
“What the Women Want”. An Overview on Labiaplasty: Function and Beauty Researched with an Aesthetic Gynecological Procedure
*Corresponding Author(s):
Fedele LemboPlastic And Reconstructive Surgery Department, Ospedali Riuniti-OORR, University Of Foggia, Foggia, 71100, Italy
Tel:+39 0881733803,
Email:lembofedele@gmail.com
Abstract
Labiaplasty is the most commonly performed female cosmetic genital surgery procedure. Women sought labiaplasty for aesthetic reason and/or for functional impairment. Despite increasing numbers of procedures performed, there is a lack of consensus of standards of nomenclature, of care and of outcomes. The aim of this study was to clarify the current notions and the management of these women. A systematic literature review of the last 5 years (2015-2020) was performed using the PubMed database. The search returned 111 articles; after applying inclusion criteria to identify studies evaluating classification of labia minora hypertrophy, surgical techniques, complications and outcomes, 50 articles were selected (11 reviews, 3 clinical trials, 36 prospective and retrospective studies). In this brief review the authors clarify that no consensus exists in the literature regarding the classifications of labia minora hypertrophy. Overall, 7 different techniques have been reported, and patient satisfaction rates ranged from 95 to 100 percent. The most common complication described was wound dehiscence (around 5%).
The analysis of literature clearly shows that the counselling is fundamental and women’s motivations for treatment should be carefully explored. A complete medical, sexual, psychological and gynecological history should be obtained in all patients before surgery. To achieve the best outcomes in both functionality and appearance with minimal complication rates and greatest patient satisfaction, trained surgeons must inform patients about normal variations and about the potential risks of surgery, perform psychological evaluations (multidisciplinary approach), discuss realistic expectations, and personalize the technique of surgery. Although labiaplasty was described as a safe procedure with a high satisfaction rate, current study includes few patients with short follow-up. Further clinical studies should be performed to: validate current practices, define optimal management of patients and investigate long-term outcomes.
Keywords
Cosmetic genital surgery; Labial hypertrophy; Labia minora; Labiaplasty
INTRODUCTION
The surgical reduction of labia minora, defined labiaplasty, was first described in literature by Hodgkinson and Hait in 1984 [1]. About 56% of Plastic Surgeons perform labiaplasty worldwide and, over the years, this procedure has become more popular. In 2018 a total of 132.664 procedures (1.3% of total) were performed worldwide, with an increase of 25% vs 201 [2]. In 2018 Brazil was the Country in which there are recorded the higher number of procedures, about 18.476; in USA 13.668, and in Italy 4.800 [2]. According to data of American Society of Plastic Surgeons, 11.218 procedures were performed in 2019, up 9 percent from 2018 [3].
So, labiaplasty is the most commonly performed FCGS (female cosmetic genital surgery) procedure. This increase was secondary to amplified exposure to female nudity in the media and internet, which cause a definition of an ideal look of female genitalia, that, however, differs between Countries [4,5]. Women sought labiaplasty for aesthetic reason and/or for functional impairment such as irritation, pain or physical and psychological discomfort, especially in adolescent patients [6-8]. In fact, hypertrophy of labia minora can cause self-esteem reduction, insecurity when wearing tight clothing (for job or sport), dryness, irritation, tearing, chronic urinary tract infections, dyspareunia and discomfort during sexual intercourse [9,10].
Although these surgical procedures are debated for ethical aspects, about 95% of patients are satisfied with outcomes on quality of life and self-perception [11,12]. There is no consensus regarding the use of criteria to define a diagnosis of labial hypertrophy, and it has been proposed that surgery should be pursued with the presence of any chronic symptomatology. Various classifications and surgical techniques exist, with no consensus regarding their use. The lack of standards of nomenclature, of care and of outcomes have caused questions about the level of safety and efficacy of these procedures [13]. The aim of this study was to clarify the current notions and the management of these women.
MATERIALS AND METHODS
A systematic literature review of the last 5 years (2015-2020) was performed using the PubMed database with the following search algorithm: ((labiaplasty) OR (labial hypertrophy)) AND ((etiology) OR (epidemiology) OR (classification) OR (treatment)). The primary literature search returned 111 articles. The authors independently reviewed article titles and abstracts to identify all studies that assessed labial hypertrophy classification, labiaplasty techniques and outcomes. Selected articles that met these inclusion criteria then underwent full text review. Information from commentaries/replies, conferences and published abstracts was excluded. After applying inclusion criteria, of 111 articles returned, only 50 articles were selected as pertained to vaginal labiaplasty (11 reviews, 3 clinical trials, 36 prospective and retrospective studies). All articles were in English language.
DISCUSSION
Labial hypertrophy classification
The labia minora vary in length (7 mm to 5 cm), thickness, symmetry and protuberance. Women’s health care professionals play a fundamental role in helping patient to understand their normal anatomic variation [14-16]. Labial hypertrophy is most commonly congenital, but can be acquired also (androgenic hormones in infancy, topical estrogen, stretching or weight attachment, lymphedema, recidivate dermatitis, myelodysplastic diseases) [17]. There is no consensus on classification [18,19]. The most used classification system, first described by Franco [20], divides 4 stages based on the distance from the base of the labia minora to the most distal tip:
- • Stage I:
- • Stage II: 2-4 cm
- • Stage III: 4-6 cm
- • Stage IV: >6 cm
Other classifications are: the Motakef classification that is based on the protrusion of the labia minora that exceeds the size of the labia majora [21]; the Banwell classification that categorizes the labia according to the shape and morphologic variations [22]; and the Chang classification that propose 4 classes of labia protrusion based on size and location [23]. Less used classifications are described by Oranges [24] and by Mayer [25].
Preoperative consultation
In 2016, 2017 and 2020 ACOG Committee (American College of Obstetricians and Gynecologists) recommended that the women should be informed about normal variations and physical changes, that the patient’s physical and emotional development had to be evaluated, and that consultation about non-surgical technique should be provided [26-29]. In fact, counselling is fundamental to ensure that women have reliable information about normal variations and physiological changes in the external genitalia over the lifetime and about possible complication of surgery, especially in adolescents [30-34]. Many women desire the labia minora roughly symmetric, non-exposed or invaginated under of the labia majora. Women’s motivations for treatment should be carefully explored. A complete medical, sexual, psychological and gynecological history should be obtained [35-38]. In fact, principal contraindications are: body dysmorphic syndrome, enhancing sexual lives and orgasm [39].
Labiaplasty techniques
When performing a labiaplasty, the essential goals should include the reduction of the hypertrophied labia minora with maintenance of the neurovascular supply, preservation of the introitus, optimal color/texture match, and minimal invasiveness [40-45]. Although many surgical techniques have been reported in the literature, (including deepithelialization, [46] direct excision, [47] W-shaped resection, [48] wedge resection, [49-53] composite reduction, [54-55] Z-plasty, [56] and laser labiaplasty [57,58], few studies have defined an algorithm for choosing the optimal surgical procedure according to the degree of deformity. Patient-specific techniques chosen based on the patient’s anatomy and applied with a realistic approach can increase patient satisfaction and reduce complication rates. Overall, the different techniques reported can be categorized into three groups: edge resection; wedge resection; and central resection.
Edge resection
In this technique, the excess of labial tissue is removed by resecting the most protruding part. This excision can be performed either in a line that follows the curve of the labia, in an S-shaped line, or in a W-shaped resection. The S-shaped resection, or the double-W-shaped incision or the Z-plasty is widely used technique to increase the length of the scar and to reduce the effects of scar contraction [48-58].
Wedge resection
Wedge resection is the most popular labiaplasty technique. It includes various adaptations that have been made to improve aesthetic results (such as preserving the shape and colour of the labia) or to prevent loss of sensation or necrosis. The location of the wedge can be adjusted to the most bulging part of the labia minora. The central wedge resection can be performed with or without first identifying and preserving the main labial artery [50].
Giraldo et al., [56] perform a 90° Z-plasty in order to prevent scar contraction. When reduction of the clitoral hood is also desired, a central wedge can be combined with a “lateral anterior curved excision of redundant lateral labium and excess lateral clitoral hood” [50]. The wedge can also be placed posteriorly in a posterior wedge resection [49], or inferiorly with a superior pedicle flap.
Central resection
Central resection is used to maintain the original texture, contour, and pigmentation of the labial edge and includes de-epithelialization [46] and fenestration [59]. Choi et al., [46] described a de-epithelialization technique using a triangle-shaped marking centred in the labia minora. Ostrzenski et al., [59] marked the amount of tissue to be removed centrally in the labia minora in a ‘bicycle helmet’ shape. Excision is performed, and the inner and outer surface of the labia minora are sutured separately, without suturing the erectile tissue between them.
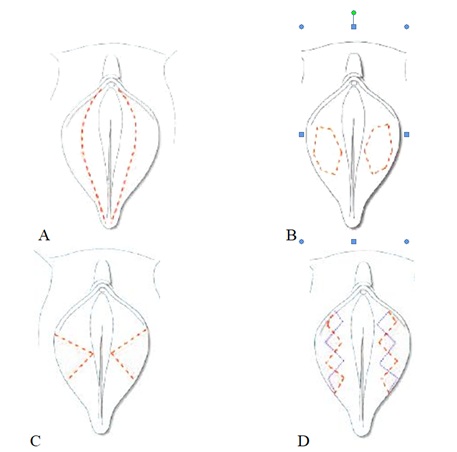
A. Direct excision; B. Deepithelialization; C. Central wedge resection; D. W-resection.
In current literature there isn’t any comparative analysis of all reported labiaplasty techniques to establish a standard operative planning. Ellsworth et al., [60] proposed this algorithmic approach: patients with Franco type I and type II may be treated most effectively with the deepithelialization technique. Patients with Franco type III or type IV may be more appropriate candidates for either the direct excision or the wedge resection technique. However, future larger studies should validate this approach.
ADVANTAGES AND DISADVANTAGES
Each technique offers its own advantages and disadvantages [61]. Although direct excision is a simple technique, yet it removes the natural contour, coloration, and texture of the free edge of the labia minora and may lead to visible scar formation. In contrast, deepithelialization may preserving the natural border of the labia minora and its neurovascular supply, but it may be unsatisfactory for wider labial width. Wedge resection retains the natural contour and coloration of the free edge of the labia minora; however, it may create an abrupt contrast in the coloration where tissues are sutured. Composite reduction is a technique that addresses both labial protrusion and clitoral hooding with excellent aesthetic outcomes. However, the complication and reoperation rate for this technique is also the highest described in the literature (about 17 percent) [55].
COMMON COMPLICATION
In current literature, few studies report on the surgical outcomes of labiaplasty with a patient satisfaction rates ranged from 95 to 100 percent [62-68]. The most common complications are dehiscence, hematoma, unsatisfactory scarring, infections, flap necrosis, fistulas, clitoral hood excess and pain [69-71]. Most reviewed studies stated that resection should not reduce the width of the remaining labia minora less than 1 cm to avoid distortion of the urethral orifice. Moreover, the resection should not extend to the posterior fourchette to avoid distorting the vaginal introitus [69,70]. More work needs to be done to validate each of these methods, better compare the available techniques, the risks and benefits for each method, and validate treatment paradigms, and to perform recommendations for perioperative patient management.
CONCLUSION
The request of female aesthetic genital surgery increases rapidly. Although the aesthetic labiaplasty is becoming a commonly performed surgery with exceptional patient satisfaction rates, the current literature is rather limited. With this safe, consistent and reproducible procedure, both function and beauty are becoming researched together. To achieve the best outcomes in both functionality and appearance with minimal complication rates and maximum patient satisfaction, trained surgeons must inform patients about normal variations and about the potential risks of surgery, perform psychological evaluations (multidisciplinary approach), discuss realistic expectations and individualize the technique of surgery. Further clinical studies should be performed to: validate current practices, define optimal management of patients, investigate long-term outcomes examining the impact of labiaplasty on a woman’s self-image and quality of life, and compare outcomes between various labiaplasty techniques.
CONFLICTS OF INTEREST
The authors declare that there is no conflict of interest regarding the publication of this paper.
FUNDING STATEMENT
No financing.
REFERENCES
- Hodgkinson DJ, Hait G (1984) Aesthetic vaginal labioplasty. Plast Reconstr Surg 74: 414-416.
- International Society of Aesthetic Plastic Surgery (2020) ISAPS International Survey on Aesthetic/Cosmetic Procedures. ISAPS, New Hampshire, USA.
- ASPS (2019) ASPS National Clearinghouse of Plastic Surgery Procedural Statistics. ASPS, Illinois, USA.
- Sharp G, Tiggemann M, Mattiske J (2016) Factors That Influence the Decision to Undergo Labiaplasty: Media, Relationships, and Psychological Well-Being. Aesthet Surg J 36: 469-478.
- Mowat H, McDonald K, Dobson AS, Fisher J, Kirkman M (2015) The contribution of online content to the promotion and normalisation of female genital cosmetic surgery: A systematic review of the literature. BMC Womens Health 15: 110.
- Brodie K, Alaniz V, Buyers E, Caldwell B, GranthamE, et al. (2019) A Study of Adolescent Female Genitalia: What is Normal? J Pediatr Adolesc Gynecol 32: 27-31.
- Westermann LB, Oakley SH, Mazloomdoost D, Crisp CC, Kleeman SD, et al. (2016) Attitudes Regarding Labial Hypertrophy and Labiaplasty: A Survey of Members of the Society of Gynecologic Surgeons and the North American Society for Pediatric and Adolescent Gynecology. Female Pelvic Med Reconstr Surg 22: 175-179.
- Sorice SC, Li AY, Canales FL, Furnas HJ (2017) Why Women Request Labiaplasty. Plast Reconstr Surg 139: 856-863.
- Hamori CA (2017) Discussion: Why Women Request Labiaplasty. Plast Reconstr Surg 139: 864.
- Oranges CM, Schaefer KM, Kalbermatten DF, Haug M, Schaefer DJ (2017) Why Women Request Labiaplasty. Plast Reconstr Surg 140: 829.
- Goodman MP, Placik OJ, Matlock DL, Simopoulos AF, Dalton TA, et al. (2016) Evaluation of Body Image and Sexual Satisfaction in Women Undergoing Female Genital Plastic/Cosmetic Surgery. Aesthet Surg J 36: 1048-1057.
- Turini T, Roxo ACW, Serra-Guimarães F, Abreu ML, de Castro CC, et al. (2018) The Impact of Labiaplasty on Sexuality. Plast Reconstr Surg 141: 87-92.
- Güne? A, Alinsod RM (2018) A mini-review of aesthetic gynecology and leading gynecology associations' approaches to this issue. Turk J Obstet Gynecol 15: 105-111.
- Clerico C, Lari A, Mojallal A, Boucher F (2017) Anatomy and Aesthetics of the Labia Minora: The Ideal Vulva? Aesthetic Plast Surg 41: 714-719.
- Dobbeleir JMLCL, Landuyt KV, Monstrey SJ (2011) Aesthetic surgery of the female genitalia. Semin Plast Surg 25: 130-141.
- Lloyd J, Crouch NS, Minto CL, Liao L-M, Creighton SM (2005) Female genital appearance: "normality" unfolds. BJOG 112: 643-646.
- Gulia C, Zangari A, Briganti V, Bateni ZH, Porrello A, et al. (2017) Labia minora hypertrophy: causes, impact on women's health, and treatment options. Int Urogynecol J 28: 1453-1461.
- González PI (2015) Classification of Hypertrophy of Labia Minora: Consideration of a Multiple Component Approach. Surg Technol Int 27: 191-194.
- Lykkebo AW, Drue HC, Lam JUH, Guldberg R (2017) The Size of Labia Minora and Perception of Genital Appearance: A Cross-Sectional Study. J Low Genit Tract Dis 21: 198-203.
- Franco T, Franco D (1993) Hipertrofia de ninfas / Nympha hypertrophy. J Bras Ginecol 103: 163-168.
- Motakef S, Rodriguez-Feliz J, Chung MT, Ingargiola MJ, Wong VW, et al. (2015) Vaginal labiaplasty: current practices and a simplified classification system for labial protrusion. Plast Reconstr Surg 135: 774-788.
- Banwell PE (2017) Anatomy and Classification of the Female Genitalia: Implications for surgical management. In: Hamori C, Banwell PE, Alinsod R (eds.). Female Cosmetic Genital Surgery: Concepts, Classification, and Techniques. Thieme Publishers, New York, USA. Pg no: 306.
- Chang P, Salisbury MA, Narsete T, Buckspan R, Derrick D, et al. (2013) Vaginal labiaplasty: defense of the simple "clip and snip" and a new classification system. Aesthetic Plast Surg 37: 887-891.
- Oranges CM (2015) Vaginal Labiaplasty: Current Practices and a Simplified Classification System for Labial Protrusion. Plast Reconstr Surg 136: 845-846.
- Mayer HF (2015) Vaginal Labiaplasty: Current Practices and a Simplified Classification System for Labial Protrusion. Plast Reconstr Surg 136: 705-706.
- Hamori CA (2016) Teen Labiaplasty: A Response to the May 2016 American College of Obstetricians and Gynecologists (ACOG) Recommendations on Labiaplasty in Adolescents. Aesthet Surg J 36: 807-809.
- ACOG (2017) Breast and labial surgery in adolescents 129. ACOG, Washington, D.C., USA.
- ACOG (2020) Elective Female Genital Cosmetic Surgery: ACOG Committee Opinion, Number 795. ACOG, Washington, D.C., USA.
- ACOG (2020) Elective Female Genital Cosmetic Surgery: ACOG Committee Opinion Summary, Number 795. Obstet Gynecol 135: 249-250.
- Spriggs M, Gillam L (2018) "I Don't See That as a Medical Problem": Clinicians' Attitudes and Responses to Requests for Cosmetic Genital Surgery by Adolescents. J Bioeth Inq 15: 535-548.
- Barbara G, Facchin F, Meschia M, Vercellini P (2015) "The first cut is the deepest": a psychological, sexological and gynecological perspective on female genital cosmetic surgery. Acta Obstet Gynecol Scand 94: 915-920.
- Stahl D, Vercler CJ (2018) What Should Be the Surgeon's Role in Defining "Normal" Genital Appearance? AMA J Ethics 20: 384-391.
- Runacres SA, Wood PL (2016) Cosmetic Labiaplasty in an Adolescent Population. J Pediatr Adolesc Gynecol 29: 218-222.
- Wood PL (2018) Cosmetic genital surgery in children and adolescents. Best Pract Res Clin Obstet Gynaecol 48: 137-146.
- Abbed T, Chen C, Kortesis B, Hunstad JP, Bharti G (2018) Labiaplasty: Current Trends of ASAPS Members. Aesthet Surg J 38: 114-117.
- Hunter JG (2016) Labia Minora, Labia Majora, and Clitoral Hood Alteration: Experience-Based Recommendations. Aesthet Surg J 36: 71-79.
- Sharp G, Mattiske J, Vale KI (2016) Motivations, Expectations, and Experiences of Labiaplasty: A Qualitative Study. Aesthet Surg J 36: 920-928.
- Learner HI, Rundell C, Liao L-M, Creighton SM (2019) 'Botched labiaplasty': A content analysis of online advertising for revision labiaplasty. J Obstet Gynaecol 12: 1-6.
- Huayllani MT, Eells AC, Forte AJ (2020) Body Dysmorphic Disorder in Plastic Surgery: What to Know When Facing a Patient Requesting a Labiaplasty. Plast Reconstr Surg 145: 468-469.
- Özer M, Mortimore I, Jansma EP, Mullender MG (2018) Labiaplasty: motivation, techniques, and ethics. Nat Rev Urol 15: 175-189.
- Wilkie G, Bartz D (2018) Vaginal Rejuvenation: A Review of Female Genital Cosmetic Surgery. Obstet Gynecol Surv 73: 287-292.
- Kaya AE, Dogan O, Yassa M, Basbug A, Çal??kan E (2018) A Novel Technique for Mapping the Vascularity of Labia Minora Prior to Labiaplasty: Cold Light Illumination. Geburtshilfe Frauenheilkd 78: 775-784.
- Gonzalez F, Dass D, Almeida B (2015) Custom Flask Labiaplasty. Ann Plast Surg 75: 266-271.
- Kelishadi SS, Omar R, Herring N, Tutela JP, Chowdhry S, et al. (2016) The Safe Labiaplasty: A Study of Nerve Density in Labia Minora and Its Implications. Aesthet Surg J 36: 705-709.
- Gowda AU, Chopra N, Khalifeh M (2015) Indications, Techniques and Complications of Labiaplasty. Eplasty 15: 46.
- Choi HY, Kim KT (2000) A new method for aesthetic reduction of labia minora (the deepithelialized reduction of labioplasty). Plast Reconstr Surg 105: 419-422.
- Girling VR, Salisbury M, Ersek RA (2005) Vaginal labioplasty. Plast Reconstr Surg 115: 1792-1793.
- Maas SM, Hage JJ (2000) Functional and aesthetic labia minora reduction. Plast Reconstr Surg 105: 1453-1456.
- Kelishadi SS, Elston JB, Rao AJ, Tutela JP, Mizuguchi NN (2013) Posterior wedge resection: a more aesthetic labiaplasty. Aesthet Surg J 33: 847-853.
- Alter GJ (2008) Aesthetic labia minora and clitoral hood reduction using extended central wedge resection. Plast Reconstr Surg 122: 1780-1789.
- Ju M, Wang W, Ma N, Chen W (2019) Reduction of Hypertrophic Labia Minora by Posterior-Lateral Wedge Resection with Preservation of the Central Blood Vessels and Nerve Bundle. Aesthetic Plast Surg 43: 742-749.
- Abbed T, Mussat F, Cohen M (2017) Origami Model for Central Wedge Labiaplasty: A Simple Educational Model with Video Tutorial. Aesthet Surg J 37: 132-136.
- Filho OP, Ely JB, Lee KH, Paulo EM (2020) Labiaplasty with Stable Labia Minora Retraction—Butterfly-like Approach. Plast Reconstr Surg Glob Open 8: 2664.
- Li F, Li Q, Zhou Y, Li S, Cao Y, et al. (2020) L-Shaped Incision in Composite Reduction Labiaplasty. Aesthetic Plast Surg.
- Gress S (2013) Composite reduction labiaplasty. Aesthetic Plast Surg 37: 674-683.
- Giraldo F, González C, de Haro F (2004) Central wedge nymphectomy with a 90-degree Z-plasty for aesthetic reduction of the labia minora. Plast Reconstr Surg 113: 1820-1825.
- Smarrito S (2014) Lambda laser nymphoplasty: Retrospective study of 231 cases. Plast Reconstr Surg 133: 231-232.
- González-Isaza P, Lotti T, França K, Sanchez-Borrego R, Tórtola JE, et al. (2018) Carbon Dioxide with a New Pulse Profile and Shape: A Perfect Tool to Perform Labiaplasty for Functional and Cosmetic Purpose. Open Access Maced J Med Sci 6: 25-27.
- Ostrzenski A (2014) Fenestration Labioreduction of the Labium Minus: A New Surgical Intervention Concept. ISRN Obstet Gynecol 2014: 1-7.
- Ellsworth WA, Rizvi M, Lypka M, Gaon M, Smith B, et al. (2010) Techniques for labia minora reduction: An algorithmic approach. Aesthetic Plast Surg 34: 105-110.
- Oranges CM, Sisti A, Sisti G (2015) Labia minora reduction techniques: A comprehensive literature review. Aesthet Surg J 35: 419-431.
- Boas SR, Ascha M, Morrison SD, Massie JP, Nolan IT, et al. (2019) Outcomes and Predictors of Revision Labiaplasty and Clitoroplasty after Gender-Affirming Genital Surgery. Plast Reconstr Surg 144: 1451-1461.
- Bucknor A, Chen AD, Egeler S, Bletsis P, Johnson AR, et al. (2018) Labiaplasty: Indications and Predictors of Postoperative Sequelae in 451 Consecutive Cases. Aesthet Surg J 38: 644-653.
- Surroca MM, Miranda LS, Ruiz JB (2018) Labiaplasty: A 24-Month Experience in 58 Patients: Outcomes and Statistical Analysis. Ann Plast Surg 80: 316-322.
- Oppenheimer AJ (2017) The Horseshoe Labiaplasty: Problems and Pearls. Ann Plast Surg 78: 286-288.
- Sharp G, Tiggemann M, Mattiske J (2016) Psychological Outcomes of Labiaplasty: A Prospective Study. Plast Reconstr Surg 138: 1202-1209.
- Sharp G, Tiggemann M, Mattiske J (2017) A Retrospective Study of the Psychological Outcomes of Labiaplasty. Aesthet Surg J 37: 324-331.
- Garcia B, Scheib S, Hallner B, Thompson N, Schiavo J, et al. (2020) Cosmetic gynecology-a systematic review and call for standardized outcome measures. Int Urogynecol J.
- Ouar N, Guillier D, Moris V, Revol M, Francois C, et al. (2017) [Postoperative complications of labia minora reduction. Comparative study between wedge and edge resection]. Ann Chir Plast Esthet 62: 219-223.
- Lista F, Mistry BD, Singh Y, Ahmad J (2015) The Safety of Aesthetic Labiaplasty: A Plastic Surgery Experience. Aesthet Surg J 35: 689-695.
- Placik OJ, Arkins JP (2015) A Prospective Evaluation of Female External Genitalia Sensitivity to Pressure following Labia Minora Reduction and Clitoral Hood Reduction. Plast Reconstr Surg 136: 442-452.
Citation: Lembo F, Cecchino LR, Parisi D, Portincasa A (2020) “What the Wom- en Want”. An Overview on Labiaplasty: Function and Beauty Researched with an Aesthetic Gynecological Procedure. J Reprod Med Gynecol Obstet 5: 053.
Copyright: © 2020 Fedele Lembo, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

