ABSTRACT
Background: The concept of ‘Five Moments for Hand Hygiene’ described in the WHO Guidelines on Hand Hygiene in Health Care, defines the key moments when health-care workers should perform hand hygiene in order to break the transmission of infectious organism via the hands. The concept stipulates that healthcare workers perform hand hygiene before touching and after touching a patient, before sterile or aseptic procedure, after touching patients’ environment and after exposure to blood or body fluids. Although hand hygiene is recognized as the most effective measure for preventing the transmission of infections in healthcare settings compliance with hand hygiene among Healthcare Workers (HCWs) remains unsatisfactory.
Objective: To determine compliance with hand hygiene among healthcare workers based on the ‘five moments’ concept.
Methodology: In this observational descriptive study, one hundred and fifty four HCWs in five randomly selected wards of a tertiary hospital were covertly observed for compliance with five moments for hand hygiene over a period of two weeks.
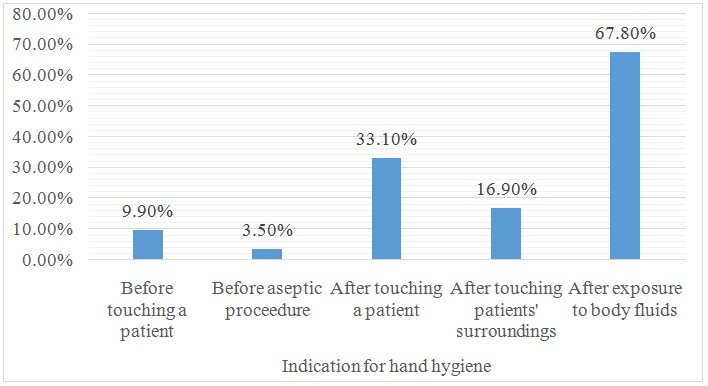
Results: A total of 718 opportunities for hand hygiene were observed with an overall compliance of 23.5%. Compliance was highest after exposure to blood/body fluids (67.83%) and lowest before aseptic procedures (3.5%). It was 9.9%, 33.1% and 16.9% for before touching, after touching and after touching patients’ surrounding respectively.
Conclusion: Overall hand hygiene compliance was low. Compliance was higher in the ‘after’ than in the ‘before’ moments for hand hygiene. Therefore hand hygiene compliance before any patient contact should be emphasized.
KEYWORDS
Compliance; Five moments; Hand hygiene
Introduction
The act of hand rubbing with an alcohol-based antiseptic solution or hand washing with soap and water with the aim of reducing or inhibiting the growth of micro-organisms on the hands is referred to as hand hygiene [1]. For several decades hand hygiene has been known to be a very simple and effective measure for preventing Healthcare Associated Infections (HCAIs) [2-6], but compliance with recommended standards for hand hygiene among Healthcare Workers (HCWs) has not been satisfactory globally [7]. Studies in Nigeria have also shown that hand hygiene compliance among Nigerian HCWs is very poor [8,9]. The implication of this is high prevalence of HCAIs with associated increase in morbidity, mortality and cost of healthcare in a country battling with a high burden of preventable infectious diseases. This further dashes any hope of improving patient safety in an already weak health systems.
In order to improve compliance with hand hygiene as well as provide a solid basis to understand, teach, monitor and report hand hygiene practice, the World Health Organization (WHO) in collaboration with some patient safety and infection control experts developed a concept referred to as ‘Five Moments for Hand Hygiene’ [7,10]. This concept defines key moments during routine patient care activities when hand hygiene is required to stop transmission of infectious organisms via the hands in healthcare settings [1]. It represents a shift from the traditional ‘two moments’ view of hand hygiene which emphasizes hand hygiene immediately before and at the end of patient care activity. The traditional view is an oversimplification of hand hygiene and practically may not be as effective as the ‘five moments’ approach in preventing HCAI when applied. This is because the hands can be contaminated during the process of care making it possible to transmit pathogens from a colonized to a sterile body site on the same patient. According to the ‘five moments’ concept, healthcare workers should perform hand hygiene ‘before touching a patient’, ‘after touching a patient’, ‘before any sterile or aseptic procedure’, ‘after touching patient’s environment’ and ‘after exposure to blood or body fluids’ [10]. The “before” moments are aimed at preventing the risk of transmitting pathogens to the patient and from one body site to a sterile site on the same patient while the “after” moments are intended to prevent transmission of pathogens from the patients to the healthcare worker, the healthcare environment, and other patients. Several studies on hand hygiene in healthcare setting have simply and broadly described compliance in terms of before and after patient care activity [9,11,12]. This approach falls short of describing the most important and critical indications for hand hygiene during the sequence of care. This study was designed to study compliance with hand hygiene with a view of describing compliance with each of the key moments for hand hygiene during routine patient care activity.
Methodology
This descriptive study was conducted in a government-owned multidisciplinary tertiary hospital in Umuahia the capital city of Abia State in the South East geopolitical zone of Nigeria. The hospital is also an accredited centre for the training of specialist doctors and serves an area with a population of over one million people.
The study population consisted of 154 Healthcare Workers (HCWs) who were doctors and nurses providing care to patients on admission in five out of seventeen wards in the hospitals. The list of the HCWs was obtained from the duty roster provided in the five wards. All of them were directly and covertly observed for compliance with five moments for hand hygiene while providing care to patients on admission during the study period. The five wards were selected by stratified random sampling.
Data on hand hygiene compliance was collected using the World Health Organization’s hand hygiene observation form [13] unmodified. Five junior resident doctors were recruited as hand hygiene observers and trained on how to use the observation form. The training entailed a two day intensive seminar and practical sessions on how to recognise and record the moments (or opportunity) for hand hygiene on the form in one of the hospital wards. After the training exercise, one observer was assigned to each of the wards used for the study. The observers conducted three (morning, afternoon and evening) observation sessions per day in each of the ward over a period of two weeks in the August 2012. Each observation session lasted for 20-30 minutes and was done covertly to minimize Hawthorne effect [14].
An opportunity for hand hygiene was defined as the period between the moment a HCW’s hands touched any surface in the healthcare area and the moment in which the same hands touched a receptor surface during a healthcare activity while an indication for hand hygiene was the reason(s) that motivate(s) hand hygiene action [1,7]. At least one indicator for hand hygiene defined an opportunity to perform hand hygiene. HCW’s hands were presumed to be potentially contaminated before any healthcare activity and were therefore expected to perform hand hygiene before any contact with the patient. This criterion also defined an opportunity for hand hygiene. Hand hygiene actions were categorized as either missed, hand washing or hand rubbing. Antiseptic hand rubbing using an alcohol-based hand sanitizer or hand washing with soap and water when an opportunity for hand hygiene presented, was considered appropriate hand hygiene action. Only hand hygiene actions taken at the point-of-care were recorded with exception of those indications for hand hygiene that required hand washing with soap and water since there were no sinks on each bedside. Any hand hygiene action taken outside the point-of-care was considered as a missed opportunity but whenever a HCW left the point-of-care to use soap and water when indicated, it was recorded as appropriate hand hygiene action.
All data collected were entered and analyzed using Epi Info version 3.5.3. Overall hand hygiene compliance (in percentage) was calculated by dividing the total number of recorded hand hygiene actions by total opportunities for hand hygiene and multiplied by 100% [1]. Hand hygiene compliance was also computed for each professional group and compared. Chi squared test was used to test the differences in proportion of the categorical variables. Statistical significance was defined as a P-value of less than 0.05. Simple frequency distribution was used to describe variables. Ethical clearance for the study was obtained from the hospital research and ethics committee
Results
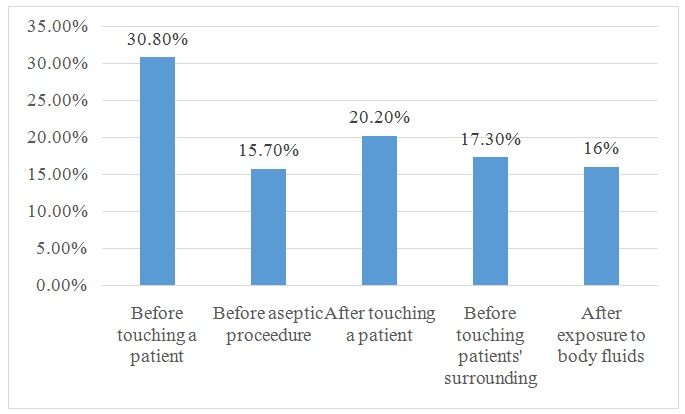
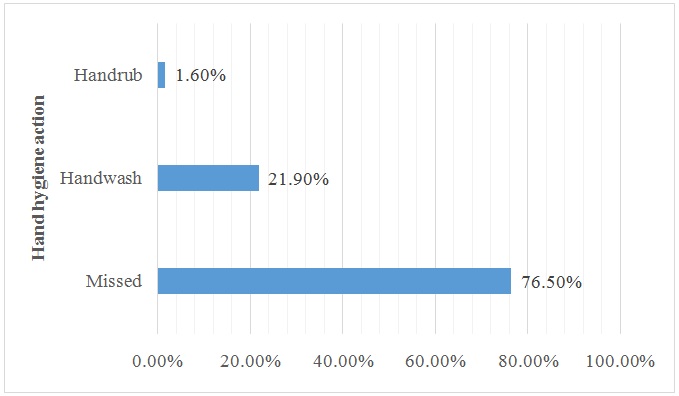
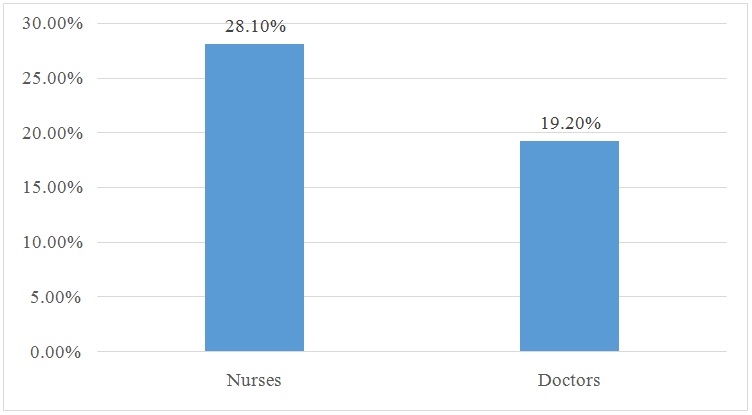
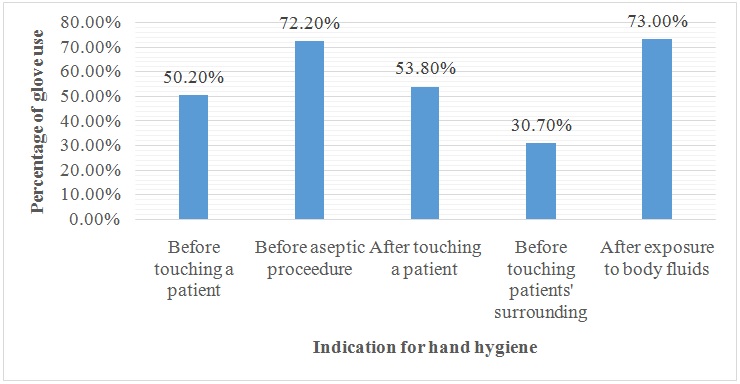
A total of 718 opportunities for hand hygiene were observed. The opportunities were fairly distributed among the professional groups-doctors (50.8%) and nurses (49.2%). Figure 1 shows that ‘before touching patient’ (30.8%) and ‘after touching patient’ (20.2%) indications for hand hygiene were the most observed compared to the other three indications- ‘before aseptic or sterile procedure’ (15.7%), ‘after touching patients surrounding’ (17.3%), and ‘after exposure to blood/body fluid’ (16.0%). Of the 718 opportunities recorded, 169 (23.5%) appropriate hand hygiene actions were observed while 549 (73.5%) were missed. It was also observed that hand rubbing with an alcohol-based hand sanitizer constituted only 1.6% of all hand hygiene actions (i.e., hand washing, hand rubbing and missed). This is depicted in figure 2. Of the 169 appropriate hand hygiene actions we observed, hand washing with soap and water was predominant (92.9%) while antiseptic hand rubbing constituted only 12 (7.1%). Figure 3 shows that compliance with hand hygiene was highest (67.83%) after the study participants engaged in any healthcare activity that potentially exposed them to blood/body fluids and lowest (3.5%) before they performed aseptic procedures e.g., setting up an intravenous line. When we compared the frequency of appropriate action taken when hand hygiene was indicated for doctors versus nurses, we found that nurses were more compliant than doctors (28.1% versus 19.2% respectively). This was statistically significant (p=0.006) (Figure 4). Table 1 shows the distribution of the observed opportunities for hand hygiene in each of the five wards and the corresponding frequency of compliance (appropriate hand hygiene action taken). The level of compliance was as follows- accident and emergency (19.2%), female medical ward (28.3%), male medical ward (23.9%), female surgical ward (25.5%) and orthopaedic ward (21.0%). The observed differences was not statistically significant (p=0.386). Glove use when indicated constitutes good hand hygiene practice. Data collected on glove use revealed that gloves were worn in more than half of the total observed opportunities (393 out of 718) and the missed opportunities (53.4%) for hand hygiene. In the “before touching patient” indication for hand hygiene, gloves were worn in approximately 50% of the opportunities observed (Figure 5).
Discussion
The process of providing care to a patient on hospital admission at the point-of-care is both complex and unpredictable. Integrating standard hand hygiene practice into this process is even more challenging since most HCWs will traditionally perform hand hygiene after completing the task of caring for a particular patient. Our attempt to study HCW’s workers compliance with hand hygiene based on ‘my five moments’ concept gave us insight into the state-of-the-practice in a typical tertiary hospital in a resource constraint setting.
The overall compliance was low (23.5%) a finding that is similar to what has been observed among HCWs in some developed and less developed countries [7,9,15,16]. When we considered compliance with respect to individual moments for hand hygiene, compliance was higher in the ‘after moments’ compared to the ‘before moments’. For instance, figure 5 show that compliance with ‘before aseptic procedure’ was only 3.5% while ‘after exposure to blood/body fluid’ was 67.8%. Infection control experts generally agree that the main benefit of hand hygiene before contact with a patient is prevention of transmission of potential HCAI pathogens to the patient while hand hygiene after contact with a patient (and/or his environment) is protection of HCWs from becoming colonized by HCAI pathogens [10,17]. The observed higher compliance with the ‘after moment’ suggests that most HCWs in this study may have performed hand hygiene for self-protection rather than safety of the patient. In their study Borg MA et al., also observed that self-protection is potentially the main reason why HCWs perform hand hygiene [18]. When healthcare workers perform hand hygiene only for self-protection without considering the safety of the patients, the whole essence of hand hygiene in the healthcare setting is defeated.
Another important and salient observation was the method of hand hygiene HCWs in this study applied when they complied. In spite of the global acceptance of antiseptic hand rubbing using an alcohol-based solution as a safe, east-to-use and effective method of hand hygiene, [7,19-21] the use of AHR by HCWs in this study was suboptimal as depicted in figure 2. Possible reasons for this are unavailability of the product and lack of awareness among the HCWs. In healthcare settings it is easier to mount and maintain AHR than to install water tap and sink on each bedside. It is also possible for HCWs to carry their personal AHR as they go about their duties. Bedside-mounted AHR and pocket carried AHR make it easier for HCWs to perform hand hygiene at the point-of-care without the need to leave the patient area [7]. We observed that in this hospital setting, there were no bedside-mounted AHR or water tap and sink. The location of the facility for hand washing in each ward was far from patient’s bedside and since HCWs in this setting predominantly used soap and water for hand hygiene (Figure 2), the risk of missed opportunities for hand hygiene was very high. This may be a possible explanation for the low compliance with hand hygiene observed in this study.
Several studies have reported that nurses comply with hand hygiene more than doctors [22-25]. We observed a similar trend in this study (Figure 3). The implication of this in hospital infection should be seriously considered. While nurses may have more contact with patients than doctors in the hospital, doctors perform more invasive procedures than nurses thereby increasing the risk of transmission of HCAI pathogens by doctors when they fail to perform hand hygiene.
Generally, gloves were worn by study participants in more than half of all observed opportunities for hand hygiene- 393 out of 718 opportunities but most of them failed to remove their gloves when it was indicated during patient care activity. In most instances, the same pair of gloves was used to perform multiple tasks or attend to several patients. The fact that gloves are not indicated in the “before touching a patient” moment for hand hygiene except for contact precautions [17], the observed high utilization of gloves ‘before touching a patient’ indicates that there was inappropriate use of gloves by the study participants. Use of gloves is known to prevent transmission of infectious organism in healthcare settings but inappropriate use of gloves is equivalent to no hand hygiene. We also observed a high number of missed opportunities when gloves were worn suggesting that the use of gloves had a negative impact on hand hygiene compliance. This is similar to what has already been documented [17].
Conclusion
We conclude that the overall compliance was low among HCWs in this study. However, it was highest after exposure to blood/body fluids (67.83%) and lowest before aseptic procedures (3.5%). Nurses were more compliant than doctors while low utilization of AHR and inappropriate use glove may have been the key factors responsible for the poor compliance. In the light of the foregoing we recommend that interventions to promote ‘five moments’ for hand hygiene should ensure the provision of AHR at patient’s bedside, emphasize hand hygiene before any patient contact, behaviour change among doctors, promote the use of AHR and proper use of gloves.
Figures
Figure 1: Distribution of Indications for Hand Hygiene.
Figure 2: Action Taken By Study Participants whenever Hand Hygiene Was Required During Patient Care Activities.
Figure 3: Frequency of Compliance (Appropriate Hand Hygiene Action) For Each Indication for Hand Hygiene.
Figure 4: Hand Hygiene Compliance of Doctors and Nurses.
*p=0.006
Figure 5: Indications for Hand Hygiene and Corresponding Frequency of Use of Gloves by the Hcws.
Tables
| Wards | Opportunities (%) | Compliance (%) |
| Accident & Emergency | 146 (20.3) | 28 (19.2) |
| Female medical | 145 (20.2) | 41 (28.3) |
| Orthopaedic | 143 (19.9) | 30 (21.0) |
| Female surgical | 142 (19.8) | 36 (25.5) |
| Male medical | 142 (19.8) | 34 (23.9) |
| Total | 718 (100.0) | 169 (23.5) |
Table 1: Distribution of Opportunities for Hand Hygiene in Each Ward and Corresponding Compliance (Appropriate Hand Hygiene Action).