Congenital Ejaculatory Ducts Obstruction by Wolffian Duct Cyst: A Case Report
*Corresponding Author(s):
Lucas Loiola Ponte Albuquerque RibeiroMedical Student, Universidade De Fortaeza, Brazil
Tel:+55 8534773676,
Fax:+55 85998579944
Email:lucaspontelol@edu.unifor.br
Abstract
The infertility in relationships affects 15% of couples and the male’s causes are responsible for 45% of this problems. The ejaculatory ducts obstruction are a very rare cause of infertility and must be investigated when the sperm analysis shows a persistently decreased ejaculatory volume.
In this case report, the patient presents with genital pain of low-middle intensity, worsen by the ejaculation. By two years, he was trying to have children's, without success. In the first medical evaluation, the patient showed a recent sperm analysis that reveal azoospermia and hypospermia. In the physical exam, was noticed epididymis and vas deferens congestion, with a normal testicle volume. A second sperm analysis was requested and showed a low fructose and normal hormones levels. The alterations of the first analysis continued. A transrectal ultrasonography was done and reveals a distension of the seminal vesicles and a cyst in the central area of the prostate gland. The diagnosis of ejaculatory ducts obstruction was confirmed by a bilateral vasography. The patient was submitted for a transurethral resection of the prostatic cysts anterior wall.
Keywords
INTRODUCTION
The Ejaculatory Duct Obstruction (EDO) can be separated in congenital and acquired causes. The acquired causes are secondary of trauma, infections or inflammation states. Calculi due to infections can also cause obstruction. In the congenital etiologies, we have congenital atresia or stenosis of ejaculatory duct and cyst with source in Müllerian or Wolffian ducts [3].
We report a case of a young man that searched the urology department complaining about primary couple's infertility, decreased ejaculatory volume and pain in genital area. After medical research, the diagnosis of EDO was confirmed.
CASE REPORT
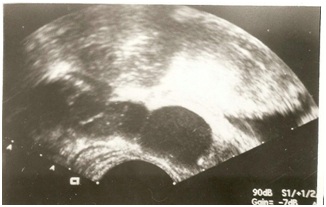 Figure 1: Transrectal ultrasonography of the prostate gland with seminal vesicles distension.
Figure 1: Transrectal ultrasonography of the prostate gland with seminal vesicles distension. Figure 2: Transrectal ultrasonography of the prostate gland shows a cyst in the prostate gland central area, with 1,8 cm of diameter, compatible with cyst due the remaining of the Müllerian duct.
Figure 2: Transrectal ultrasonography of the prostate gland shows a cyst in the prostate gland central area, with 1,8 cm of diameter, compatible with cyst due the remaining of the Müllerian duct.The diagnosis of EDO was made. The patient was taken to surgical center and received spinal anesthesia to do a vasography by puncture with injection of iodine and methylene-blue-impregnated contrast. The exam shows that the contrast was deposited in the interior of the prostatic cyst (Figure 3). In the same act, the patient was submitted for a transurethral resection in the roof of the prostatic cyst, that was localized under the bladder neck, with observation of methylene-blue contrast leakage. Afterwards, the patient lost the follow-up.
 Figure 3: Vasography with the prostatic cyst and seminal vesicles filled with iodinated contrast.
Figure 3: Vasography with the prostatic cyst and seminal vesicles filled with iodinated contrast.DISCUSSION
From embryology, the vas deferens develops from Wolffian duct system. They are 1-2 cm in length and enter the prostate gland obliquely and posterior to the base,and then course medially and anteriorly through the prostatic glandular tissue, eventually opening into the prostatic urethra at the verumontanum as slit-like orifices [1,3].
The symptoms may vary, including the asymptomatic presentation. Besides infertility, decreased force of ejaculation (more common), pain during or after ejaculation, perineal or testicular pain related to ejaculation, history of symptoms suggestive of prostatitis or epididymitis, lower back pain, dysuria, urinary obstruction and hematospermia are related. In patients with partial obstruction, the symptoms are typically less pronounced. However, no single symptom can make the diagnosis of EDO [3,6].
In the medical examination of the infertile men, the anamnesis is done followed by a complete physical exam. In the genital examination, the testicles volume, the presence of duct deferens and epididymis must be evaluated. If in doubt about this pathology, in the digital rectal exam, the examinator can touch the seminal vesicles and notice a prostatic cyst [7].
The sperm analysis is the standard exam to assess a infertile men. This exam analyze the pH, ejaculatory volume and the concentration, mobility and morphology of the sperm cell [6].
In EDO, the decrease of the ejaculatory volume (<1,5ml), azoospermia or oligospermia, acidic pH and absence of fructose are observed [2]. The levels of Follicle-Stimulating Hormone (FSH) and total testosterone are normals 4.
In cases suspect of EDO, the TRUS can reveal inflammatory signs or cystic structures intra or periprostatic, that can be better visualized by CT scan or MRI [7,8]. The vasography was considered the gold standard for EDO diagnosis but, due to being invasive and have increased risk of complications, the ultrasonography is now the standard exam [4,5]. Echographic findings in patients with EDO are cysts in the central line of the prostate gland and distension of the seminal vesicles or the ejaculatory ducts [5].
The standard treatment of EDO is the surgical transurethral resection. The approach consists in superficial resection in the midline of verumontanum, with improvement of the symptoms and pregnancies taxes that can be close to 29% [3].
Previously published data have shown improvement of semen parameters in 50-65% of cases and spontaneous pregnancy in 20-30% of cases after surgical treatment [9]. Improvement of sexual satisfaction, by the increased ejaculatory volume, are also related by the patients [6].
In this case, the prostatic cyst was localized in the midline of the prostate gland and proximal to verumontanum, under the bladder neck. This location and the cyst filling with contrast, showing a communication between the ejaculatory ducts, suggest Wolffian cyst [5,10]. The patient was treated with transurethral resection of the cyst wall with protection of the bladder neck.
The first surgical description to treat this pathology was made in 1973 by Farley and Barnes, remaining as gold standard until nowadays. It consists in transurethral resection of the cyst wall with a strap attached to an electric scalpel [5,6,8,10].
Post-surgical complications affect approximately 13-26% of patients. In the immediate postoperative period, epididymitis and macroscopic hematuria can occur, that require vesical catheterization. At a later stage, sperm change in consistency, azoospermia and urinary reflux to the interior of prostate gland can be present [5,10].
CONCLUSION
REFERENCES
- Tanagho Emil A, Mcaninch Jack W (2010) Urologia geral de smith. (17th edn). McGraw Hill, Brasil Pg no: 756-797.
- Johnson CW, Bingham JB, Goluboff ET, Fisch H (2005) Transurethral resection of the ejaculatory ducts for treating ejaculatory symptoms. BJU International 95: 117-119.
- Fisch H, Lambert SM, Goluboff ET (2006) Management of ejaculatory duct obstruction: Etiology, diagnosis, and treatment. World J Urol 24: 604-610.
- Tu XA, Zhuang JT, Zhao L, Zhao LY, Zhao JQ, et al. (2013) Transurethral bipolar plasma kinetic resection of ejaculatory duct for treatment of ejaculatory duct obstruction. J Xray Sci Technol 21: 293-302.
- Modgil V, Rai S, Ralph DJ, Muneer A (2016) An update on the diagnosis and management of ejaculatory duct obstruction. Nat Rev Urol 13: 13-20.
- Johnson CW, Bingham JB, Goluboff ET, Fisch H (2005) Transurethral resection of the ejaculatory ducts for treating ejaculatory symptoms. BJU International 95: 117-119.
- Jungwirth A, Diemer T, Dohle GR (2018) EAU Guidelines. (edn). Presented at the EAU Annual Congress Copenhagen.
- Abdel Raheem, Luca F De, Muneer A, Ralph D (2016) Presentation and treatment outcome of ejaculatory duct obstruction (EDO). J Sex Med 13: 263-265.
- El-Assmy A, El-Tholoth H, Abouelkheir RT, Abou-El-Ghar ME (2012) Transurethral resection of ejaculatory duct in infertile men: Outcome and predictors of success.Int Urol Nephrol 44: 1623-1630.
- Sangster, Pippa (2017) Presentation and treatment outcomes of ejaculatory duct obstruction.
Citation: de Souza IT, Ribeiro LLPA, Pinheiro AM, Pinto GP, Teixeira GC, et al. (2019) Congenital Ejaculatory Ducts Obstruction by Wolffian Duct Cyst: A Case Report. Arch Urol 2: 005.
Copyright: © 2019 Ivon Teixeira de Souza, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.