
Years of Undiagnosed Panic Disorder Finally Caught as an SVT
*Corresponding Author(s):
Zohra MalikDepartment Of Internal Medicine, Saint John’s Episcopal Hospital, New York, United States
Tel:+1 9176002733,
Email:zohrarazaq@gmail.com
Abstract
Panic Disorder (PD) is characterized by sudden attacks of intense fear with somatic symptoms such as tachycardia and palpitations. Palpitations and tachycardia can also be caused by PSVT (paroxysmal supraventricular tachycardia) and may therefore be misdiagnosed as panic disorder. A PSVT is often difficult to document on the ECG (electrocardiogram) since it has often subsided before the patient comes to medical attention and ECG abnormalities between episodes can often not be identified. In some patients with frequent panic attacks, catheter ablation was able to cure patients of their panic attacks. This evidence shows that in some patients paroxysmal SVT is the cause, but not the consequence of a panic attack. Our patient with years of undiagnosed panic disorder and all previous work-up negative finally was lucky enough to reach the diagnosis of PSVT based on ECG evidence. Patient had an episode of panic attack while visiting our hospital for her appointment. ECG was done at the time of the attack and showed PSVT. Therefore, we may hypothesize that a certain proportion of panic disorders are due to an underlying arrhythmia rather than a primary psychiatric disorder.
Introduction
Panic disorder is a type of an anxiety disorder characterized by symptoms like chest pain, dizziness, shortness of breath, heart palpitations, sweating, chills, shaking, trembling, feeling of loss of control, feeling faint, accompanied by repeated and unexpected episodes of intense fear. Per ADAA (Anxiety and Depression Association of America), 2020 statistics, around 6 million adults have panic disorders. SVT (supra ventricular tachycardia) is an abnormally fast rhythm of the heart which arises from improper electrical activity in the heart. There are four main types of SVT: paroxysmal supraventricular tachycardia (PSVT), atrial fibrillation, atrial flutter, and Wolf-Parkinson-White syndrome.
Most of the times, people spend their entire life with the label of panic disorder as SVT was never caught on their work-up. We here-by present a patient suffering from panic attacks for many years that were finally diagnosed with SVT.
Case Presentation
We hereby present case of a 59-year-old-woman with past medical history of diabetes mellitus, essential hypertension, arthritis, anxiety disorder who presented to our emergency department with an episode of perspirations and palpitations. Patient was visiting our hospital for her regularly scheduled appointment when all of a sudden she started to feel her heart beat and started perspiring and was taken to the emergency room. The patient admits to several episodes of palpitations associated with lightheadedness going back to two years. She endorses she was diagnosed with an anxiety disorder and these episodes are worsened with stress but does not describe an inciting event. The episodes occur with rest, exercise and last several minutes. She denies associated chest pain, shortness of breath, syncope, falls, fever, thyroid disorders, anemia, prior cardiac history, heavy caffeine use, alcohol use, use of illicit drugs. She takes atorvastatin, vitamin D, Lisinopril, hydrochlorothiazide and Metformin.
On presentation, the patient was alert, afebrile, with BP 118/70 mm Hg, oxygen sat 96% on room air and initial heart rate of 188 BPM (beats per minute). EKG showed SVT (Figure 1).
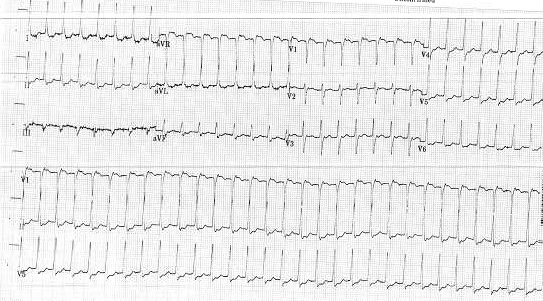 Figure 1: ECG 1: Showing PSVT.
Figure 1: ECG 1: Showing PSVT.
12-adenosine IV push was administered. Repeat EKG shows 116 bpm sinus tachycardia (figure 2). Cardizem 20mg IV push was administered. The patient reverted to normal sinus rhythm with a heart rate of 108 BPM (figure 3). Labs on presentation as shown in table 1.
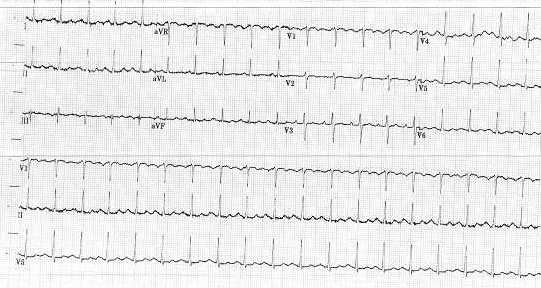 Figure 2: EKG 2: Post 12 mg Adenosine.
Figure 2: EKG 2: Post 12 mg Adenosine.
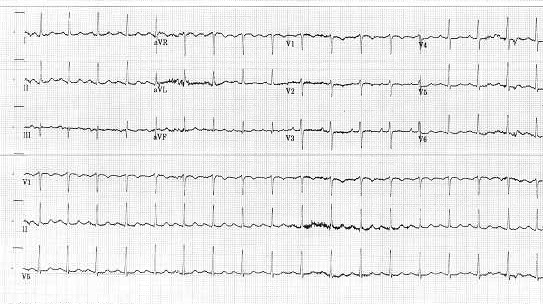 Figure 3: EKG 3: Post 20 mg Cardizem.
Figure 3: EKG 3: Post 20 mg Cardizem.
|
Laboratory |
Patient’s Value |
Normal Range |
|
WBC |
10.6 x 103/uL |
5.2-12.4 x 103/uL |
|
Hgb |
10.8 g/dL |
12.0-18.0 g/dL |
|
MCV |
92 FL |
81-99 FL |
|
Platelets |
262 x 103/uL |
130-400 103/uL |
|
INR |
1.03 units |
0.88-1.16 units |
|
BUN |
22.0 mg/dL |
7.0-17.0 mg/dL |
|
Creatinine |
0.60 mg/dl |
0.52-1.04 mg/dl |
|
Sodium |
138 mmol/L |
137-145 mmol/L |
|
Potassium |
4.2 mmol/L |
3.5-5.1 mmol/L |
|
AST |
22 U/L |
14-36 U/L |
|
ALT |
14 U/L |
4-35 U/L |
|
Total Bilirubin |
0.5 mg/dL |
0.2-1.3 mg/dL |
|
Troponin |
<0.012, 0.016, <0.012 |
0.00-0.034 |
|
TSH |
2.13 mIU/L |
0.47-4.68 mIU/L |
|
Free T4 |
1.12 ng/dL |
0.78-2.19 ng/dL |
|
|
|
|
Table 1: Labs on presentation.
Case Discussion
Tachycardia means a ventricular heart rate exceeding 100 beats per minute. Tachycardias are broadly categorized based upon the width of the QRS complex on electrocardiogram [1]. A narrow QRS complex tachycardia (<120 milliseconds), suggests rapid activation of the ventricles and this arrhythmia originates above or within the His bundle (i.e., a supraventricular tachycardia). The site of origin may be in the AV node, sinus node, the atria, or the His bundle. A widened QRS tachycardia (≥120 milliseconds), suggests ventricular activation is abnormally slow. The most common reason for a widened QRS could be that the arrhythmia originates below the His bundle in the bundle branches, Purkinje fibers, or ventricular myocardium. Alternatively, a supraventricular arrhythmia can produce a widened QRS if there are either pre-existing or rate-related abnormalities within the His-Purkinje system or if conduction occurs over an accessory pathway. Thus, wide QRS complex tachycardia’s may be either supraventricular or ventricular in origin [2].
Panic attacks are very common among our population. These panic attacks may increase the risk of other psychiatric diseases and increase visits to the clinic and emergency departments [3]. Patient has a feeling of impending doom and therefore undergoes diagnostic tests and procedures to rule out somatic origin of their disorder [3]. Supraventricular Tachycardia (SVT) is the heart arrhythmia most likely to be mistaken for a panic attack. It can make heart beat as much as 150 to 250 times a minute. One of the similarities between both panic attacks and SVT is the rapid action of the heart [4]. In PSVT, ECG may be completely normal or nearly normal. If an ECG is taken exactly during the attack, the diagnosis is simple since, besides the rapid heart action often at rates of 160 to 180 beats/min, there is no longer the normal activation of the heart with a P wave followed by the QRS complex but the P wave is mostly hidden within the QRS complex. In a panic attack, the rapid heart action is due to an increased sympathetic drive, which leads to an increase in sinus rate, with the sequence of the P, and QRS being maintained [4].
Our patient was able to achieve a clear diagnosis as the panic attack occurred in a hospital setting and was caught on the ECG as SVT. This case is unique as the patient was living under the diagnosis of panic disorder instead of a rhythm disorder. Sometimes 12-lead ECG is not enough in diagnosing an SVT. Smartphone-based ECG is another modality for accurately detecting atrial rate and rhythm [5,6]. Long-term ECG recorders, patient-activated ECG recorders or implantable loop recorders [4] can achieve an improved documentation of the ECG during an attack. Correlation of symptoms with Holter monitoring is crucial for a precise diagnosis [7].
For management of PSVT, there are physical maneuvers like Valsalva maneuver, medications such as adenosine, diltiazem, verapamil or anti-arrhythmic drugs such as sotalol or amiodarone. If a person is hemodynamically unstable or other treatments are not effective, synchronized electrical cardioversion may be used [8].
Conclusion
Panic attacks and SVT frequently present with similar clinical presentation. Without electrocardiographic evidence of SVT, it sometimes can be difficult to distinguish between the two. Rather than putting a label of a primary psychiatry disorder on patients who are being treated for an anxiety disorder and panic attacks, we need to evaluate them further for an underlying arrhythmia. An adequate diagnosis and proper treatment of SVT is important to stop the chronic process and to enhance the quality of life of the patient.
Conflict of Interest
The authors declare they have no conflict of interest.
References
- Ganz LI, Friedman PL (1995) Supraventricular tachycardia. NEJM 332: 162-73.
- Ganz L, Knight BP, Goldberger AL, Hoekstra J, Dardas TF (2021) Narrow QRS complex tachycardias: Clinical manifestations, diagnosis, and evaluation.
- Katon WJ, Korff MV, Lin E (1992) Panic disorder: relationship to high medical utilization, unexplained physical symptoms, and medical costs. J Clin Psychiatry 57: 8-11.
- Frommeyer G, Eckardt L, Breithard G (2013) Panic attacks and supraventricular tachycardias: the chicken or the egg? Netherlands Heart Journal 21: 74-77.
- Haberman ZC, Jahn RT, Bose R, Tun H, Shinbane JS, et al. (2015) Wireless smartphone ECG enables large-scale screening in diverse populations. Journal of Cardiovascular Electrophysiology 26: 520-526.
- Tarakji KG, Wazni OM, Callahan T (2015) Using a novel wireless system for monitoring patients after the atrial fibrillation ablation procedure: the iTransmit study. Heart Rhythm Society 12: 554-559.
- Thavendiranathan P, Bagai A, Khoo C (2009) Does this patient with palpitations have a cardiac arrhythmia? JAMA 302: 2135-2143.
- https://en.wikipedia.org/wiki/Paroxysmal_supraventricular_tachycardia#Treatment
Citation: Malik Z, Razaq Z, Shamail S, Daniel B (2020) Years of Undiagnosed Panic Disorder Finally Caught as an SVT. J Surg Curr Trend Innov 5: 047.
Copyright: © 2021 Zohra Malik, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

