Introduction
Lower extremity amputations are performed for numerous reasons including: trauma, vascular disease, infection, malignancy, and congenital deformity. It is a commonly performed procedure; in 2005 approximately 185,000 people underwent lower extremity amputation in the United States, with that number expected to grow substantially by 2050 [1]. Estimates indicate that 1.6 million Americans in 2005 were living without a limb, which is approximately 1 in every 190 Americans [1]. Although the indications for amputation vary significantly the goals remain uniform: preserve as much limb length as safely as possible that will result in a functional residual limb.
Determining the level of amputation is difficult as balancing length, the status of the proximal joint, evaluating the soft tissue envelop, and estimating osseous prominences can be a complex decision making process. In the landmark article from 1976, Waters was the first to document increased gait velocity and decreased energy expenditure when comparing transtibial to transfemoral amputees [2]. He also noted that patients undergoing amputation for different procedures had different results; amputees from trauma out-performed amputees from vascular disease. Literature published around the same time reported that compared to similar able-bodied individuals those with amputations had a significantly higher energy expenditure with ambulation, even on a level surface [3]. Transfemoral amputees recorded 65% higher energy expenditure when compared to able-bodied individuals [4]. More recent literature supports these theories by showing that amputees have slower average walking speeds (21%) compared to able-bodied individuals as well as higher aerobic demands at paced speeds (55%-83%). It is thought that an above average amount of energy is spent on posture and balance in addition to the added cost of ambulation [5]. The more proximal and amputation the more energy the body spends on posture and balance, thus increasing the complexity of post-operative rehabilitation and ambulation with or without prosthesis.
Caring for the amputee is best performed by a team of medical specialists each with their own knowledge and area of expertise. While the surgeon performs the operation and removes the limb, most of the principal medical treatment occurs after the wound has healed and is given by physical medicine and rehabilitation physicians, prosthetists, physical therapists, and psychiatrists. Involving these team members pre-operatively facilitates surgical planning by discussing the level of amputation, prosthesis design, physical therapy protocol, and mental health management and can be customized to each individual patient.
Surgical Principles
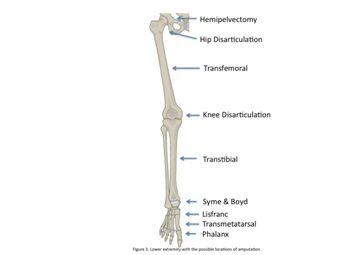
The lower extremity has a myriad of locations where amputation is an option (Table 1); the most common lower extremity amputation is the transtibial while the least is the transpelvic amputation [6]. Proximal lower extremity amputations, the hemipelvectomy and hip disarticulation, have an extremely high mortality rate, reported as high as 50% [7]. Advances in anesthesia and surgical technique have drastically decreased these numbers to 0-10% [8].
Transfemoral
Transfemoral amputations have seen an improvement in surgical ideology over time. Traditionally, according to the general and vascular surgery literature, muscle transection when performing this procedure can be done without any stabilization. Contrary to that, orthopedic principles indicate that when performing a transfemoral amputation a myodesis is to be performed to limit the likelihood of developing a flexion or abduction contracture (Figure 1). With either contracture the amputee would be unable to generate sufficient power to manipulate prosthesis [9]. When performing the adductor myodesis, the hip must not be flexed as this would create an iatrogenic flexion contracture that would only complicate post-operative rehabilitation. Maximizing length in the extremity assists patients with transfers and sitting. A long posterior skin flap with adequate muscle coverage over the beveled femoral diaphysis and adductor myodesis allows for a cosmetic residual limb that is amenable to prosthesis fitting and eventual ambulation.
Previously aforementioned techniques are unnecessary when performing a knee disarticulation as femoral alignment and length are undisrupted. For all disarticulation procedures, including the knee, transfer of weight bearing is distributed through the metaphyseal bone over a large surface area. This is in contrary to a transosseous amputation that requires a thick, mobile, robust soft tissue envelope to cushion the highly concentrated shear forces seen with ambulation [10]. When fitting a patient with the prosthesis following an amputation, the prosthetist must be aware of whether the procedure were a transosseous or disarticulation procedure to ensure the prosthesis is constructed appropriately to distribute force throughout the limb. Incorrect force distribution can lead to ulcers, wound compromise, and ultimately a need for revision to a more proximal amputation.
Transtibial
Transtibial amputation is the most commonly performed major limb amputation. Many of the patients have a realistic chance to ambulate post-operatively; the literature quoted varies from 17%-77% [11-14]. The transtibial amputation is not for every patient, those critically ill, debilitated, spastic, or currently with a knee flexion contracture will end up with a poor outcome because of an inability to transfer or sit. A more proximal knee disarticulation results in better outcomes in the spastic patient population. Various incisions have been described for the transtibial amputation, however, the long posterior myocutaneous flap has been proven to have good outcomes with few wound complications and a high likelihood of post-operative ambulation [15]. The ideal length for a transtibial amputation is to make the tibia osteotomy approximately 12 cm to 18 cm from the tibia tubercle [16]. Depending on whether the Ertl technique will be employed, which supporters argue improves weight distribution in the residual limb, the fibula osteotomy is performed either 4 cm distal to the tibia osteotomy to allow for fibular bone bridge creation, or 1 cm to 2 cm proximal to it. In a recent retrospective review, Brown et al., indicate that those patients undergoing the Ert l procedure had a higher rate of post-operative wound complications compared to those without the bone bridging part of the procedure [15]. A key component of the transtibial amputation is the myodesis, similar to the transfemoral amputation, however this involves tacking the soleus to the anterior tibial cortex through cortical drill holes. When the long posterior myocuteanous flap is delivered anterior, the muscle bulk of the posterior compartment pads the distal end of the residual limb while simultaneously moving the wound from the prosthesis-residual limb weight bearing interface. An appropriately designed flap has minimal “dog ears” and is nicely tapered to optimize the fit for the prosthesis (Figure 2).
Syme and boyd
The Syme amputation is a disarticulation of the tibio-talar joint with removal of the malleoli. Historically this surgical procedure was performed in 2 stages. The first stage involves disarticulation at the ankle and 6 weeks later osteotomy of the malleoli at the level of tibia plafond. More recent literature indicated the procedure could safely be performed in a single stage [17]. Criteria to have the Syme amputation include: ability to walk with a prosthesis following surgery, viable heel pad without infection, and enough vascular inflow to support wound estimated by ankle-brachial-indices > 0.5 in diabetics and 0.45 in non-diabetes [18-19]. A key component in quality outcomes after Syme amputation is a modification that attaches the heel pad to the distal tibia thus preventing migration and complicated prosthesis fitting [20]. Distal to the Syme amputation exist numerous options for treating forefoot and mid foot problems requiring amputation. The Boyd amputation is one option. A Boyd amputation requires disarticulation of the tibiotalar joint with excision of the malleoli, however, what makes it unique from the Syme amputation is the calcaneus is osteotomized and fixed to the tibiotalar joint with screws. Similar to the Syme amputation, it allows for ambulation without a substantial increase in energy expenditure compared to controls; however it is not a simple procedure [2].
Mid-foot and distal
Additional disarticulation options exist anatomically between the syme amputation and the transmetatarsal amputation: the tarsal (Chopart) and the tarsometatarsal (Lisfranc) disarticulations. These are infrequently performed because of the numerous complications including wound healing and equinovarus deformity [21]. The transmetatarsal amputation is a slightly more distal amputation than the Lisfranc and is performed in a similar manner with a long plantar skin flap. Only difference between the two is the bone cuts that are made in the proximal metatarsal metaphysis instead of tarsometatarsal disarticulations. Transmetatarsal amputation is a great amputation option for forefoot pathology as it maximizes length, is cosmetic as it allows for regular shoe wear without prosthesis, and promotes independent ambulation [22]. Literature indicates that candidate selection is paramount or else revision procedures resulting in more proximal amputation [23]. Partial amputations of the forefoot including ray resections and toe amputations are twice as common in the United States than transtibial or transfemoral amputations [24]. Maintaining length with ray resection and digit amputation is vital as with all other amputations, however what is most important is ensuring adequate resection of the infected or ischemic digit or ulcer. A retrospective review from 2013 reports a 42.4% incidence of proximal amputation following ray resection or toe amputation [25]. Additionally, the authors report that approximately 70% of patients will return to the office with new ulcerations, wounds requiring antibiotics, or have ancillary procedures done on the operative extremity [25]. Therefore, given the patient population being treated with this surgical procedure and the likelihood of proximal progression some surgeons argue a more proximal amputation may be indicated as the index and final procedure.
Other principles
Gentle soft tissue handling is paramount when performing any lower extremity amputation, but this becomes even more vital the more distal the amputation. Long posterior soft tissue flaps without compromised blood supply are vital to successful healing of the knee disarticulation, a trans-femoral amputation, a transtibial amputation, a syme amputation and nearly all amputations distal to the hind foot. One long posterior skin flap is advantageous as it moves the incision from the end of the extremity, thus decreasing the contact it has as the weight-bearing portion of the limb and the possibility for breakdown.
While closing the amputated limb, surgical drains are often left in place to decrease the deep space for fluid collection in the newly formed extremity. Literature on drain placement following amputation surgery is controversial with a recent study from 2012 suggesting that placing a drain, especially in diabetic patients, is associated with an increased risk of post-operative complication from infection [26]. As with all other surgical procedures peri-operative antibiotics should be given intravenously to the patient to decrease the risk of infection post-operatively [27]. Once closed, the wound is often dressed sterile with a non-adhesive gauze, dry gauze, abdominal pads, and wrapped tightly with a circumferential All Cotton Elastic (ACE) wrap. The tight circumferential ACE wrap protects the wound while simultaneously controlling post-operative edema. Soft versus soft and hard dressings are controversial with the benefit of the stiffer immobilization prohibiting post-operative contractures, such as knee flexion following transtibial amputation. Physiotherapy literature indicates that transtibial amputees who had removable rigid dressings placed post-operatively experienced shorter times to initial prosthetic casting and independent walking [28]. However, the independent ambulation benefits come at the cost of possibly compromising the soft tissue envelope, as a rigid dressing may irritate the skin around the wound.
Pain management in lower extremity amputation is multifarious. Amputees are known to have various type of pain with different mechanisms of action, thus it is important to differentiate them, as they require distinctive modalities for management. Phantom Limb Pain (PLP), the sensation of pain in the amputated limb, and Residual Limb Pain (RLP), sensation of pain in the residual limb, are the two common clinical presentations of Post-operative pain [29]. Controlling pre-operative pain has been shown to decrease the likelihood of developing chronic pain [30]. It is vital that the surgeon, anesthesiologist, and the pain physicians collaborate in the peri-operative period to decrease the acute post-operative pain and thus decrease the chance of developing chronic pain that would later prohibit rehabilitation. Epidural analgesia peri-operatively is controversial, as literature exists in the form of randomized clinical trials both supporting and disproving improvement in phantom limb pain after amputation [31-32].
Amputation surgery has not been evaluated as extensively as arthroplasty in regards to appropriate thromboprophylaxis post-operatively. A recent Cochrane review from 2013 implies that no good data exists on prophylaxis for venous thromboembolism in patients undergoing lower extremity amputations [33]. It is vital not to forget thromboprophylaxis post-operatively in lower extremity amputees. Studies show an increased incidence of pulmonary embolism in patients who underwent an amputation following trauma compared to patients with long-bone fractures after a trauma without amputation [34]. Additionally many of the risk factors for venous thromboembolism are present in the population undertaking the amputation: increased age, sedentary lifestyle, and longstanding peripheral artery disease [33].
Outcomes and Rehabilitation
Amputation surgery is frequently performed electively, although emergency amputation operations do occur, thus allowing for pre-operative workup and evaluation by the rehabilitation team [35]. This team is composed of the rehabilitation physician, the physiotherapist, the healthcare psychologist, a psychiatrist, and a social worker [35]. In the Netherlands consensus has been reached on the focus of pre-operative, post-operative, and the prosthesis phases of rehabilitation, they include: joint mobility preservation, muscle strength training, cardiovascular fitness, balance, mobility, home-exercise, activities of daily living management, and home situation integration [35]. Delivering a service line in such a fashion allows for optimization of amputee rehabilitation increases the probability of a return to work, which is currently quoted at between 60%-80%.
Transfemoral
Function and thus rehabilitation following transfemoral amputation is affected by residual femur length, femoral orientation, and adductor muscle attachment [41]. Recent literature indicates that shorter more abducted limbs following transfemoral amputation result in more aberrant pelvic kinematics [42]. Unattached adductors allow for unopposed abductor function, thus making the femur unstable and altering the anatomic and mechanical alignment of the limb. The abductor lurch, commonly seen following inappropriate soft tissue repairs during transfemoral amputation, prohibits energy efficient ambulation and often cannot be overcome with prosthesis [42]. The adductor magnus maintains the largest cross sectional area of adductor muscles, thus its moment arm in stabilizing the femur is greatest, making it vital be incorporated in the myodesis. As transfemoral amputees increase in age, they are less likely to ambulate independently [43]. Current belief is that of the two factors, femur length and femur orientation, that length is the dominant factor in assessing gait outcomes for patients with transfemoral amputations. Although a more proximal amputation, transfemoral amputations are sometimes preferred to the knee disarticulation because advancements in prosthetic design and technology have facilitated return to independent ambulation.
Knee disarticulation
Significantly less literature exists on knee disarticulation compared to transfemoral or transtibial amputations. This procedure is advantageous to both ambulators and non-ambulators. Known benefits to those who ambulate include end weight bearing, adductor preservation, less energy expenditure, avoidance of painful bone spurs, fewer tendencies to develop a hip flexion contracture, and a simple prosthesis [44]. To those who do not ambulate it simplifies transfers, allows for ease of mobility with a wheelchair, and eliminates the complication of knee flexion contracture post-operatively [44]. Compared to the transfemoral amputation the knee disarticulation has a longer lever arm that improves counter balance properties. In recently published article by Murakami and Murray in 2015, the authors note an improvement in living status in patients who had a knee disarticulation compared to transfemoral amputation; however ambulation with prosthesis remained inconsistent [45]. Cosmetically, a knee disarticulation can be preferred in certain situations as it maintains length of the amputated extremity and does not require application of a complex flexion bearing prosthesis. Conversations regarding the risks and benefits of both surgical options should be detailed to the patient pre-operatively to maximize informed decision making by the patient.
Transtibial
Amputees after transtibial amputation return to an independent ambulatory status 78% of the time, with the literature reporting a range from 16% to 77% depending on the quoted article, when using a posterior myocutaneous flap [15]. Limitations to rehabilitation post-operatively include pre-operative ambulatory status, previous myocardial infarction, and elevated serum creatinine [15]. Often a limitation in the rehabilitation process after the transtibial amputation, especially for elderly patients, is a lack of access to appropriate prosthesis [25]. Fletcher et al., reported that only 36% of older lower extremity amputees received proper prosthesis post-operatively, 64% in the transtibial group [25]. Given the increased energy expenditure needed to ambulate, it is the elder patient population most in need of an appropriately fitting prosthesis to increase the likelihood of successful independent ambulation. Transtibial amputation is often selected as the level of amputation because of the functional advancements in prosthetic technology but also because a more distal level may not heal secondary to poor vasculature.
Syme and boyd
The Syme amputation preserves length and thus functions, making it a good option for patients with forefoot and midfoot pathology. The more proximal amputation option, the transtibial, although quite commonly performed is substantially more morbid and requires more from the patient to return to an ambulatory status. In certain patient populations, such as pediatrics, the Syme amputation has substantial benefit as it allows the tibia to grow as the patient ages. Syme amputees rarely require rehabilitation admissions post-operatively and those patients appear to live longer compared to the more proximal transtibial amputees [46]. A classic study by Pinzur revealed that one third of patients who underwent Syme amputation died on average 5 years post-operatively while 33% of patients after transtibial amputations died within 2 years from surgery [46]. The authors note the obvious possible flaw of those with a more distal amputation had less severe disease and thus were able to ambulate with more independence. Following Syme amputation, minimal gait training is required to return to ambulation, thus they are more likely to return to walking independence than the transtibial amputee [20]. Pinzur’s study from 2003 revealed only 2/82 patients who had a Syme amputation were unable to ambulate with a prosthesis. The energy cost and metabolic demand of ambulation after a Syme amputation in not substantially increased compared to a non-amputee, however, it is significantly less when compared to the transtibial ambulator. The Boyd amputation, according to Boyd, is not only anatomically but also physiologically more advantageous to patients than other described amputations about the ankle [47]. The weight bearing stump removes the need for an artificial limb while simultaneously providing proprioceptive feedback to enhance rehabilitation and ambulation [48-49]. Although the idea of a distal amputation such as the Boyd is attractive to patients as it facilitates early weight bearing and maintains length it often results in revision surgery. The revision rates are documented as high as 50%, which would set a patient back drastically from a rehabilitation process [49]. Thus, a surgeon must have a high index of suspicion clinically for amputation success to make the decision to perform a Boyd amputation.
Mid-foot and distal
Amputations and disarticulations distal to the hind foot have a high success rate for ambulation, for example the transmetatarsal amputee ambulates without prosthesis over 75% of the time [23]. Rehabilitation to ambulation is less complex in patients having the procedure for diabetes or infection compared to those undergoing it for peripheral arterial disease. Patients with peripheral arterial disease are more likely to have delayed wound healing in a transmetatarsal amputation, and thus they have a lower likelihood of post-operative ambulation [23]. The contrary is therefore true as well that although the transmetatarsal amputation is not a disfiguring amputation and ambulation will not come at an increased cost of energy expenditure compared to controls, it is still not guaranteed [2,23]. The normal mechanics of gait by keeping the lever arm of the foot are relatively maintained by amputations of the foot distal to the hind foot allowing for lower energy expenditure ambulation without prosthesis [50]. Of note, a recent study examining the quality of life in patients after amputation recorded no difference in quality of life when comparing partial foot to transtibial amputees [51]. The authors suggest surgeons remove this variable when deciding level of amputation in the lower extremity. Ambulation and rehabilitation following forefoot amputations is relatively straightforward, as the least amount of native anatomy has been removed. Independent ambulation is nearly entirely achieved and shoe modifications can be made by a well-trained prosthetist to help re-create the foot lever arm and best restore anatomic gait biomechanics.
Conclusion
Amputation of the lower extremity is a common procedure performed by orthopedic surgeons at various levels for pathology ranging from tumor to sepsis to trauma. Treating patients with amputation requires not only ample knowledge of anatomy, but also a thorough understanding of gait biomechanics along with the current state of prosthetics and orthotics. Understanding the options for lower extremity amputation is an important part of an orthopedic surgeon’s armamentarium as it allows for the ideal surgical procedure to be performed that maximizes optimal post-operative function and rehabilitation (Figure 3). Treating the whole patient by assessing pre-operative functional status, evaluating medical co-morbidities, and reviewing the surgical pathology requiring amputation will help the surgeon and patient come to a consensus decision on the operation to be performed and rational functional goals post-operatively. Teamwork when treating amputees remains paramount for a successful return to function.