
When an Exanthem Misleads the Diagnosis: Association of Incomplete Kawasaki and COVID-19, A Case Report
*Corresponding Author(s):
Andrea CuevaMédico Residente Del Posgrado De Dermatología Universidad UTE, Mariana De Jesús, Quito 170129, Ecuador
Tel:+593-99-574-2745,
Email:a.andreacueva@gmail.com
Abstract
The association of Kawasaki disease with SARS-CoV-2 has rarely been described. It is important to identify the association, as the syndrome´s cardiac associations could be fatal. A male infant presented to Enrique Garces Hospital in Quito, Ecuador with targetoid skin lesions suggestive of a drug reaction. The patient continued with the spread of the targetoid lesions and hand-foot and mouth oedema, the primary diagnosis was Kawasaki disease, but the patient continued with respiratory symptoms, and SARS-CoV-2 test yielded positive. The patient had an excellent therapeutic response and cardiological follow-up with no findings of cardiac lesions. As new crops of mutations of COVID appear, one should think of cutaneous associations to the syndrome.
Keywords
CoVID; Case report; Exanthem; Kawasaki; Viral exanthema
Abbreviations
None.
Introduction
Kawasaki disease is a small and medium vessel vasculitis that appears most commonly in children under 5. Its cutaneous manifestations represent a diagnostic challenge due to its morphology and atypical course [1]. It is associated with viruses, bacteria and genetic factors. In children, the association of SARS-CoV-2 with multisystem inflammatory response has been reported. [2] The clinical criteria for diagnosis of classic Kawasaki disease are: fever for more than five days accompanied by b) lesions on the oral mucosa such as raspberry tongue or pharyngeal erythema, conjunctival injection without the presence of exudate, maculopapular rash, erythroderma or erythema multiform, edema in the hands and feet in the acute phase and cervical lymphadenopathy greater than 1.5 cm in diameter that is generally unilateral [3]. According to the American Heart Association and the American Academy of Pediatrics, Kawasaki disease that does not meet all clinical criteria accompanied by unexplained fever lasting more than 5 days is called incomplete disease.
Case Presentation
This is a 17-month-old male patient with a clinical history of upper respiratory infection at one year of age, which required an intensive care unit. He presented to his pediatrician with cough, odynophagia, irritability, asthenia and fever; as well as erythematous and oedematous amygdalae. He diagnosed pharyngitis and prescribed amoxicillin clavulanate for 10 days without improvement. On day 11, the patient presented typical targetoid lesions involving the palms and soles, which coalesced in a morbilliform exanthem, with no involvement of the oral mucosa (Figure 1). An adverse drug reaction was considered and the patient was treated with systemic steroids, antipyretics and antihistamines. His patient´s clinical condition worsened presenting annular erythematous plaques with a grayish macular center accompanied by periorbital and lower extremity oedema by day 13.
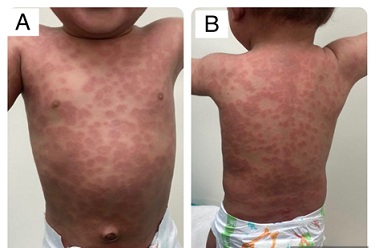 Figure 1: Generalized morbilliform exanthem.
Figure 1: Generalized morbilliform exanthem.
His test results demonstrated elevated leukocytes (26.4), neutrophils (12.36), Lymphocytes (12.9), LDH (352) Procalcitonin (85.8), D-dimer (686), and decreased haemoglobin and albumin (3.29), blood cultures were negative, and the rest of laboratory exams were normal. SARS-COV-2 antigen test turned positive, which aided in the diagnosis of incomplete Kawasaki disease as a sequel to COVID-19.
The patient´s clinical condition worsened presenting annular erythematous plaques with a grayish macular center accompanied by periorbital and lower extremity oedema by day 13 (Figure 2).
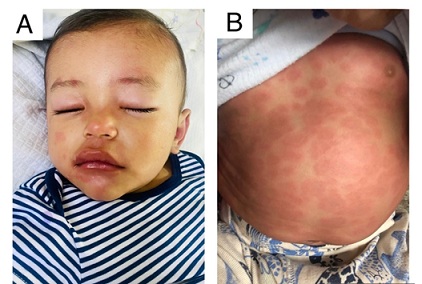 Figure 2: (A) Perioral edema (B) Annular dusky colored macules 48 hours after steroid therapy.
Figure 2: (A) Perioral edema (B) Annular dusky colored macules 48 hours after steroid therapy.
Discussion
Kawasaki disease is a self-limiting systemic vasculitis that usually occurs in children. Incomplete Kawasaki disease is defined by the presence of fever plus 2 or 3 definitory criteria, and there are reports of a greater association between incomplete Kawasaki disease with coronary aneurysms. Atypical Kawasaki disease, on the other hand, refers to the presence of symptoms not characteristic of the disease.
Several causative virus and bacteria are associated with Kawasaki disease, such as Staphylocuccus aureus toxin, Herpes virus 6, Epstein Barr virus, Leptospira sp, and recently SARS-CoV-2 [4].
Clinical signs of Kawasaki disease include changes in extremities (70% of patients) and can undergo 3 stages: first palmoplantar erythema, then indurated edema, and lastly peeling. The polymorphous exanthem is present in up to 80% of patients, could be maculopapular, scarlatiniform or erythema-multiforme like, and usually begins in extensor areas, affecting the perineal area [5]. Other, uncommon signs of Kawasaki disease are gangrene of the peripheral extremities, and transverse orange-brown pseudochromonychia due to splinter hemorrhages in the nail bed. Petechiae, crusts, and vesiculobullous lesions are uncommon [6].
Treatment is based on immunomodulation, and it should be initiated when fever lasts more than 5 days and 2 or 3 criteria is present, or fever lasts more than 7 days and severity criteria is present: PCR ≥ 3 mg/dL, ESR 40 mm/hr, 3 or more of the following: anemia, platelets ≥ 450,000, albumin ≤ 3 g/dL, elevated ALT, leukocytes ≥ 15,000/mm; or positive echocardiogram. This case highlights that Kawasaki disease can manifest with a variety of symptoms, other than those described in the diagnostic criteria, thus a high index of suspicion is important for early diagnosis and treatment.
Conflict of Interest
There are no conflicts of interest.
References
- Salamanca JYP, Ospina RDPP, Vargas JMS (2018) Enfermedad de kawasaki incompleta. Pediatría. 51: 40-42.
- Sotelo-Cruz N (2016) Atypical and incomplete Kawasaki disease in the pediatric age. Boletín médico del Hospital Infantil de México. 73: 147-148.
- Morishita KA, Goldman RD (2020) Kawasaki disease recognition and treatment. Canadian Family Physician. 66: 577-579.
- Castillo AC, Romero AC, Morales CZ, Grajales Morales AdC, et al. (2020) Enfermedad de Kawasaki y SARS-CoV-2, reporte de un caso. Alergia, Asma e Inmunología Pediátricas. 29: 52-58.
- Sánchez-Manubens J, Bou R, Prada F, Antón J (2020) Enfermedad de Kawasaki. Protoc diagn ter pediatr. 2: 213-224.
- Tessarotto L, Rubin G, Bonadies L, Valerio E, Cutrone M (2015) Orange - brown chromonychia and Kawasaki disease: a possible novel association? Pediatric Dermatology. 32: e104-105.
Citation: Andrade PC, Orbea AB, Caviedes CF, Cueva A, Bonifaz J, et al. (2024) When an Exanthem Misleads the Diagnosis: Association of Incomplete Kawasaki and COVID-19, A Case Report. J Clin Stud Med Case Rep 11:230
Copyright: © 2024 Paola Cáceres Andrade, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

