve done nothing wrong. You’ve done wrong with me… My family never contact me.” (A4, Length of Stay: 1-2 years, Male, Chinese)
More than half of the participants-13 out of 25 residents-reported having troubled family relationships. Proxies for poor relationships include few or nonexistent calls or visits from family members, venting about being put in a nursing home by their family, bequest disputes, and abandoned or estranged family relationships. The other individuals enjoy supportive or positive relationships with their families. During an observation session, a senior member of the nursing staff casually mentioned that many of the home's residents didn't have a lot of family support.
“I think that family support also plays a big role, but unfortunately here, family is not so supportive. Very few percentage have family support.” (Impromptu Conversation with Assistant Nurse Manager 1 at Post-interview Observation at Nursing Home E)
Fulfil the need for spiritual care
Three Freethinkers (those who accept the concept of a superior being like God or deities but form opinions and think independently of any religious dogmas), one Atheist, and participants who belong to the major religious traditions of Singapore's population (Buddhism, Taoism, Christianity, Islam and Hinduism) are represented in this theme. Despite the variety of religious and spiritual convictions, two common sub-themes emerged: (i) the use of one's religious or spiritual beliefs as a compass while facing life’s difficulties; and (ii) the provision of support for individual spiritual needs. A life of purpose and guiding values emerged as two other sub-themes. The intra-connection a person has with themselves in terms of values, meaning, and purpose in life, as well as the relationship with God or the cosmos, are two of the four domains of the Spiritual Well-being Model [40,41]. The Environmental Domain of the Spiritual Well-being Model emphasises connection and harmony with nature, having a deep sense of calm and being in awe of its beauty when spending time in nature (strolls in the park, forest treks, etc), and the Communal Domain emphasises one's relationships with others (covered in theme 3). New information regarding the necessity of assisting the elderly in seeking forgiveness, reconciliation, and letting go of the weight of regret surfaced during the coding and analysis of the data from the last two nursing homes. In Erik Erikson’s eighth stage of human development, ‘Integrity vs Despair’, the urge to forgive oneself and work toward reconciliation is a crucial final psychological stage that takes place in old age [16]. Support for forgiveness and reconciliation is the new fifth sub-theme.
Results of theme 4 - Fulfil the need for spiritual care
Religious or spiritual beliefs
There are both good and bad religious coping mechanisms [42]. When someone practices positive religious coping, they experience a strong spiritual connection with their family, friends, and the larger community and are generous in giving and kind to others. A little over 70% of the participants, or 18 out of 25 participants, reported adopting positive religious coping mechanisms to varying extent, which were evident in their positive attitudes toward their lives and a feeling of meaning and purpose in their daily activities.
“I pray every day in the room. My heart I pray, chant. I pray in the morning, before breakfast. I don’t have a wicked heart. I don’t hurt people. I think nothing wrong. If you do something evil maybe you scared…I believe that if there is no God, we cannot come to this world. There is a God then you come to this world… Whatever the world is given we take. You make good karma, so you can get good things. Good karma is a blessing… I believe that whatever I want, God give me, that one I believe.” (B1, Length of Stay; 3-5 years, Female, Chinese)
“I cannot kneel on floor. I sit in the wheelchair and always praying in my heart, always praying in my heart the Quran. Anytime I pray… Give me joy pray Allah… Pray Allah really make me healthy. Bless family with health and money.” (C6, Length of Stay: 3-5 years, Male, Malay)
“I pray to God my leg don’t cramp too often. I ask God to give me strength to bear the pain. The only problem give me is my leg now. Last time my leg seldom cramp. Now everyday cramp.” (D4, Length of Stay: 3-5 years, Female, Chinese)
“In fact, at all times. Sometimes when I shower, I was eating, I was doing my things whatever thing, I have been like in prayer mood, deep in tune with God… I believe that after I die, I will go be with the Lord, go to be with Jesus, Jesus will bring me to heaven.” (E4, Length of Stay: >5 years, Male, Chinese)
Nine individuals, or just over one-third of the group, keep mementos of their religion or a copy of their holy book nearby and pray before going to sleep.
“Got the photo God, I put on top small cabinet near my bed and I pray. All God photo, ‘Vinayagar’, ‘Lord Shiva’ <Hindu deities>, got ‘ah’, pray. I Hindu must pray in the morning after bathing... Before I sleep, I pray.” (A1, Length of Stay: 3-5 years, Female, Indian)
The remaining residents who practice a religion said prayers from memory because they forgot to bring their holy books to the nursing home.
“In my heart. What I can remember, I just read from my heart.” (C6, Length of Stay: 3-5 years, Male, Malay)
“Nobody, nobody knows that I bookless <prayer book>. I wanted to call my nephew to bring for me, he always says he got no time.” (D3, Length of Stay – 1- 2 years, Female, Chinese)
Two Hindu individuals who do not maintain religious symbols by their bedsides either decided not to or misplaced the picture.
“… can keep but I don’t want, don’t know why... I don’t want, I never ask before. I don’t like, don’t know why.” (E1, Length of Stay: 3-5 years, Male, Indian)
“The other nursing home I keep small one; can keep in our purse the small one. Now don’t know go where. After operation, all lost already.” (E2, Length of Stay: 1-2 years, Female, Indian)
Two out of the 25 participants said they had prayed in the nursing homes' gardens.
“…more cooling outside, a lot of leaves. I like to look at the leaves, green leaves all these... I just concentrate, close my eyes for one minute. Then I pray ah, just pray. Enjoy praying.” (A3, Length of Stay: 1-2 years, Male, Chinese)
Internal conflict involving one's relationship with oneself, others, and God is a sign of negative religious coping. According to research, negative religious coping can lead to excessive guilt, poor health, and even mortality [42].
Three out of the 25 participants, or just over 10% of the group, admitted to having trouble with unhealthy religious coping.
“… never go to church after my father die when I young… Yeah, baptised. One day go to church after my father die. When young, If I never go, my father beat us go to church. My mother never beat. My dad beat… I don’t know. I never go to church. I ‘devil’. It is written. Written that I do plenty sin. Drink beer...go hell.” (B5, Length of Stay: 3-5 years, Male, Eurasian)
One of the three participants is torn between his commitment to two different religious traditions, and which one will enable him to regain his ability to walk.
“I believe now got two religions inside my body, one Jesus Christ and amulets ‘lah’… See now, when I pray, I want to concentrate more on Jesus. Even the amulet do come and disturb me, I just don’t want to think… For those Thai amulets, they do have this type of amulet to heal. Heal the sickness. … All similar, basically all the same: don’t cheat people, don’t kill people, don’t do bad things, all the same thing but how come for Christian they say all these is not real, this is all demon. But it’s true ‘lah’ those amulets, when I wear that time, I feel very happy, I feel very safe. (A3, Length of Stay: 1-2 years, Male, Chinese)
One Freethinker and the atheist, out of the three Freethinkers and the atheist, do not use religious coping mechanisms to find meaning and purpose in their life. Even if he claims not to believe in God, the atheist appreciates the tranquility and beauty of the natural world (he recalls fondly his long walks in the forests of New Zealand during his undergraduate days and the nature walks and runs in Singapore). The Freethinker likes flowers and the outdoors as well. “I like to watch the koi pond, it is very peaceful”, he says. The Environmental Domain of the Spiritual Well-being Model, which emphasises harmony and connection with nature, is one of its four domains [40,41].
Two participants who claimed to be members of religious orders and who said they pray in the nursing home do not use religious coping mechanisms to handle the difficulties of living in a nursing home. There is no contradiction here because having a religious faith or being religious implies partaking in religious activities generally (e.g., going to worship services, praying daily, etc.), whereas religious coping is the process by which people use their religious convictions to demonstrate behaviours (either positive or negative religious coping behaviours) to deal with stress and loss [43,44].
Support for spiritual needs
Over 90% of the participants-23 people with or without a religious faith-reported needing spiritual support to help them deal with their health issues and worries about meaning, purpose, beliefs, or a connection to God.
“You know one thing which is very lacking here, pastoral care, this is totally lacking. They may say they have a pastor and all that… If he does come down because it is to preach. If you go in and look there are a lot of them there waiting to die. They’ve got nothing to do. Pastoral care should be more than just preaching. It should be really getting to know and understand how the elderly feel and communicate with him.” (A5, Length of Stay: >5 years, Male, Chinese)
“… you can pray but must go toilet, use clean water wash face, mouth, nose, ears, hair, arms, feet. Nobody got time take me toilet five times, wash clean before pray <referring to ritual washing called ‘wudu’ by Muslims before praying>.” (C6 Length of Stay: 3-5 years, Male, Malay)
“That will help. That will help. But there’s nobody, ‘ah’ there's nobody. That probably will help, probably will help. Most humans when they come this condition, this age, similar ideas come into their brain <thoughts of suicide and feeling helpless as he is paralysed waist down.>” (D1, Length of Stay: 3-5 years, Male, Indian)
These 23 participants stated that even before the COVID-19 pandemic they either did not have the opportunity to go to their places of worship, receive support from prayer groups, or receive spiritual counseling to deal with their deteriorating health conditions or existential questions or that their opportunities to do so were very limited.
“That time I stay at my nephew’s house, Neptune court, Holy Family <name of the church>. I can walk, go church. <Now>, No. Just stay at home and pray at bed.” (B2, Length of Stay: >5 years, Female, Chinese)
“None of this are existing <visits by church volunteers>… there’s nobody, ‘ah’ there’s nobody. That probably will help, probably will help. Most humans when they come this condition, this age, similar ideas come into their brain… There is nothing to look forward now with my condition. I don’t mind passing away because I’m living in a wheelchair, just lying down.” (D1, Length of Stay: 3-5 years, Male, Indian)
“No cannot go out. Nobody wants to bring.” (D3, Length of Stay:1-2 years, Female, Chinese; D3 has never been to a Buddhist temple after being admitted to the nursing home)
The two participants stated that a religious organisation of their faith founded the nursing home where they live so they received some help for their spiritual needs. But they also said that they haven't visited their churches since being admitted to the nursing home. When his siblings made the special arrangement to fetch him up from the nursing home, one participant had only ever attended weddings of younger family members at his former church.
Guiding value
Guiding values are moral principles, an ideology, or religious convictions that establish residents’ behaviours and attitudes [45-47]. Only actions that are visible manifestations of a person's values can be noticed.
A little over 90% of the participants, or 23 out of 25 people, use their religious beliefs to influence their behaviour and frame of reference. These participants include people who identified as members of religious groups as well as two Freethinkers who hold the belief in God.
“For me, all human being must be together in harmony. Don't fight, have peace… Respect like friend, like brother is important.” (C6, Length of Stay: 3-5 years, Male, Malay)
“I believe in God ‘lah’. You cannot just live on your own. There must be somebody above, right?” (D2, Length of Stay: 3-5 years, Male, Chinese)
“One day, one food. We also get that one food. Here every day, they give me food. If you do good things, God will help… I believe no one day also no food... I never ask you any food and never worry one day. ‘Amman’ <Goddess> give, every day ‘Amman’ <Goddess> give even the ant one sugar. Same as me also.” (E2, Length of Stay: 1-2 years, Female, Indian)
Participants also have values and/or beliefs that have been ingrained in them since they were young and shaped by their life experiences (both positive and negative experiences), such as the importance of hard work as a value and not relying on others, the value placed on money, the belief that honesty is overrated and mistrust of people.
“Work hard to earn money. Don’t go and ask people for money.” (C2, Length of Stay: 1-2 years, Male, Chinese)
“It all depends. The money factor. All the people who are rich, they have pastors coming to their houses and preach to them. Whereas the poor people, they have to go to the church.” (E5, Length of Stay: >5 years, Male, Chinese)
“Good people in the open. But inside don't know. One thing you cannot trust people. You cannot trust human being… In life, it is very hard to be honest, everything honest, cannot.” (B3, Length of Stay: 3-5 years, Male, Chinese)
Nonreligious, yet fundamental human ideals guide both the Freethinker and the Atheist in their daily lives and social relationships.
“To be kind to each other, to take more time to understand each other, the areas where you don’t have enough understanding behind the story. It is interesting how thinking develops, like a tree… You give them more benefit of doubt.” (B4, Length of Stay: 1-2 years, Male, Chinese; an atheist who is a nature lover, a man of science and optimistic about the future scientific discoveries that could treat his disease)
“I feel that after death there's nothing. It’s more like communist thinking that life after death is nothing… I don’t care about what people say, I only believe in myself. I analyse and believe in myself. Life is like that, what you like, you just do it. But no harm to others. And if you can afford to have it, that's it.” (C3. Length of Stay: 1-2 years, Male, Chinese; although he is a Freethinker, he shared that he is “more aligned to Christianity” and its teachings that “you do good, you're accepted by God”)
A life of purpose
A resident is said to be living with a purpose if they have a strong motivation in their life that drives them to continue living to realise their personal goals. “A central, self-organizing life aim that organizes and stimulates goals, manages behaviors, and provides a sense of meaning” is how McKnight & Kashdan ([48], p. 242) define the purpose. According to Keyes [49], the purpose is the intention and commitment to achieve one’s own goals that are advantageous to oneself and/or others.
Instead of being something a person is born with, the purpose is something that is discovered, made, or learned through one's experiences in life. It can also evolve throughout one's lifetime [50,51].
Over two-thirds of the participants, or 17, who claimed to have a purpose in life despite their deteriorating health and residing in a nursing home, did so. Among the 17 are both males and females from varied educational levels and ethnic groups who find meaning in their religious beliefs.
“Purpose now is to make myself good enough to go to heaven.” (A4, Length of Stay: 1-2 years, Male, Chinese).
“I pray in my heart to Allah to give me long life… I already old, very old. Do whatever make me happy I will do. Give me joy pray Allah. Pray Allah really make me healthy.” (C6, Length of Stay: 3-5 years, Male, Malay).
“When I was young, I think of many things. Now old already, my purpose is I hope I am strong and healthy. No more problem with my left leg… I pray to God my leg don’t cramp too often. I ask God to give me strength to bear the pain… And leave this world peacefully.” (D4, Length of Stay: 3-5 years, Female, Chinese).
“The purpose of my life is I live my best life until the end of my life to finish my life well. Live a proper life, a life that you feel happy. Happy to live a life that is based on Christ… Finish well, finish my life in my Lord Jesus. Live a life for Jesus.” (E4, Length of Stay: > 5 years, Male, Chinese).
There are also those among the 17 (both males and females from varied educational levels, including the atheist and the freethinkers) who choose to continue living each day as it comes with some optimism.
“Well, life I cannot take away my life. So, I just go along with it with the best I can do and no harm to others. If possible, I can do any good I'll do any good. That's all… I try not to get sick, that's the first thing, because when I'm sick I'll be a burden to people.” (C3, Length of Stay: 1-2 years, Male, Chinese).
“I am doing ‘keto’ for my health. Because this is something I can do to help myself without depending on medicine because they said xxx <name of the disease> there is no cure, but they can only treat the symptoms… To be able to be physically able again and to have the chance to <learn> more things. I want to travel.” (B4, Length of Stay: 1 - 2 years, Male, Chinese).
“I just take, what it comes ‘ah’. I cannot change the fate ‘ah’. I cannot change anything on my own. I just live from day to day that's all ‘ah’.” (D2, Length of Stay: 3 - 5 years, Male, Chinese).
“Try to help yourself, one day, day by day. Keep, keep up a, a nice, healthy body. Don't think until so sick… Don't aim for too much...So old already.” (D3, Length of Stay: 1 - 2 years, Female, Chinese).
Out of the 17 participants, there are two females who reported being there for a loved one is their life's purpose. No male participants reported on this.
“Yeah, I love her. I think that when I stay with her here, they will look after her nicely. So, with both my eyes can see. As older sister, I feel that I must always care for my younger sister… I pray God will make me healthy, I can see, take care my sister…I pray every day that I can take care my sister. Don't let people bully.” (B1, Length of Stay: 3-5 years, Female, Chinese; her sister is staying in the nursing home with her).
“I must have my leg <prosthetic leg>. I must walk to my house. I must see my God all how. Where every day I stay the house, I must put the light <for the altar lamp>… Then I want to see my husband. Cos one time I cook my own self. I blended the food, I bring go feed him. He say, “Wow, very nice.” He say very nice, say like that. Then I very happy because he like small kid like that. Say very nice like children, like that my husband say, he like smile like baby. I must go and feed him before I die because after I die then… <she cries softly>”. (E2, Length of Stay: 1 - 2 years, Female, Indian).
Around the world, women are predominantly the caregivers for family members who are unable to care for themselves due to illness or disability [52-55]. According to the social role theory [56,57], caregiving is viewed as a woman’s responsibility and societies have internalised this gender norm [58]. Across the three main ethnic groups in Singapore, it is a cultural norm and societal expectation that women take up the main responsibility for providing care for dependent relatives.
Because of their poor health, advanced age, or loneliness, 7 participants, or roughly 30% of them, both males and females from varied educational levels, ethnic groups and religious faiths, indicated that they had no reason to live and were simply waiting to pass away.
“Waiting for my death bed… Now I cannot walk. I cannot go out… Now I don't think because I have no money. I don't think. No purpose, waiting to die.” (B3, Length of Stay: 3-5 years, Male, Chinese)
“Nothing. Nothing. My hand and legs no good. Nothing can do. (B5, Length of Stay: 3-5 years, Male, Eurasian)
“There is nothing to look forward now with my condition. I don’t mind passing away because I’m living in a wheelchair, just lying down. It doesn't give, it doesn't thrill me. It doesn’t excite me; you see life is outside. When you can walk, you can travel, and everything is outside, but not inside, you see?” (D1, Length of Stay: 3-5 years, Male, Indian)
“I thinking quickly God take me away. I feel so lonely. I feel so boring. I cannot talking. Missing friends… I want to finish this world, not mine no more… I not thinking much, just thinking don't be sick and die. Die, just quiet die. Don’t pain, don’t sick, no operation nothing. Just close eyes, just quiet then go.” (E3, Length of Stay: 3-5 years, Female, Chinese)
“I guess I cannot <purpose in life> because of my age.” (E5, Length of Stay: >5 years, Male, Chinese)
One female participant didn't mention whether she was leading a purposeful life. She expressed her sadness at her children fighting over her apartment on multiple occasions. She wants them to get along, come to see her more often and bring her back home on leave.
Support for forgiveness and reconciliation
A crucial last psychosocial stage that happens as people age is the desire to forgive oneself, accept certain uncontrolled events that occurred in their lives, and work toward reconciliation [16]. According to Erikson [16], older people who do not forgive themselves or come to terms with their mistakes or tough pasts will fall into a state of despondency that may be harmful to their general health and well-being. According to this study, older people cannot experience Joy in Living while they are in a desperate situation.
Five participants spoke about:
- Inability to accept that he is an adopted child
- Frustration at not being able to reconcile with family over the abandonment
- The treatment of adoptive parents, grandmother, and family over the decades as a house help rather than an adopted child
- Regrets of past mistakes
- Inability to accept father’s re-marriage
I feel like if I were to live my life again, I want to be born properly to a family. Not an orphan… You'll feel like something that belong to somebody. Not really like me like that, nobody wants.” (A2, Length of Stay: 1-2 years, Male, Chinese)
“I don’t think they will ever visit me. I was in Geelong rehab. They were staying in Melbourne. It's about 100km. I don't understand why my wife cannot take the kids to come and see me. It breaks my heart. If the situation is reversed, I 'die die', I will make sure the kids will come and see you. No matter what.” (A4, Length of Stay: 1-2 years, Male, Chinese)
“Yeah, grandma beat me, scold me. They are Peranakan. I speak Malay, Peranakan speak Malay. She call me go market, buy things. Then she said you go find husband when I come home late. So bad that time... I cannot remember how old. Adopt me but do housework, clean house, go market, cook for them.” (B2, Length of Stay: >5 years, Female, Chinese)
“I regret my job, so many things ‘ah’! I regret so many things, my wife, my everything. I cannot say not one thing, many things. My family also I regret, I miss my family also. Because I do this robbery what and my family come to know. My family comes to know, they hate me. See, then I stay alone. I never go to mix with my family.” (E1, Length of Stay: 3-5 years, Male, Indian)
“Maybe because everybody the home this one not the same. They have the heart, friend, mother, father. I don't have mother. It's different. My father is marry second wife, then not the same already… I mean, everybody's home not the same. Some may be got love me, some nothing love much. Why should I say much, my heart pain if I think too much, right?” (E3, Length of Stay: 3-5 years, Female, Chinese)
Personal control
Studies on seniors have revealed the importance of having some control over their daily lives, which fosters their self-identity and contributes to their well-being [12,17-19].
Results of theme 5 - Personal control
All participants reported a lack of personal control in various aspects of their nursing home life. The lack of a voice to provide input or feedback on how their lives are planned and structured for them in the nursing home is a common thread.
Autonomy, having a choice
13 out of 25 participants, or slightly over 50%, believe that there is no independent living because their freedom has been taken away and their options are non-existent.
“This one, they got totally nothing here. They’ll lock you in, lock within the area. Can’t even go out. Can’t even come out here.” (A2, Length of Stay: 1-2 years, Male, Chinese)
“Here they are telling you what to do. You have no freedom to do. So, it bugs me. I make my coffee, I come out and read and drink, and they say why you come here for, so you get very frustrated...”. (C4, Length of Stay: 3-5 years, Male, Indian)
“This one is very difficult - I must go out. All the time in this pigeonhole.” (D3, Length of Stay: - 1-2 years, Female, Chinese)
“No go everywhere, just stay here.” (E3, Length of Stay: 3-5 years, Female, Chinese)
“Terrible. You can’t do anything that you want to do. You are controlled. <cannot> Smoke. I like to play football… Because everything is controlled.” (E5, Length of Stay: >5 years, Male, Chinese)
However, 11 out of 25 participants, or over 40%, reported having some control over their health conditions by taking actions to improve or maintain their physical health.
“But no matter how, ‘die die’ I still need to do. I cannot skip my exercise.” (A3, Length of Stay: 1-2 years, Male, Chinese)
“They will show us the TV , last time my leg cannot carry but after this one I see is very good, I can move my legs. Like this one very good, American exercise. Or Australia, Australia one, not sure.” (B1, Length of Stay: 3-5 years, Female, Chinese)
“But I came to this place for now for 17, 18 months and I never smoke, never drink… Fits improved, upgraded by God.” (C5, Length of Stay: 3-5 years, Male, Indian)
“… no need to drinking alcohol again. It is a blessing in disguise... My blood pressure has gone down quite a lot. I don’t even take that much medicine nowadays. They cut down my medications.” (D2, Length of Stay: 3-5 years, Male, Chinese)
“Of course. Yeah. Now I under control <blood pressure>. That time I had stop drinking and so basically everything okay now… Yes, better than last time.” (E1 Length of Stay: 3-5 years, Male, Indian)
Having a voice
20 participants, or 80%, believe they do not have a voice or a say in expressing their opinions, providing feedback, complaining, or making improvement suggestions that will be considered by staff/management.
“No. What is there to feedback because when you are given what he called the status of resident. So, in this thing, they are not accepting anything.” (C4, Length of Stay: 3-5 years, Male, Indian)
“It's up to the nursing staff here ‘ah’. They will, they will put us where they think we will sit ‘ah’.” (D2, Length of Stay: 3-5 years, Male, Chinese)
“Sometimes I will let them all know, not hot. They say, you are very fussy”. (D3, Length of Stay: 1-2 years, Female, Chinese)
“We have asked them to get a billiard table. They say ok, ok. After that nothing is done.” (E5, Length of Stay: >5 years, Male, Chinese)
Avoid being a burden
17 out of 25 residents, or slightly less than 70%, made or accepted the decision to remain in a nursing home to avoid being a burden to family members and/or make decisions and take actions to avoid bothering staff unnecessarily.
“I am married. I have been here two to three years okay. I come here to relieve my wife. She runs around do the errands, cook, then go see doctor, go to the bank, take me to see doctor because of my xxx <name of disease>. And she has cancer… Here I can be more relaxed.” (B4, Length of Stay: 1-2 years, Male, Chinese)
“He sent me to a nursing home because there is no one to look after me at home… I sacrifice stay here.” (D4, Length of Stay: 3-5 years, Female, Chinese)
“Yeah, I cannot do my own thing much. Because I fall down, I cannot walk. Just maybe hard at home, she also want to do the housework, our own house. I mean I cannot do anything then she has to work <her daughter-in-law>… My daughter-in-law cannot help me … no strong.” (E3, Length of Stay: 3-5 years, Female, Chinese)
“Cannot walk then very hard... Trouble for them <for staff to take him on outings>.” (B5, Length of Stay: 3-5 years, Male, Eurasian)
“In the room <stay in the room after exercise>. Difficult for people, the staff <to transfer him from bed to wheelchair often>”. (C1, Length of Stay: >5 years, Male, Chinese)
Acquire new knowledge and skills
Seven of the 25 participants (both males and females from various educational backgrounds), or slightly less than 30%, expressed a desire to learn new things.
“I want to learn how to how to do ‘Zoom’ and I would like to do tuition again and I can give tuition for free.” (A5, Length of Stay: >5 years, Male, Chinese)
“Want to learn <to go on internet and use the various functions>. But how to learn?” (C2, Length of Stay: 1-2 years, Male, Chinese)
“Yeah, I would like to <learn to use a smartphone and surf the internet>. I’m still very alive.” (C3. Length of Stay: 1-2 years, Male, Chinese)
“Like something benefit for us ‘lah’. Provided I understand that then I would like to learn… Then more education in life… learn new things… If learn to talk in other languages,” (D3, Length of Stay: - 1-2 years, Female, Chinese)
“I like someone got class, try to learn drum or anything. I like.” (E3, Length of Stay: 3-5 years, Female, Chinese)
Adapting to changes
According to the Theory of Gero-transcendence, the ability to change one’s worldview in later life to adapt to changing external environments and circumstances is the beginning of the change journey in relationship with self, others and the cosmos that occurs in old age [20].
Results of theme 5 - Adapting to changes
Residents who can orient and accept changes in their new lives in a nursing home can have Joy in Living moments despite diminished health functions and lifestyle restrictions imposed by communal living.
Acceptance of new reality
22 participants, or over 80%, accept the current reality of their diminished health functions. However, given the strain of their increasing care needs on family members, most of them accept their family members' decision to place them in a nursing home half-heartedly as a ‘no choice’ situation.
Three residents expressed their dissatisfaction with their diminished health functions.
“Nothing. Nothing. My hand and legs no good. Nothing can do… My dream is 80 pass away. Now 76. 4 more <years>.” (B5, Length of Stay: 3-5 years, Male, Eurasian)
“Now I cannot walk. I cannot go out. I happen to go out, my eyes will be gone…” (B3, length of Stay: 3-5 years, Male, Chinese)
“Well do you want to know something? I will tell you honestly. I do pray that the lord will end my life. I don’t want to continue to live anymore.” (D1, Length of Stay: 3-5 years, Male, Indian)
Orientating to new reality
13 out of 25 participants, or slightly over 50%, reported being able to orient and adapt to living in a nursing home.
“I was sick, I fall down. Yeah, so my friends say it’s very difficult, you two stay and no people to look after I and my sister…I see the home is quite good, my friend told me, so they let me think over around three days… I think to make sure my sister also wants to go. My sister says okay, we go in a home better.” (B1, Length of Stay: 3-5 years, Female, Chinese).
“You think yourself ‘lah’ you think you because you stay here also same like own house. Thinking we are at home… This is ‘rumah’ <house in Malay>.” (E3, Length of Stay: 3-5 years, Female, Chinese)
Most of those who can adapt to living in a nursing home do so by becoming accustomed to it.
“I stay here quite long already. I use to.” (C6, Length of Stay: 3-5 years, Male, Malay)
“Initially, I felt very upset and lonely <about not being able to go to church>. I have no alternative; I have to get used to it. So, I got used to it now. (D1, Length of Stay: 3-5 years, Male, Indian)
Four residents, or slightly less than 20% of the participants, expressed strong opposition to being forced to live in a nursing home because of their changed circumstances.
“Yeah, I feel that whatever it is, I don’t find any excuse for anybody. This place is not correct. These people don't belong there. This is supposed to be a nursing home, to nurse from injury, you take care of somebody, not somebody who’s waiting to die. What’s the point, I am coming here to live here like this, this is a wrong condition.” (A2, Length of Stay: 1-2 years, Male, Chinese)
“For me, I can take care of myself so many years all along. Why should I need to be in a home? I know the reason simple, they didn’t accept me, but I didn’t expect it to be all the way you know. They took my freedom; they took my freaking life away.” (C4, Length of stay: 3- years, Male, Indian)
“I was thinking my brother from hospital bring me home. He said I will send you to nursing home. He didn’t mention which nursing home. I told him that if I am not happy, I want to go home. Now, he don’t agree. Every night, before I sleep, I pray to God that my brother send me home. I want to go home.” (D4, Length of Stay: 3-5 years, Female, Chinese)
Desire to be free from worries
There is a growing interest in the impact of worries on seniors. Many recent studies have found that anxiety caused by worry leads to a lower quality of life [59-61]. Most recent studies rely on Borkovec's [62] definition of worry, which defines worry as a continuous sequence of negative thoughts while attempting to solve a current problem with unclear solutions and outcomes.
Results of theme 7 - Desire to be free from worries
Free of financial worries
14 of the 25 participants, or more than half, mentioned once during the interview that they are free of financial worries because nursing home fees are subsidised by the government and the remaining portion is paid by family members or from rental proceeds of a vacant house managed by a family member.
“I think my brother is arranging that... I don’t know. I simply pass my time like that, no problem. I never go and check whether many more money left or what. I never go and check.” (C3. Length of Stay: 1-2 years, Male, Chinese)
“The Nursing Home? We all are subsidised anyway, so we don’t pay much ‘lah’. Well, the government is already paying a lot… You only pay a few dollars a month ‘ah’. Usually, my sister will pay ‘lah’. She looks after all my financial problems.” (D2, Length of Stay: 3-5 years, Male, Chinese)
“Because I come here, I don’t need to worry about the three meals, who cook for me, go where, marketing, how to buy, how to go, like this.” (D3, Length of Stay: 1-2 years, Female, Chinese)
“Because my nursing home take care of me and give me the food. Most important the food ‘lah’… Now one day also without food I never sleep. The time come already, they give the food. So, you enjoy the life here.” (E1, Length of Stay: 3-5 years, Male, Indian)
Only one interviewee mentioned being free of financial worries more than once.
“Young time I was worried…Everything I worry. If have enough money for rent, food, and everything. <Now> Everything is free. Just don’t want to worry.” (C2, Length of Stay: 1-2 years, Male, Chinese)
Free of caregiving obligations and/or managing a household
Only the code under the sub-theme ‘free of caregiving obligations and/or managing a household’ had a gender skew in response. No male participants reported being free of caregiving responsibilities and/or household management. Two female participants stated that they were exempt from this obligation. One female participant made a unique reference to being free of this obligation during the preliminary analysis of data from the first three nursing homes. The sub-theme is retained in the final framework of seven themes and sub-themes on Joy in Living experiences in nursing homes because another female participant reported on it in the data analysed from the last two nursing homes.
“I stay here, no need to do work. I stay here good…Now, I no need to walk, and just lie down. Last time in my home, cook, cook, cook then scold. At my nephew’s house, he got so many things, too many things, the plate too many to wash.” (B2, Length of stay: >5 years, Female, Chinese)
“You know after the falling down, I cannot do much. <before the fall> I help to clean the house first and after clean nothing to do, so I go out. Sometimes few, my daughter-in-law cook more. Now no need, so good now.” (E3, length of Stay: 3-5 years, Female, Chinese)
Discussion
The aim of this study was to uncover the lived experiences of elderly residents in nursing homes and acquire an understanding of what truly and essentially constitutes Joy in Living from their perspective. The study was also meant to shed light on the enabling conditions that nursing home operators can implement that are conducive for Joy in Living, and disenabling conditions to be avoided or eliminated for Joy in Living experiences of residents to flourish. The results showed that there are seven themes that are important for Joy in Living experiences of elderly to flourish in nursing homes: (i) ‘supportive nursing home environment and practices’ that includes adopting person-centred care, (ii) ‘meaningful daily living’, (iii) ‘connectedness through meaningful relationships’, (iv) ‘fulfil the need for spiritual care’, (v) ‘personal control’, (vi) ‘adapting to changes’ and (vii) ‘desire to be free from worries’.
These themes include the enabling and disenabling conditions to Joy in Living in nursing homes and when enabled, are conducive to Joy in Living experiences of the elderly residing in nursing homes. For example, if a nursing home allocates resources, builds capability of its staff, and works with volunteers to provide activities and opportunities for residents to have meaningful daily living, then this constitutes an enabling condition to Joy in Living in nursing homes, while neglecting meaningful engagement is a disenabling condition to Joy in Living in nursing homes.
Supportive nursing home environment and practices
The themes are all interconnected and, when enabled, promote Joy in Living experiences. The themes will be discussed individually and cross-referenced with other themes as needed to elaborate on a discussion point. The foundational theme that provides the conducive ecosystem for Joy in Living experiences to flourish is ‘supportive nursing home environment and practices’. This is reflected in the fact that it ranks first in terms of the frequency of coding reference. Within this theme, eight distinct sub-themes are visible to varying degrees (small, moderate, or large) in the five nursing homes, as determined by the number of mentions and associated emotions in each interview and across interviews and observation data.
The critical sub-themes that need to be in place to a moderate extent at least for Joy in Living experiences to flourish as these are experienced by residents daily are ‘leadership competency’, ‘person-centred care’, ‘supportive living environment’, ‘staff competency and capacity’, and ‘food for residents’. The most significant sub-theme is ‘leadership competency’.
The frequency of coding references to ‘leadership competency’ is lower than the other sub-themes because residents in general do not have a complete 360-degree view of how a nursing home is run because they interact with frontline care staff more than the leadership team. Residents cannot see the leadership involvement in driving person-centricity as a philosophy and culture. Leadership involvement is not readily apparent, except when the leadership team is seen walking the grounds or attending staff briefings at observation sessions (e.g., in Nursing Home B), or when staff mentions leadership support in impromptu conversations at observation sessions (e.g., mention of CEO conducting dementia training in Nursing Home A). Staff interviews, which were not one of the study's data collection methods, could have provided data on leadership direction and support. However, this is not a limitation of the study. The purpose of the study is to capture the voices and lived experience of residents in nursing homes. Therefore, the data collection methods best suited for the study are interviews with residents and observations of their activities in their natural environment.
According to a review of the literature on the impact of leadership on organisations, ‘leadership competency’ is the most important sub-theme because management sets the tone of the culture and practices in a nursing home, which affects organisational performance and outcomes [63-66]. There are numerous definitions of leadership; one that stands out is “a process by which an individual influences a group of individuals to achieve a common goal” [67]. Using this definition of leadership, we can see why the ‘leadership competency’ sub-theme is the bedrock of the daily lived experience of personalised care, an empowering living environment, staff with the capacity and competencies to provide Person-centred Care, and food served that considers residents’ ethnic preferences.
Person-centred Care extends beyond medical and nursing needs to include psychosocial and mental well-being (which are addressed in theme 2 on ‘meaningful daily living’ and theme 3 on ‘connectedness through meaningful relationships’). Person-centred Care [5] and variations of Person-centred Care, such as Person-directed Care [6] and the Eden Alternative model [7], have been shown in studies to improve the well-being of elderly people in nursing homes, have positive impact on care outcomes for them, improve staff morale, retention, and organisational performance [102-104].
Person-centred Care has been implemented to a moderate extent in Nursing Homes A, B, C, and D in areas such as grooming, medication administration, monitoring, assisted feeding, and support at group activities and exercises. Nursing Home E has embraced Person-centred Care to a large extent by providing these services, avoiding over-reliance on restraints, and planning to identify residents who are suitable for assisted toileting and wean them off adult diapers. Both Nursing Homes A and E have designed living spaces that promote a family concept of communal living and are, to a large extent, conducive to Joy in Living. Although Nursing Homes B, C, and D have dormitory-style bedrooms for their residents, they have softened the institutional feel by providing inviting common shared spaces for residents and gardens on their premises that are moderately conducive to Joy in Living.
Given the demands on staff resources to implement COVID-19 infection control safety protocols, staff capacity is a real challenge for all five nursing homes. To a moderate extent, all five nursing homes manage the increased workload and challenges of recruiting foreign staff during the peak of the COVID-19 pandemic by relying on a handful of staff per shift and overtime. All five nursing homes ensure adequate rest for staff by rostering shifts/overtime/covering arrangements and making changes to foreign staff housing and ward zoning to reduce COVID-19 cross-infection among staff and residents. Nursing Home E has implemented these measures and taken advantage of the opportunity to re-design the job scopes of their Healthcare Attendant (Activities) and Physiotherapy Associates to take on greater responsibilities in the delivery of psychosocial engagement, physiotherapy, and occupational therapy programmes, respectively, to relieve the workload of their already overburdened allied health workforce. These employees are guided and reviewed to ensure the quality and safety of the services they provide to residents.
Also, empowering junior staff to plan and organise meaningful activities for residents in Nursing Home E during extended periods when volunteers were not permitted to visit residents and conduct programmes has positively mitigated feelings of loneliness and boredom, as elaborated in sections 5.10 and 6.2 on ‘meaningful daily living’.
Despite having a central kitchen onsite to cook meals for residents, all five nursing homes only met the dietary needs and preferences of their residents to a moderate extent. During the pre-interview observation session, the kitchen at Nursing Home A was being renovated. When the post-interview observation was carried out several months later, their kitchen had already been operational, but there was no difference in the food waste observed at both sessions. Although residents’ meals must adhere to the dietician's order of a reduced sugar/saturated fat/sodium diet or soft diet preparation, there is still room for improvement in this area. Residents have complained about the poor taste, cold meals, and meals that do not meet their ethnic dietary needs of vegetarian meals on certain days and spicier meals/curries. This is supported by data on food waste collected in all five nursing homes. An impromptu conversation at an observation session at Nursing Home D revealed that they had piloted a once-a-week meals order from a hawker centre for its residents, which had been well-received. The programme has since been discontinued, and the staff has no idea why. In terms of frequency of coding reference, the ‘safety and security’ sub-theme has the second highest score. The caveat is that the prevalence of this sub-theme in interviews and observation data is primarily because of COVID-19 safe distancing and infection control measures. These measures have been widely implemented in all five nursing homes. The COVID-19-related safety measures in this sub-theme, on the other hand, have negative consequences on theme 2 on ‘meaningful daily living’, which is elaborated in sections 5.10 and 6.2.
‘Clear communications’ ranks lowest in terms of frequency of coding reference and is present to varying degrees in all five nursing homes. Again, this could have been gleaned from staff interviews, which were not one of the study's data collection methods. The sub-theme of ‘clear communications’ is not a critical sub-theme to have for Joy in Living experiences to flourish in a nursing home because there are instances of residents experiencing Joy in Living despite the nursing home scoring a small extent in having clear communications. 30% of participants reported miscommunication and misunderstanding of COVID-19 restrictions on next-of-kin visits and certain nursing home policies, and two senior members of the nursing team of two nursing homes expressed frustration with dealing with unreasonable next-of-kin. While having ‘clear communications’ is not critical, it is beneficial to clear misunderstandings and manage the expectations of various stakeholder groups (i.e., staff, residents, next of kin and volunteers).
Given the scarcity of nursing care and allied health staff resources in the ILTC sector, the sub-theme on ‘continual improvement efforts’ to innovate and harness technology to improve staff productivity and service delivery experiences is the short- to medium-term direction for all nursing homes to take. Nursing Homes A, B, C, and D have moderately implemented ‘continual improvement efforts’ by implementing centralised laundry and kitchen services and implementing technology (an autonomous robot for food delivery in Nursing Homes A and D and an automated steam machine to clean the floors of the dining hall of Nursing Home C). Nursing Home E has adopted ‘continual improvement efforts’ to a large extent through the adoption of centralised laundry and kitchen services, technology (use of ceiling hoist for transfer of bedbound residents and ambulatory hoist and forearm rollator for physiotherapy walking exercise) and implementing an innovative ‘Hope Kee’ programme conducted entirely by staff to improve the psychosocial well-being of its residents.
The significance of the sub-themes of the ‘supportive nursing home environment and practices’ theme in this study was identified in several quantitative studies conducted in Singapore. A study by Wang et al., ([9], p. 1) to identify “predictors of self-reported Quality Of Life (QOL) of NH residents in Singapore” revealed that “depression and difficulty in communication with staff are the two main modifiable risk factors of poor QOL of local NH residents”. According to the findings of the quantitative study, higher food enjoyment scores were negatively associated with major depression and poorer cognitive function. Higher autonomy scores were negatively associated with major depression, increased dependence, and difficulty communicating with staff. Theme 5 on ‘personal control’ in sections 5.14 and 6.5 discusses autonomy.
Meaningful daily living
It is surprising that, despite the adoption of Person-centred Care approaches in Singapore nursing homes, the findings of the theme on ‘meaningful daily living’ highlight widespread feelings of boredom among our nursing home residents. Despite Brownie and Nancarrow's [68] study found that management and staff in aged care facilities equate good care solely with good medical care, nursing homes in Singapore continue to prioritise medical and nursing care at the expense of focusing resources on residents' broader aspirations for psychosocial and mental well-being.
One key finding in a recent local study on “QOL, Person-centred Care, and lived experiences of nursing home residents in a developed urban Asian country” by Tew et al., ([69], p. 1) is that “beyond their basic care needs, the residents' psychosocial needs can be better fulfilled”. 696 residents from seven Singapore nursing homes participated in the cross-sectional study. The survey asked about five aspects of care: “environment, interaction with people, activities, food, and impact on lifestyle and overall”. Less than half were satisfied in “areas of psycho-emotional needs and autonomy (interaction with the community, maintain a home routine, awareness of happenings outside NH <nursing home>, staff informing residents about what is happening and considering their preferences)” ([69], p. 6). The survey findings in the five dimensions of care highlight the importance of improving psychosocial care and empowering elderly residents.
The current COVID-19 pandemic has highlighted the over-reliance on volunteers to organise meaningful recreational activities that engage residents and provide social interaction to avoid boredom and loneliness. Although a few nursing homes in Singapore have implemented online platforms such as ‘Zoom’ virtual sessions for volunteers to interact with residents and conduct activities for them (I observed a ‘Zoom’ session led by church volunteers at Nursing Home A), the reach and variety pale compared to pre-Covid volunteer activities (as gathered from the interviews with residents).
While the relaxation of COVID-19 safety measures should encourage volunteer-led activities, this should only be one pillar of a multi-pronged approach. Another pillar could be developing staff internal capabilities and providing sufficient bandwidth for staff to organise and carry out such activities; for example, Nursing Home E’s innovative ‘Hope Kee’ programme and Nursing Home A’s ‘Mini-mart’ initiative. Another way to avoid boredom and foster a sense of belonging is to increase the number of opportunities for residents to volunteer in the nursing home. Currently, less than 20% of participants reported being able to spend their time meaningfully.
Given that ethnic minorities have reported a lack of activities as well as a lack of newspapers and reading materials in their vernacular languages, nursing homes can consider how to best address this by hiring staff or volunteers who speak the vernacular languages of the ethnic minorities residing in nursing homes and providing reading materials in their vernacular languages.
Connectedness through meaningful relationships
According to a review of the literature, research has shown the value of establishing and preserving relationships in assisting the elderly in overcoming social isolation and loneliness. Themes 2 and 3 discovered in this Joy in Living study were disclosed by the two distinct studies by Bowers et al., [17] and Katz et al., [18]: Seniors with high care requirements place a high priority on meaningful interpersonal connections (existing or new), participating in fulfiling and enjoyable activities, giving back to the nursing home and other residents, and maintaining or enhancing their physical health.
Only slightly less than 50% of the participants in this study indicated that they were friends with care staff, and the main reasons given by the participants were language barriers and the care staff's busy schedules, which prevented them from forming new relationships with foreign care staff (especially staff from Myanmar who generally cannot speak good English). During the observation sessions, it was observed that staff members concentrated on the duties at hand and generally avoided engaging in casual discussions with residents. Nursing homes may want to put incoming foreign employees through structured modular programmes in spoken English, Mandarin, Malay and dialects like Hokkien to help with the language barrier issue. The staff's perspective needs to be changed so that talking with residents is seen as a crucial job that also enhances their psychological well-being and allows for the early identification of any issues or fears that the elderly may have to make any necessary adjustments to the care plans. Management would need to free up enough time for staff to take on this new duty. The bandwidth required for this can be created by utilising technology and automation to reduce the present workload of nursing personnel through regular, repetitive chores.
Several local mid-career hires were observed engaging residents more effectively during the observation sessions. These staff are literate in the local tongues. These local mid-career hires present a chance to augment the foreign staff strength and improve overall resident engagement.
Friendships are frequently made at schools, places of employment, places of religion, within groups of people who share interests and with neighbors. Most of the participants - representing all racial and ethnic groups, both sexes, and a range of educational backgrounds-cited difficulties with developing friendships because of language issues, being on different wavelengths, and having different mentalities. It is unreasonable to assume that seniors will make acquaintances on their own because of living in communal settings. Instead of leaving things to chance, some deliberate action needs to be taken on this front, including a review of living arrangements and the creation of chances for residents to interact with people from other wards besides those on their own.
Many residents receive little to no help from their families. According to the interviews, the residents experienced a lot of stress and sadness because of unresolved family matters, family members who are too busy to visit them often, and/or a lack of possibilities to reconcile strained relationships. The management of nursing homes needs to reevaluate the existing care paradigm, which places an excessive emphasis on residents' physical health. To better focus resources on psychological well-being, their care service delivery paradigm must be reviewed. Investment in family-bonding measures, including family counseling, family participation in caregiving, and nursing home events, is a crucial part of this.
Fulfil the need for spiritual care
For Joy in Living experiences to grow, it is crucial to ‘fulfil the need for spiritual care’, which is an additional dimension that Person-centred Care models do not address. It is not surprising that this subject has emerged in the study since, following the Theory of Gero-transcendence [20], relationships with one's self, others, and the universe change as one age. For Joy in Living experiences to flourish, the study identified five sub-themes of the main theme, ‘fulfill the need for spiritual care’: (i) ‘religious or spiritual beliefs’; (ii) ‘support for spiritual needs’; (iii) ‘guiding values’; (iv) ‘a life of purpose’; and (v) ‘support for forgiveness and reconciliation’. Literature on religion and spirituality supports the findings of the study.
There are many definitions of spirituality in the literature. Notwithstanding the variety in the definition, there are some common themes such as personal to the individual, inner connection, self in harmony with the external world, the quest for answers to existential questions, relationship with the cosmos or God, and being spiritual with or without religious faith. For example, Puchalski ([70], p. 36) explained that “some measures have included religious attendance or frequency of prayer . . . while others have looked at more existential or philosophical constructs such as meaning in one’s life or satisfaction with achieving life’s goals”. On the other hand, religion is described as a prescribed set of beliefs, customs, and practices that identifies an individual with a particular religious faith [71]. Puchalski [70] associated spirituality with the very essence of being human and the source of our existence and for this very reason, there were studies in the last two decades advocating that spirituality be considered and offered in clinical care settings [72-74]. Waaijman [75] claimed that spirituality involves a relationship to a God or a higher power and can be expressed in many art forms and the interaction with nature, community, and family. Pattison et al., [76] stated that many individuals associate their religious beliefs with spirituality, yet an individual can be spiritual without being religious.
The theme on ‘connectedness through meaningful relationships’ is another one that will help Joy in Living experiences thrive. MacKinlay [77] asserts that having a close connection to others, especially those who are important in one's life, is a key component of spirituality. She continued by saying that people who have maintained a spiritual connection throughout their lives have a more balanced outlook on life, continue to live lives of meaning as they become older, and are receptive to new concepts and ways of doing things. The ‘communal’ domain, which focuses on a person's interactions with other people, is one of the four domains of the Spiritual Well-being Model [40,41]. These studies further strengthen the premise that fulfilling the need for spiritual care is important for Joy in Living experiences to flourish and is a new dimension to be considered in Person-centered Care Model [5] and its variations Person-directed Care Model [6] and Eden Alternative Model [7] in the delivery of services to nursing home residents.
There have been many studies on two of the sub-themes under this theme, ‘religious or spiritual beliefs’ and ‘a life of purpose’ and their link on a range of positive well-being outcomes, and physical and mental health [78-80]. A person’s physical health begins to decline as they get older. Studies have found that those with positive religious coping behaviours handle their disease, despair, pain, and death anxiety better when presented with a debilitating or terminal illness [81-83] Meanwhile, research has shown that unhealthy religious coping mechanisms are more strongly linked to worsening mental and physical health [84-86].
According to Pargament [42], one of religion’s major goals is to help people discover a purpose for their lives. Finding purpose in life is an ongoing quest that endures hardship, ageing, and even the knowledge of impending death [87]. Studies have shown that those who have a purpose in life live longer and have higher immune systems [88,89]. According to the study’s findings, slightly over 70% of the participants said they used positive religious coping mechanisms to varying degrees, which was reflected in their positive attitudes toward their lives. Nearly 30% of the participants said they felt like there was no point in living because of their poor health, advanced age, or loneliness.
In light of this study and the preceding studies, nursing homes should consider setting aside resources and/or collaborating with external organisations to provide ‘support for spiritual needs’, counseling ‘support for forgiveness and reconciliation’ and, co-designing meaningful activities and opportunities for residents to volunteer their skills and talents to lead a ‘life of purpose’, as these conditions, when enabled, allow Joy in Living experiences to flourish. When disenabled, it leads to bitterness and despair, as shown in figure 4.
 Figure 4: Joy in living versus despair.
Figure 4: Joy in living versus despair.
Personal control
Bowers et al., [17] and Katz et al., [18] conducted separate studies that revealed common themes of personal identity and self-esteem contributing to the quality of life. Even with the loss of independent living and the loss of control over many aspects of their lives, the elderly in nursing homes want to maintain as much control as possible over their daily lives, with healthcare service providers seeking and hearing their opinions [17,90]. A local study by Tew et al., [69] revealed that less than half were satisfied in “areas of psycho-emotional needs and autonomy” (p. 6). The survey findings in the five dimensions of care highlight the need to increase the empowerment of elderly residents in Singapore nursing homes.
Given the findings of the aforementioned studies and this study, which show that more than half of the participants strongly believe there is no independent living and that 80% believe they have no say, we can conclude that empowerment practices and culture are lacking in nursing homes. Reduced personal control does not foster Joy in Living experiences. Nursing homes should consider redesigning work processes to balance work efficiency with resident needs in areas such as:
- Shower timings and duration
- Mealtimes and special diet preferences (e.g., vegetarian meals on certain days, having spicier curries and choice of cuisines of the ethnic minority groups)
- To allow residents and their next of kin access to amenities of the nursing home and gardens outside their wards with the relaxation of COVID-19 safe distancing measures at the national level
- Choice of activities to participate in
- Opportunity to learn new skills of interest and keep up with mainstream technology use
Nursing homes should think about implementing a structured process for soliciting resident feedback and closing the feedback loop on actions taken.
Adapting to changes
According to the findings of this study, many residents (nearly half of the participants) are unable to adjust and adapt to living in a nursing home. There will be difficulties during the adjustment period, and if it is too long and residents are left to their own devices, they may “get used to it” or become depressed and resentful that their family has forced this decision on them. These are the conditions that prevent Joy in Living experiences from flourishing in nursing homes. As a result, nursing homes should intervene early to assist residents in adjusting to this change in living situation. Most nursing homes create care plans for residents before their admission. A nursing home social worker could arrange a family meeting with the resident and family members before admission to discuss openly why they have decided to place the elderly in the nursing home and how they each feel about the upcoming change in living arrangements for the resident. The social worker should emphasise the importance of continued involvement and visits by family members at this family meeting.
During the first six months of a resident’s stay in the nursing home, social work and nursing staff can conduct monthly check-ins to learn how residents are adjusting to life in a nursing home, gather feedback on their daily lived experiences, and identify their interests and talents. Their interests and talents can be incorporated into care plans and developed by organising classes to teach the skills and creating opportunities for them to volunteer their services. Following the initial six-month period, such check-ins can be scheduled on a six-monthly basis.
Desire to be free from worries
While worry has been established as one of the major symptoms of anxiety disorders, moderate levels of worry, like moderate levels of stress, can nudge a person to solve a problem before it becomes unmanageable, according to Granier and Segal [91]. However, the study found that seniors with fewer resources than younger working adults are less able to solve problems, and their worry can quickly lead to anxiety and even depression.
Given the research on the negative impact of worrying on mental and physical health, nursing homes must monitor changes in the financial situation of residents and their families at the proposed six-monthly check-ins with residents and/or when next-of-kin fails to pay monthly caring fees. The social work department can work with the family to study the various government subsidy schemes/funds and nursing home charity funds that are available to pay the caring fees and even help with the family's expenses if their financial situation changes drastically (e.g., loss of job of the main breadwinner, etc.).
Conclusion
The findings on ‘connectedness through meaningful relationships’, ‘meaningful daily living’, ‘desire to be free from worries’, 'personal control,’ and ‘adapting to changes’ are consistent with the findings of the three studies by Bowers et al., [17], Katz et al., [18] and Minney & Ranzijn [19]. According to the findings of the study by Minney & Ranzijn [19], participants’ ability to accept the loss of certain aspects of their lives before retirement, willingness to modify their current lifestyles because of health impediments, and freedom from responsibilities and worries all influenced their perception of a Good Life.
This study yielded two new themes: ‘supportive nursing home environments and practices’ and ‘fulfil the need for spiritual care’. Even Rinnan et al., [12] study on the Joy of Life of the Elderly in Norwegian Nursing Homes did not find a spiritual component among the five dimensions identified. The study by Rinnan et al., [12] revealed one dimension of ‘sources of meaning’ that is aligned with one of the sub-themes: ‘a life of purpose’ of the ‘fulfil the need for spiritual care’ theme as revealed by this study. The frequency of coding reference was not the only basis for organising the themes and sub-themes within the theoretical framework. A literature review and the first author’s experience on Sree Narayana Mission (Singapore)’s Board of Directors were also used to interpret the data. For example, the sub-theme ‘leadership competency’, which is ranked seven out of the eight sub-themes of the theme ‘supportive nursing home environment and practices’, is ranked as the most impactful because management sets the tone of the culture and practices in a nursing home.
The study sheds light on the seven themes that have emerged as important for Joy in Living experiences of elderly to flourish in nursing homes that include the enabling and disenabling conditions.
The following recommendations address the implications for operators of nursing homes:
Implications for operators of nursing homes
Supportive nursing home environment and practices
In the area of supportive nursing home environments and practices, management as the nursing home’s leadership team can do more to role model desired behaviours and be more ‘hands-on’ in soft skills training programmes to bring the values of their organisations to life through storytelling to inspire staff. Staffing and duty rostering should be reviewed to ensure adequate staff bandwidth and rest to prevent burnout, especially with the ongoing COVID-19 outbreaks in the community. Management can also establish systems and practices that encourage staff and resident feedback for improvement efforts, as well as hold regular communication sessions with them to keep them up to date on evolving COVID-19 measures and other policies affecting the ILTC sector and their nursing home.
Nursing homes should expand their staff development training programmes to include people’s skills training as well as spoken English and vernacular language courses for foreign staff. Within one year of joining the organisation, nursing home management can collaborate with external training providers or AIC to develop structured modular programmes on basic, intermediate, and advanced spoken English for new foreign staff (particularly staff from Myanmar). In their second year of employment, all new foreign staff can be scheduled to attend basic spoken Mandarin, Hokkien, Cantonese, and even Malay courses. Existing staff (foreign or local) can attend the spoken vernacular language courses as a refresher course. Such training programmes can help foreign staff and residents communicate more effectively.
Current training emphasises nursing skills-based training, as evidenced by daily shift handover meetings and educational posters on display in nursing homes. Certain soft skills training programmes, such as resilience training for nursing staff, can even be extended to residents, providing them with the knowledge and skills they need to recover from setbacks in their health functions or the loss of a loved one or a fellow resident. Food, a conducive living environment, and safety are all basic needs that must be met. While it is important to prepare nutritious meals for the elderly, management must be aware that repeated menu options can lead to boredom. Having a diverse menu featuring local delicacies and catering to residents with dietary restrictions such as vegetarians, vegans, and Muslims who require halal meals are important considerations. By eating the same meals as the residents on certain days, management can ensure the quality of meals catered or prepared in-house. Nursing homes may want to consider ordering meals from selected hawker stalls which are recognised for their nutritious food content for at least one meal per week, where residents can choose their meal from a pre-set menu.
Management can work with consultants experienced in designing elderly communal living spaces to build homely, conducive, and accessible physical spaces for the elderly to encourage social interaction and participation in activities that promote independence when revitalising existing nursing home premises or designing new nursing home facilities. Physical security and safety are critical. However, rather than using restraints excessively, management should balance residents’ desire for autonomy versus fall prevention and investigate pharmacological and non-pharmacological therapy interventions to treat agitation in residents. For a longer-term solution to the bird nuisance problem, management can collaborate with the National Parks Board of Singapore on innovative and ethical methods to control the bird population near nursing homes.
Meaningful daily living
To foster a sense of belonging, the nursing home’s social work department can collaborate with the nursing team to identify residents’ talents, skills, and interests within three to six months of admission. Opportunities for residents to volunteer their services based on their talents and skills can be created. A resident who can play a musical instrument or sing, for example, can lead a music interest group. Also, management can expand their volunteer base to tap into external expertise to train residents who want to learn a new skill or organise community-based activities for residents. Also, management can consider developing staff capabilities and restructuring their jobs to allow them to organise activities for residents. To avoid boredom, there is room to expand the breadth and depth of social and recreational activities available to residents.
Connectedness through meaningful relationships
Most nursing homes in Singapore have care plans in place for their residents. These care plans are created before admission and are expanded upon throughout the patient’s stay in the nursing home. When creating individual care plans, the social work department can collaborate with the nursing team to house residents who share a common language, educational background, and interests. Nursing homes can provide opportunities for residents to participate in games and recreational activities, as well as share meals with residents from other male and female wards. Also, there is an opportunity to supplement the foreign workforce with local mid-career recruits who are switching careers to improve overall engagement with residents.
Fulfil the need for spiritual care
Nursing home operators in Singapore can do more to provide spiritual care for their residents. Nursing homes should consider hiring spiritual counsellors who can connect residents with community resources and provide the appropriate faith, spiritual, and cultural support. Within each region of Singapore, there may be a pool of nursing home chaplains of various faiths who can be called upon to support residents’ spiritual needs. Although the ‘fulfil the need for spiritual care’ theme is only one of seven, it is the least developed in Singapore nursing homes when compared to the other themes. The study findings and recommendations on this theme, if implemented in Singapore nursing homes, will significantly improve Joy in Living experiences in nursing homes (Table A2; appendix A).
Implications for the regulator of nursing homes
‘Personal control’, ‘adapting to changes’ and ‘desire to be free from worries’
The Ministry of Health (MOH) regulates and funds nursing homes. Operating licenses are granted to nursing home operators who meet the minimum Enhanced Nursing Standards, which specify three aspects of compliance: (1) clinical care; (2) social care; and (3) governance and organisational excellence. Breaching the terms and conditions may result in the suspension or revocation of the nursing home license, as well as prosecution.
MOH has the option of revising the Enhanced Nursing Standards to include the following:
- Provide residents with ‘personal control’, i.e., the ability to have a say in their care plans and daily activities and implement a structured mechanism to gather feedback from residents under the standard’s ‘social care’ dimension
- Assist residents in ‘adapting to changes’, such as transitioning from living in their homes to a communal living arrangement in the nursing home during the pre-admission stage and the first six months of a resident’s stay in the nursing home under the standard’s ‘social care’ dimension; and
- Under the ‘social care’ dimension of the standard, provide residents and next-of-kin with financial counselling and assistance in accessing available government grants and subsidies with the evolving family financial situations
Fulfil the need for spiritual care
The ‘fulfil the need for spiritual care’ theme is the least developed in Singapore's nursing homes. Based on the findings of this study and other studies on the positive impact of spirituality on well-being outcomes and improved physical and mental health in older adults, MOH can consider expanding the standard’s ‘social care’ dimension to include spiritual care for nursing home residents.
Strengths & limitations of the study
The study’s strength is its understanding of what truly and essentially constitutes Joy in Living from the perspective of Asian elderly residents of multicultural Singapore, as well as the identification of a new dimension on meeting residents’ spiritual needs in Person-centred Care approaches to allow Joy in Living experiences to flourish. While the small sample size prevents findings from being generalisable to all nursing homes in Singapore, future quantitative or mixed methods studies with larger samples can confirm the findings. The study’s revision from two observation sessions to at least one observation session either before or after the interviews for the fourth and fifth nursing homes is one of its limitations. The original intention of having two observation sessions was that if one of the observation sessions was biased, the other session would provide a balanced perspective and thus a more robust and rigorous design. The first author attempted to conduct one observation before and after the interviews whenever possible. However, given the critical situation with COVID-19 cluster developments at several nursing homes, nursing home management was hesitant to set aside already overburdened staff resources to facilitate the conduct of two observation sessions (either in-person or virtually). As a result, the final two nursing homes received only one post-interview observation session.
Although the last two nursing homes only had one observation session, the first author maintained a balanced perspective of the observation data through impromptu conversations with staff and residents to arrive at an unbiased viewpoint. For example, observations of a shift handover meeting in Nursing Home E revealed an over-reliance on diapers and efforts to wean residents off them, which was then probed for better understanding during an impromptu conversation with an assistant nurse manager. Also, the data from the observation session was triangulated with the interview data from Nursing Home E residents to arrive at the study’s insights/findings.
Another limitation of the study is that the interviews were conducted in English, which excluded elderly people who could only communicate in vernacular languages. To some extent, this limitation was overcome by including participants who could understand and speak basic English in the study.
These changes, if implemented by nursing home operators and MOH, are expected to promote better psychosocial well-being of the elderly and better living environments in which nursing home residents can enjoy satisfactory accommodation while spending their remaining years in joy.
References
- Department of Statistics Singapore (2021). Population Trends. SingStat, Singapore.
- Hirschmann R (2021) Forecasted share of the population aged 65 years and above in Singapore in 2019, 2030 and 2050. Statista, Germany.
- Goh LG, Kua EH, Chiang HD (2015) Ageing in Singapore: The next 50 years. Spring Publishing Pte Ltd, Singapore.
- Basu R (2016) Safe but soulless: Nursing homes need a new narrative. Lien Foundation & Khoo Chwee Neo Foundation. Pg no: 1-138.
- Rogers CR (1961) On Becoming a Person: A Therapist's View of Psychotherapy. Houghton Mifflin, Massachusetts, USA.
- White DL, Newton-Curtis L, Lyons KS (2008) Development and initial testing of a measure of person-directed care. Gerontologist 48: 114-123.
- Thomas WH (2003) Evolution of Eden. Journal of Social Work in Long-Term Care 2: 141-157.
- Engel GL (1977) The need for a new medical model: A challenge for biomedicine. Science 196: 129-136.
- Wang P, Yap P, Koh G, Chong JA, Davies LJ, et al. (2016) Quality of life and related factors of nursing home residents in Singapore. Health Qual Life Outcomes 14: 112.
- Chaturvedi SK, Muliyala KP (2016) The Meaning in Quality of Life. Journal of Psychosocial Rehabilitation and Mental Health 3: 47-49.
- Gray RS, Rukumnuaykit P, Kittisuksathit S, Thongthai V (2008) Inner Happiness Among Thai Elderly. J Cross Cult Gerontol 23: 211-224.
- Rinnan E, André B, Drageset J, Garåsen H, Espnes GA, et al. (2018) Joy of Life in nursing homes: A qualitative study of what constitutes the essence of Joy of Life in elderly individuals living in Norwegian nursing homes. Scand J Caring Sci 32: 1468-1476.
- Carstensen LL, Turan B, Scheibe S, Ram N, Ersner-Hershfield H, et al. (2011) Emotional Experience Improves with Age: Evidence Based on Over 10 Years of Experience Sampling. Psychol Aging 26: 21-33.
- Baltes PB, Baltes MM (1990) Successful Ageing: Perspectives from the Behavioral Sciences. Cambridge University Press, Cambridge, UK.
- Giele JZ, Elder GH (1998) Methods of life course research: Qualitative and quantitative approaches. Sage Publications, California, USA.
- Erikson EH (1963). Childhood and Society (2ndedn.). W.W. Norton & Co, New York, USA.
- Bowers H, Clark A, Crosby G, Easterbrook L, Macadam A, et al. (2009). Older people’s vision for long term care. Joseph Rowntree Foundation, York, UK.
- Katz J. Holland C, Peace S, Taylor E (2011) A better life: What older people with high support needs value. Joseph Rowntree Foundation, York, UK.
- Minney MJ, Ranzijn R (2016) “We Had a Beautiful Home . . . But I Think I’m Happier Here”: A Good or Better Life in Residential Aged Care. Gerontologist 56: 919-927.
- Tornstam L (1997) Gerotranscendence: The contemplative dimension of aging. Journal of Ageing Studies 11: 143-154.
- Leedy PD, Ormrod JE (2001) Practical research: Planning and design (7thedn). Merrill Prentice Hall and Sage Publications.
- van Manen M (1990) Researching lived experience: Human science for an action sensitive pedagogy. State University of New York Press, New York, USA.
- Braun V, Clarke V (2006) Using thematic analysis in psychology. Qualitative Research in Psychology 3: 77-101.
- Braun V, Clarke V (2021) One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qualitative Research in Psychology 18: 328-352.
- Braun V, Clarke V (2019) Reflecting on reflexive thematic Qualitative Research in Sport, Exercise and Health 11: 589-597.
- Creswell JW (2007) Qualitative inquiry and research design: Choosing among five approaches (2ndedn). Sage Publications, California, USA.
- Cohen MZ, Kahn DL, Steeves RH (2000) Hermeneutic Phenomenological Research: A Practical Guide for Nurse Researchers. Sage Publications, California, USA.
- Lawton MP, Nahemow L (1973) Ecology and the ageing process. In: Eisdorfer C, Lawton MP (eds.). The psychology of adult development and ageing. American Psychological Association: 619-674.
- Iwarsson S, Ståhl A (2003) Accessibility, usability and universal design--positioning and definition of concepts describing person-environment relationships. Disabil Rehabil 25: 57-66.
- McCormack B, Dewing J, McCance T (2011) Developing person-centred care: Addressing contextual challenges through practice development. Online J Issues Nurs 16: 3.
- Werngren-Elgström M, Carlsson G, Iwarsson S (2009) A 10-year follow-up study on subjective well-being and relationships to person-environment (P-E) fit and activity of daily living (ADL) dependence of older Swedish adults. Arch Gerontol Geriatr 49: 16-22.
- Aryana IGPS, Kuswardhani RAT (2018) Sarcopenia in elderly. International Journal of Geriatrics and Gerontology 1: 1-4.
- Dorner TE, Luger E, Tschinderle J, Stein KV, Haider S, et al. (2014) Association between nutritional status (MNA®-SF) and frailty (SHARE-FI) in acute hospitalised elderly patients. J Nutr Health Aging 18: 264-269.
- Marques M, Faria A, Cebola M (2019) Body mass index and body composition in institutionalized older adults with malnutrition, sarcopenia and frailty. European Journal of Public Health 29: ckz034-070.
- World Health Organisation (2022) Malnutrition. World Health Organization, Geneva, Switzerland.
- Chinnakkaruppan A, Wintzer ME, McHugh TJ, Rosenblum K (2014) Differential Contribution of Hippocampal Subfields to Components of Associative Taste Learning. J Neurosci 34: 11007-11015.
- Bowling A (2008) Enhancing later life: How older people perceive active ageing? Aging Ment Health 12: 293-301.
- Williamson T (2010) My Name is not Dementia: People with Dementia Discuss Quality of Life Indicators. Alzheimer’s Society, London, UK.
- Atchley RC (1989) A continuity theory of normal aging. Gerontologist 29: 183-190.
- Fisher JW (2001) Comparing Levels of Spiritual Well-being in State, Catholic and Independent Schools in Victoria, Australia. Journal of Beliefs and Values 22: 99-105.
- Fisher JW (2011) The Four Domains Model: Connecting Spirituality, Health and Well-Being. Religions 2: 17-28.
- Pargament KI (2001) The psychology of religion and coping: Theory, research, practice. The Guilford Press, New York, USA.
- Pargament KI (1997) The Psychology of Religion and Coping: Theory, Research, Practice. Guilford, New York, USA.
- Sherman AC, Simonton S (2001) Assessment of religiousness and spirituality in health research. In: Sherman AC, Plante TG (eds.). Faith and Health: Psychological Perspectives, Guilford, New York, USA.
- Ajzen I, Fishbein M (1980) Understanding Attitudes and Predicting Social Behavior. Prentice Hall, New Jersey, USA.
- Rokeach M (1968) Beliefs, attitudes, and values: A theory of organization and change. Jossey-Bass, San Francisco, USA.
- Rokeach M (1973). The Nature of Human Values. Free Press, New York, USA.
- McKnight PE, Kashdan TB (2009) Purpose in Life as a System that Creates and Sustains Health and Well-Being: An Integrative, Testable Theory. Review of General Psychology 13: 242-251.
- Keyes CLM (2011) Authentic purpose: The spiritual infrastructure of life. Journal of Management, Spirituality & Religion 8: 281-297.
- Baumeister RF, Vohs KD (2002) The pursuit of meaningfulness in life. In: Snyder CR, Lopez SJ (eds.). Handbook of positive psychology. Oxford University Press. Pg no: 848.
- Park N, Park M, Peterson C (2010) When is the search for meaning related to life satisfaction? Applied Psychology: Health and Well-Being 2: 1-13.
- Haberkern K, Szydlik M (2010) State care provision, societal opinion and children's care of older parents in 11 European countries. Ageing and Society 30: 299-323.
- Quinn C, Clare L, Woods RT (2010) The impact of motivations and meanings on the wellbeing of caregivers of people with dementia: a systematic review. Int Psychogeriatr 22: 43-55.
- del-Pino-Casado R, Frías-Osuna A, Palomino-Moral PA, Ramón Martínez-Riera J (2012) Gender differences regarding informal caregivers of older people. J Nurs Scholarsh 44: 349-357.
- Sharma N, Chakrabarti S, Grover S (2016) Gender differences in caregiving among family - caregivers of people with mental illnesses. World J Psychiatry 6: 7-17.
- Eagly AH (1987) Sex differences in social behavior: A social-role interpretation. Lawrence Erlbaum Associates, Inc.
- Eagly AH (1997) Sex differences in social behavior: Comparing social role theory and evolutionary psychology. Am Psychol 52: 1380-1383.
- Glauber R (2017) Gender differences in spousal care across the later life course. Res Aging 39: 934-959.
- de Sousa RD, Rodrigues AM, Gregório MJ, Branco JDC, Gouveia MJ, et al. (2017) Anxiety and Depression in the Portuguese Older Adults: Prevalence and Associated Factors. Front Med (Lausanne) 4: 196.
- Hohls JK, König HH, Quirke E, Hajek A (2019) Association between anxiety, depression and quality of life: Study protocol for a systematic review of evidence from longitudinal studies. BMJ Open 9: 027218.
- Ribeiro O, Teixeira L, Araújo L, Rodríguez-Blázquez C, Calderón-Larrañaga A, et al. (2020) Anxiety, Depression and Quality of Life in Older Adults: Trajectories of Influence across Age. Int J Environ Res Public Health 17: 9039.
- Borkovec TD (1988) Comments on “Worry as a phenomenon relevant to the elderly”. Behavior Therapy 19: 381-383.
- Cummings GG, MacGregor T, Davey M, Lee H, Wong CA, et al. (2010) Leadership styles and outcome patterns for the nursing workforce and work environment: A systematic review. Int J Nurs Stud 47: 363-385.
- Jeon YH, Simpson JM, Li Z, Cunich MM, Thomas TH, et al. (2015) Cluster Randomized Controlled Trial of An Aged Care Specific Leadership and Management Program to Improve Work Environment, Staff Turnover, and Care Quality. J Am Med Dir Assoc 16: 629.
- Poels J, Verschueren M, Milisen K, Vlaeyen E (2020) Leadership styles and leadership outcomes in nursing homes: A cross-sectional analysis. BMC Health Serv Res 20: 1009.
- Rokstad AM, Vatne S, Engedal K, Selbæk G (2015) The role of leadership in the implementation of person-centred care using Dementia Care Mapping: A study in three nursing homes. J Nurs Manag 23: 15-26.
- Hunt JG (2004) What Is Leadership? In: Antonakis J, Cianciolo AT, Sternberg RJ (eds.). The Nature of Leadership. Sage Publications, Thousand Oaks, California, USA.
- Brownie S, Nancarrow S (2013) Effects of person-centered care on residents and staff in aged-care facilities: A systematic review. Clin Interv Aging 8: 1-10.
- Tew CW, Ong SP, Yap PLK, Lim AYC, Luo N, et al. (2021) Quality of life, person-centred care and lived experiences of nursing home residents in a developed asian urban country: A cross-sectional study. The Journal of Nursing Home Research 7: 1-8.
- Puchalski CM (2008) Spirituality and the care of patients at the end-of-life: An essential component of care. Omega (Westport) 56: 33-46.
- Baker DC (2003) Studies of the inner life: The impact of spirituality on quality of life. Quality of Life Research 12: 51-57.
- Koenig HG (2012) religion, spirituality, and health: The research and clinical implications. ISRN Psychiatry.
- Puchalski C, Ferrell B, Virani R, Otis-Green S, Baird P, et al. (2009) Improving the quality of spiritual care as a dimension of palliative care: The report of the consensus conference. Journal of palliative medicine12: 885-904.
- Saguil A, Phelps K (2012) The spiritual assessment. Am Fam Physician 86: 546-550.
- Waaijman K (2007) Spirituality-A multifaceted phenomenon. Interdisciplinary explorations Studies in Spirituality 17: 1-114.
- Pattison S, Hannigan B, Pill R, Thomas H (2010) Emerging values in health care the Challenge for professionals. Jessica Kingley Publishing, Philadelphi, USA.
- MacKinlay E (2021) Ageing and frailty: A spiritual perspective of the lived experience. Journal of Religion, spirituality & Aging 33: 236-249.
- Brown DR, Carney JS, Parrish MS, Klem JL (2013) Assessing spirituality: The relationship between spirituality and mental health. Journal of Spirituality in Mental Health 15: 107-122.
- Ho MY, Cheung FM, Cheung SF (2010) The role of meaning in life and optimism in promoting well-being. Personality and Individual Differences 48: 658-663.
- Kim ES, Sun JK, Park N, Kubzansky LD, Peterson C (2013) Purpose in life and reduced risk of myocardial infarction among older US adults with coronary heart disease: A two-year follow-up. J Behav Med 36: 124-133.
- Pargament KI, Koenig HG, Tarakeshwar N, Hahn J (2004) Religious coping methods as predictors of psychological, physical and spiritual outcomes among medically ill elderly patients: A two-year longitudinal study. J Health Psychol 9: 713-730.
- Vitorino LM, Low G, Vianna LAC (2016) Linking spiritual and religious coping with the quality of life of community-dwelling older adults and nursing home residents. Gerontol Geriatr Med.
- Zwingmann C, Wirtz M, Muller C, Korber J, Murken S (2006) Positive and negative religious coping in German breast cancer patients. J Behav Med 29: 533-547.
- Ellison CG, Fang Q, Flannelly KJ, Steckler RA (2013) Spiritual struggles and mental health: Exploring the moderating effects of religious identity. The International Journal for the Psychology of Religion 23: 214-229.
- O'Brien B, Shrestha S, Stanley MA, Pargament KI, Cummings J, et al. (2019) Positive and negative religious coping as predictors of distress among minority older adults.International journal of geriatric psychiatry 34: 54-59.
- Rababa M, Hayajneh AA, Bani-Iss W (2021) Association of death anxiety with spiritual well-being and religious coping in older adults during the COVID-19 pandemic. Journal of Religion and Health 60: 50-63.
- Frankl V (1962) Man’s search for Meaning. Simon and Shuster, New York, USA.
- Hill PL, Turiano NA (2014) Purpose in Life as a Predictor of Mortality Across Adulthood. Psychol Sci 25: 1482-1486.
- Fredrickson BL, Grewen KM, Coffey KA, Algoe SB, Firestine AM, et al. (2013) A functional genomic perspective on human well-being. Proc Natl Acad Sci USA 110: 3684-13689.
- Potter C (2009) What quality healthcare means to older people: Exploring and meeting their needs. Nurs Times 105: 14-18.
- Granier KL, Segal DL (2021) Diverse Aspects of Worry among Younger and Older Adults: A Multifaceted Approach. Psychology 12: 441-461.
- Doyle C, Lennox L, Bell D (2013) A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 3: 001570.
- Fors A, Ekman I, Taft C, Björkelund C, Frid K, et al. (2015) Person-centred care after acute coronary syndrome, from hospital to primary care - A randomised controlled trial. Int J Cardiol 187: 693-699.
- Lowther K, Harding R, Simms V, Ahmed A, Ali Z, et al. (2018) Active ingredients of a person-centred intervention for people on HIV treatment: analysis of mixed methods trial data. BMC Infect Dis 18: 27.
- Kitwood T (1997) Dementia Reconsidered: The Person Comes First. Open University Press, Berkshire, USA.
- Edvardsson D, Sandman PO, Borell L (2014) Implementing national guidelines for person-centered care of people with dementia in residential aged care: Effects on perceived person-centeredness, staff strain, and stress of conscience. Int Psychogeriatr 26: 1171-1179.
- Barbosa A, Sousa L, Nolan M, Figueiredo D (2015) Effects of Person-Centered Care Approaches to Dementia Care on Staff: A Systematic Review. Am J Alzheimers Dis Other Demen 30: 713-722.
- Kim SK, Park M (2017) Effectiveness of person-centered care on people with dementia: A systematic review and meta-analysis. Clin Interv Aging 12: 381-397.
- Ulin K, Olsson LE, Wolf A, Ekman I (2016) Person-centred care - An approach that improves the discharge process. Eur J Cardiovasc Nurs 15: 19-26.
- Goldfarb MJ, Bibas L, Bartlett V, Jones H, Khan N (2017) Outcomes of Patient- and Family-Centered Care Interventions in the ICU: A Systematic Review and Meta-Analysis. Crit Care Med 45: 1751-1761.
- Byrne K, Frazee K, Sims-Gould J, Martin-Matthews A (2012) Valuing the Older Person in the Context of Delivery and Receipt of Home Support: Client Perspectives. Journal of Applied Gerontology 31: 377-401.
- Edvardsson D, Sjögren K, Lood Q, Bergland Å, Kirkevold M, et al. (2017) A person-centred and thriving-promoting intervention in nursing homes - study protocol for the U-Age nursing home multi-centre, non-equivalent controlled group before-after trial. BMC Geriatr 17: 22.
- Wilberforce M, Challis D, Davies L, Kelly MP, Roberts C, et al. (2016) Person-centredness in the community care of older people: A literature-based concept synthesis. International Journal of Social Welfare 26: 86-98.
- Braithwaite J, Herkes J, Ludlow K, Testa L, Lamprell G (2017) Association between organisational and workplace cultures, and patient outcomes: Systematic review. BMJ Open 7: 017708.
- Cho E, Lee NJ, Kim EY, Kim S, Lee K, et al. (2016) Nurse staffing level and overtime associated with patient safety, quality of care, and care left undone in hospitals: A cross-sectional study. Int J Nurs Stud 60: 263-271.
- Moore L, Britten N, Lydahl D, Naldemirci Ö, Elam M, et al. (2017) Barriers and facilitators to the implementation of person-centred care in different healthcare contexts. Scand J Caring Sci 31: 662-673.
- Ree E (2020) What is the role of transformational leadership, work environment and patient safety culture for person-centred care? A cross-sectional study in Norwegian nursing homes and home care services. Nurs Open 7: 1988-1996.
Appendix A
|
Theme |
Sub-Theme |
Description |
|
Supportive Nursing Home Environment and Practices |
Person-centred Care |
Implementing a holistic care approach that emphasizes the well-being of the elderly as a whole person beyond just nursing and medical care. This includes residents receiving care that is tailored to their needs. Nursing homes use various Person-centred Care approaches such as the Person-centred Care Model or its variations such as Person-directed Care or Eden Alternative Model to guide the delivery of care for elderly residents. |
|
Supportive Living Environment |
Creating a good living space in the nursing home for residents’ comfort and an experience of living in their own homes. |
|
|
Safety and Security |
Systems, processes, and practices that protect residents from harm or injury. |
|
|
Staff Competency & Capacity |
Building staff professional competencies, personal leadership, interpersonal and soft skills, and knowledge. At the same time, ensuring that staff has sufficient bandwidth by hiring adequate headcount and rostering of duties. |
|
|
Food for Residents |
Meals in nursing homes fulfil each resident's dietary needs (e.g., vegetarian diet on certain days, diabetic calorie control, "Halal" meals, etc.,) and ethnic dietary preference of what they enjoy most and find satisfying. And/or Giving residents opportunities to eat food that has nostalgia associated with it based on the social and celebratory deep memories that can include care and love. |
|
|
Continual Improvement Efforts |
Innovative or improved resident care policies, systems, processes, products, or services and care delivery approaches that improve nursing home residents’ lives. And/or reaping cost savings by bringing activities together in one place (e.g., a central kitchen, centralised laundry services) or outsourcing and using technology to simplify time-consuming tasks of staff. |
|
|
Leadership Competency |
Management of the nursing home shows by example and/or implements systems, processes, and practices that place the needs of the residents at the heart of the design and delivery of services. |
|
|
Clear Communications |
Residents receive up-to-date and clear information on the COVID-19 situation, national policies and programmes, and the rules of the nursing home. |
|
|
Meaningful Daily Living |
Promote Physical and Mental Health |
Residents participate in leisure activities and activities that involve communication and interaction with others that are tailored to the needs and preferences of individual residents. And Residents participate in exercises and activities with movement (either solo or group activities) that have benefits for health, both physical and mental health; including occupational therapy activities that help to maintain health and promote the independence of the elderly residents. |
|
A Sense of Belonging |
Having a feeling of acceptance, inclusion, and identity as a valued member of the nursing home. |
|
|
|
Pursue Interest |
Setting aside time for residents to take up leisure activities of their choice and have sufficient rest.
|
|
|
Avoid Boredom |
Boredom is a state of being weary and restless when there is too much time and limited or no opportunities to be engaged in social and recreational activities or pursue interests. |
|
Connectedness through Meaningful Relationships |
Develop New Relationships |
Systems (i.e., the structure of how an organisation is set up), processes (i.e., activities and tasks that need to be carried out to achieve the outcomes), and practices (i.e., the behaviours and actions of staff) that encourage bonding between residents and care staff (including volunteers). As a result of the bonding, residents feel that staff/volunteers genuinely care for and support them throughout their stay in the nursing home. And/or Systems, processes, and practices that encourage bonding and friendship among residents. |
|
Maintain Familial and Prior Relationships |
Proactively exploring opportunities (e.g., counseling by social workers from the nursing home) to mend and/or improve relations with residents' families. Also, residents can communicate and see their family members and friends as easily as when they were living in the community. |
|
|
Fulfil the Need for Spiritual Care |
Religious or Spiritual Beliefs |
Relating to a particular religion and its ways or relating to matters of the human spirit or soul. |
|
Support for Spiritual Needs |
Meeting residents’ need for inner awakening beyond everyday existence or *Gerotranscendence. * Gerotranscendence is a theory that older people transcend the limited opinions and views of life they once held, and develop a new understanding of the self, relationships to others, and fundamental existential questions.
Support for spiritual growth includes provision of resources by the nursing home in the pursuit of God-consciousness, spiritual and self-actualisation goals. |
|
|
Guiding Values |
Moral standards, are ideology or religious views that guide behaviours and attitudes in the lives of residents. |
|
|
A Life of Purpose |
A central motivation in a resident’s life that gives him/her a reason to carry on living to achieve personal aspirations. |
|
|
New Sub-theme: Support for Forgiveness and Reconciliation |
The need to forgive oneself and for reconciliation. Erik Erikson's 8th stage in human development 'Integrity versus Despair' emphasises the importance of this to prevent the descent into desperation and its negative impact on mental and physical health in old age. |
|
|
Personal Control |
Autonomy, Having a Choice |
Residents have opportunities and autonomy to perform actions and move around without being constrained by staff or other parties. And/or Residents have a feeling of autonomy (i.e., freedom from external control or influence; independence) in taking actions to improve their health. |
|
Having a Voice |
Giving residents an active and participatory role in either deciding or influencing a decision on their care plans and daily activities. |
|
|
Avoid Being a Burden |
Residents not wanting to cause others (especially their loved ones and caregivers) a lot of difficulties, worry, or hard work in their care. |
|
|
Acquire New Knowledge and Skills |
Growth opportunities are provided or supported by the nursing home for residents to acquire new knowledge and skills. |
|
|
Adapting to Changes |
Acceptance of New Reality |
Residents can accept their diminished health functions. |
|
Orientating to New Reality |
Residents adjust their lives toward the established norms of communal living in a nursing home. |
|
|
Desire to be Free from Worries |
Free of Financial Worries |
Residents not wanting to feel troubled or being required to do something about their finances. |
|
Free of Caregiving Obligations and/or Managing a Household |
Residents not wanting to feel stressed due to caregiving obligations to children, grandchildren, or spouses, and/or responsible for managing a household. |
Table A1: Themes and sub-themes.
|
Summary of Studies on Person-Centred Care and the Findings |
|||
|
Item Number |
Theme |
Summary of the Study Findings |
References |
|
1 |
Improved health outcomes in clinical settings |
Patient-centred care is associated with a better care process with positive outcomes, such as clinical effectiveness, satisfaction ratings, and improved Quality Of Life (QOL). |
[92-94] |
|
2 |
Effectiveness of Person-centred Care of people with dementia |
Person-centred care is associated with a positive impact on well-being, QOL, improvements to degree of depression severity, and reduced behavioural symptom of agitation in persons with dementia. |
[95-98] |
|
3 |
Reduction in cost to healthcare organisations |
Patient-centred care interventions in intensive care units and hospital treatments that resulted in cost savings from reduced length of hospital stay and improvements to discharge process. |
[99,100] |
|
4 |
Effectiveness of Person-centred Care of elderly in nursing homes and home care services |
Person-centred Care associated with a positive impact on well-being, mental and physical health, and QOL. |
[101-103] |
|
5 |
Barriers and facilitators for implementing Person-centred Care |
Organisational conditions such as culture, structures, processes, leadership, and HR practices that facilitate or hinder implementation of Person-centred Care |
[104-107] |
Table A2: Summary of studies on Person-centred Care and the findings.
Citation: Dayanandan S, Mehta K (2023) What Does Joy in Living Mean to Elderly Residents of Nursing Homes in Singapore? - The Full Study. J Gerontol Geriatr Med 9: 156.
Copyright: © 2023 Swapna Dayanandan, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

