ABSTRACT
We provide a single surgeon experience of 100 cases describing the technique of directing anterior approach to the hip through a bikini incision (bikini hip replacement) without a traction table preserving the branches of the external circumflex lateral vessels, antero-medial capsule and adjacent labrum with limited dissection of the tensor fascia-lata.
At an average of 17.2 months (7.1 to 24.1), we found no evidence of groin pain or residual numbness in the lateral thigh. 1 patient had a haematoma due to increased anticoagulation that resolved spontaneously. All components were well placed with no dislocations or leg length discrepancies until the most recent follow up.
In conclusion, this soft tissue sparing technique using the bikini incision direct anterior approach is safe and led to no incidence of groin pain or lateral thigh numbness at the most recent follow-up.
KEYWORDS
Anterior approach; Bikini hip replacement; Muscle sparing
Introduction
Anterior minimally invasive hip replacement surgery has been aggressively marketed as a truly minimally invasive procedure and rapidly gaining popularity. This approach was first described in 1881 by Carl Hueter utilizing the Hueter interval [1]. Subsequently, Smith-Petersen [2] and Judet and Judet [3] also described the anterior approach to the hip through longitudinal incisions extending from below the anterior superior iliac spine.
The anterior hip arthroplasty has claimed less damage to muscles [4-6] and quicker recovery with less pain and early independent ambulation with improved gait [7-10].
Although most of the Direct Anterior Approaches (DAA) have performed through a longitudinal incision, Leunig et al., [11] reported hip arthroplasties through a bikini line incision with improved scar appearance in relatively thinner patients compared to longitudinal incisions [10].
An increased risk of bleeding has been reported with the DAAs compared to the conventional posterolateral approach [12] with parasthesia reported in up to 14.8-81% with a decrease in symptoms overtime [13,14].
The aim of this surgical approach was to determine if the author’s soft tissue sparing surgical technique reduced the incidence of groin pain and paraesthesia in the bikini total hip replacements with less incidence of haematoma formation by preserving the lateral circumflex vessels.
Materials and Methods
The first 100 consecutive bikini incision anterior approach total hip arthroplasty (bikini hip replacement) performed by a single DAA fellowship trained orthopaedic surgeon from March, 2013 to September, 2014 were included in this study. Patients with osteoarthrosis or following displaced subcapital fractured neck of femur with BMI up to 35 were included in the study. Patients with dysplastic hips, very muscular males or BMI over 35 were excluded from this report as they had a posterolateral total hip replacement. Patients were followed up at 2, 8, 26, 52 and 78 week mark after surgery.
During the follow-up periods, patients were specifically asked for any post-operative groin pain or discomfort and lateral thigh numbness. Clinically, they were assessed for haematoma formation in the operative site and anterolateral thigh for up to 8 weeks.
Surgical Technique
Operating table and patient positioning
No traction tables were used for any of the procedures. The operating table had a table break at the level of the hip joint to ensure easy access to the proximal femur for broaching (Figure 1). Patients were positioned supine with no bumps under the pelvis, ipsilateral arm placed over the chest (Figure 1). One surgical assistant stood on the opposite side of surgery.
Landmarks and incision
The Anterior Superior Iliac Spine (ASIS) was identified and marked and the skin incision placed in the lateral groin crease, a third of the length medial to the ASIS and the other 2 thirds lateral to the ASIS approximately 6-7cm long (Figure 1). Both limbs prepped and draped up to the umbilical levels.
Perioperative prophylactic antibiotics were given before and after surgery (IV Cefuroxime 2g). If required a longitudinal incision can be made in the form of a “T” incision from the bikini incision downwards and distal if difficult cases are encountered or extensive intraoperative fractures. We did not encounter any such cases. Patients should be informed this at all times during surgical consent.
Superficial and deep dissection
The skin and subcutaneous tissue was dissected and the Tensor Fascia Lata (TFL) identified. It is important to identify this as longitudinal silvery fibers that are located running laterally and inferiorly from the ASIS. There are usually several perforators at the mid portion of the body of TFL which can be cauterized.
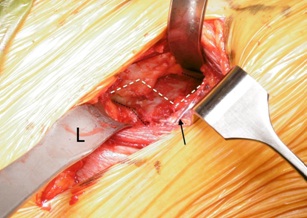
A longitudinal incision was made in the TFL approximately 3 cm below and lateral to the ASIS and the medial flap elevated utilizing the subfascial plane between the TFL and Sartorius. The TFL dissection only passed just 2-3 cm below the lateral circumflex vessels to protect the lateral branches of the lateral femoral cutaneous nerve. The ascending branches of the lateral circumflex iliac vessels were identified and preserved (Figure 2). The reflected head of rectus was gently teased off the capsule with a cob elevator and special retractors were then placed on the medial and lateral femoral neck outside the capsule (Figure 2).
Capsulotomy and femoral preparation
A partial lazy “Z” proximal lateral and distal flaps of capsule were raised without any dissection into the medial capsule past the 12’0 clock position (Figure 2). The 2 retractors repositioned intra-capsularly on either sides of the femoral neck.
A neck osteotomy was performed at the predetermined level. A further osteotomy was performed 5mm more proximal to remove a wedge of neck (napkin ring) enabling easy extraction of the head.
Only a small portion of the supero-lateral capsule was dissected and removed. The posterolateral capsule adjacent to the external rotators was carefully reflected from the neck with the aid of a large bone hook just enough to deliver the proximal femur for broaching (Figure 3) and the leg placed in figure 4. The femur was prepared first as a surgeon preference with the operated leg in a figure 4, position and the table broken to 45 degrees.
The femur was broached with a woodpecker attached to a double offset handle to the templated size making sure the modular broach was not in varus and left in situ.
Acetabular preparation
The table was leveled and retractors carefully placed (Figure 4) to avoid disrupting soft-tissue in this region and endangering the important neurovascular structures medially. Only calcified labrum laterally or superiorly removed (inner margins only) - 7’0 clock to 11’0 clock positions on a supine patient. The anterior and medial labrum was left untouched along with the anterior and medial capsule therefore protecting the iliopsoas tendon adjacent to this.
The acetabulum was reamed in increments with a double offset reamer and trialled before introducing the definitive component making sure the cup was positioned at approximately 40 degrees inclination and 15-20 degree anteversion with a double offset cup introducer. Adequate seating of the cup was assessed with a depth gauge through the screw holes. No intra operative X-rays were performed in any of the procedures. 2 screws were placed in all cases. The edge of the cup on the medial aspect was well covered with bone or thick capsule in all cases protecting the iliopsoas tendon infront. A 20 degree hooded liner was then introduced and impacted with the hood apex placed supero-laterally. Trial reductions were carried out before definitive stem was introduced and re-trialled with head sizes and leg lengths easily measured at the end of the table by feeling the medial malleoli ensuring the pelvis was square.
Components
Acetabular shell: R3™ three hole HA acetabular shell Smith & Nephew, Memphis, Tennessee. Acetabular liner: R3™ XLPE Acetabular Liners Smith & Nephew, Memphis, Tennessee. Femoral Stem (uncemented): POLARSTEM Femoral Stem, Smith & Nephew Orthopaedics AG, Baar, Switzerland. Femoral Head: oxinium femoral head, Smith & Nephew, Memphis, Tennessee.
Stability testing
Stability test was performed in every case with the operated leg crossed (Figure 4) over the contralateral leg and externally rotated to check for anterior stability and flexed and internally rotated to check for posterior stability.
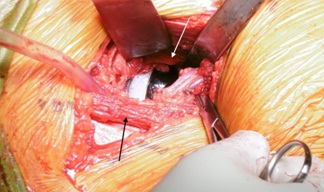
Local infiltration analgesia was carried out as per Kerr-Kohan in all cases as a part of our rapid recovery programme [15]. The lateral circumflex vessels were always protected and checked for integrity (Figure 5).
No wound drains were used in any patients.
The surgical times ranged from 48minutes to 135minutes (average 79mins).
Post-operative care
Thigh high thromboembolic stockings were used in all cases in recovery with local ice application to reduce swelling. Thromboprohpylaxis regime included oral aspirin 300mg in most cases for 6 weeks on discharge. Patients with increased risk of thromboembolism had enoxaparin 20-40mg subcutaneously daily for 4-6 weeks. All patients were mobilized either by a physiotherapist or registered nursing staff within 3-7 hours after surgery as part of our enhanced recovery programme [15].
Results
A total of 95 (n=100) patients were included in the study with an average follow-up of 17.2 months (7.1 to 24.1). Five of them had bilateral hip arthroplasties. There were 58 females, 37 males with an average BMI of 27.9 (range 23.1 to 34.8) and average age of 67 (49 to 86) - (Table 1). All except 2 patients (fracture femoral neck) were carried out for osteoarthritis. 3 hips had protrusio where the floor was bone grafted (autologous femoral head) and rim fit cup with restoration of head centre.
The majority (71%) were discharged within the first 24-48 hours post surgery enabled by our enhanced recovery programme. The rest were living home alone and waited longer for a rehabilitation bed. Most patients who went home were driving a car at an average of 11 days (3 days to 29 days).
There were no signs of superficial or deep infection or haematoma formation at early follow-up except in 1 patient who had been inadvertently taking both aspirin 300mg daily and 40mg subcutaneously. This was detected and stopped immediately at day 12 post-op. The haematoma resolved without surgical intervention. There were no dislocations or leg length discrepancies (clinical or radiological). Post operative X-rays revealed well placed acetabular and femoral components in all cases.
Until the most recent follow up no patient complained of groin pain. 2 patients had reduced sensation over the LFCN distribution which resolved with time over 26 weeks.
Intraoperatively, 1 patient had a hairline fracture only extending to the lesser trochanter but not beyond. A standard non-offset broach was being used at the time as the double offset broach was unavailable for that case. This small fracture was cerclage wired although post operatively the stem was solidly fixed with no evidence of fracture propagation. The wire was removed 8 weeks later as it was irritating the tensor fascia lata.
Another patient had a fall 3 weeks post surgery sustaining a periprosthetic fracture which was revised to a cemented long stem and fixation of fracture through posterior approach. At the most recent follow up, the components were well placed and integrated.
Discussion
The minimally invasive direct anterior approach has been popularized recently as a internervous and intermuscular approach partly driven by surgeons but also by industry and patient demands.
Emphasis should be extended to what happens under the skin incision, since this is more important than the length of the scar itself. What matters ultimately is component positioning without complications to reduce dislocations and improve longevity and function.
Leunig et al., [10] described the bikini incision for anterior approaches to the hip as it followed the anatomic cleavage lines (Langers lines) with better scars as opposed to the longitudinal scars in the standard DAA. The author of this paper was fortunate and thankful to see this incision and technique by Leunig and modify the dissection in the deeper layers with the ability to do the procedure with only 1 assistant. The author of this paper had the same experience where bikini incisions had improved scars and aesthetic appearance compared to longitudinal incisions. Our center is in the process of comparing a larger number of our longitudinal vs bikini incisions performed by a single surgeon.
The soft tissue in the path to the actual hip joint itself should be preserved as much as possible as every part handled, dissected or cut would lead to local trauma, bleeding, swelling and this would in-turn result in pain and relative limitation of function slowing recovery.
The standard DAA approaches still involve extensive dissection with ligation/cautery of the LFCA branches, extensive dissection of capsule and removal of labrum. Our technique is minimally invasive but maximally preserving with limited dissection of soft tissue and lateral circumflex vessel preservation and preserving the antero-medial capsule and adjacent labral tissue underneath. If the labrum interfered with cup seating some lateral labrum can be removed. This is because the 2 soft tissue layers can protect the anterior flexors from any irritation and subsequent pain. We did not have a single case with groin pain at the most recent follow up.
Unlike the standard DAA approaches, we preserved the branches of the lateral circumflex because even if these vessels were cauterized or ligated, with subsequent retraction and/or cessation of the temporary vasospasm (especially after cautery), these vessels may re-bleed after the wound is closed and present as haematoma or thigh swelling. This may in-turn slow recovery. In our approach described we did not need to interfere with the vessel as we managed to have good access to the proximal femur with the lateral circumflex vessels preserved.
The bikini incision anterior hip replacements were initially offered to patients with less fat and muscle over the anterior thigh. However with time the surgeon was more comfortable to extend this to patients with up to 132kg body weight.
The Lateral Femoral Cutaneous Nerve (LFCN) is at risk irrespective of the approach be it longitudinal or bikini incision. It is the deep soft tissue dissection that will determine if the nerve is at risk. Any aggressive medial retraction or extension of the TFL splitting further than 2-3centimeters beyond the level of the lateral circumflex vessels can endanger the branches of the LFCN resulting in thigh numbness. This was another reason why the lateral circumflex vessels were preserved as it acted as a landmark avoiding extensive distal TFL splitting.
The author preferred the non-traction table approach as it was much easier to check leg lengths and stability and reduced preparation time and patient change over times. This will certainly vary among surgeons and they should choose what they feel most comfortable with.
Some surgeons tend to use intra operative X-rays to check component positioning and optimal cup seating. The author of this technique had been fellowship trained in DAA and had been involved in over 250 DAA joint replacements before attempting it and was comfortable with cup placement to achieve optimal inclination and anterversion. This was confirmed on the post operative X-rays with no inclination beyond 45 degrees and anteversion beyond 20 degrees on AP and lateral films.
With respect to the scars, all patients were happy with no increased risk of infection despite being adjacent to the groin area.
Limitations
A randomized trial would have been more suitable to compare posterolateral approach with bikini and longitudinal direct anterior approach. As this paper is based on the technique itself, a subsequent trial is being planned. Our patients were all private patients who requested the anterior approach and randomization was difficult in such cases.
Initially there was bias in selecting thinner patients for the approach but with time almost all patients underwent the bikini approach.
Functional outcome scores would be very helpful in determining if this soft tissue sparing approach was superior. At the start of the study, the first group of patients did not have the rigorous post-operative scores determined although subsequent patients did and will be the basis of another study.
Conclusion
This technique of bikini hip replacement sparing the anteromedial capsule and lateral circumflex vessels and limited dissection of the TFL is a safe anterior approach to the hip to avoid anterior groin pain, haematoma formation and thigh numbness.
Figures
Figure 1: Patient Positioning.
Operating table with a table break at the level of the hip joint (just below ASIS marking). Foot bolster to prevent patient sliding off the bed during femoral preparation. Ipsilateral arm in shoulder sling. A small cylindrical bolster for the figure of “4” position was placed adjacent to the opposite knee.
Figure 2: Arrow showing preservation of the lateral circumflex branches and capsule exposed with medial and Lateral (L) retractors. The black dotted line - femoral neck outline. The white line depicts the “Z” Capsulotomy that was performed in a right hip.
Figure 3: Femoral preparation after postero-lateral capsular release and femur exposed with femoral elevator (blue handle) with leg in figure 4, position.
Figure 4: Acetabular exposure with careful placement of infero medial and infero lateral retractors (Right Hip). The infero medial retractor at 5’0 clock position-below the transverse ligament and infero lateral retractor at 8’0 clock position of acetabular margins in a right hip.
Figure 5: Lateral Circumflex vessel branches still intact after components inserted before wound closure. Antero medial capsule preserved (light arrow). The TFL still preserved at the end (dark arrow).
Tables
| Diagnosis | |
| Osteoarthritis | 98 |
| Fracture NOF* | 2 |
| Age | 67 yrs (49 to 86) |
| Sex | F=58, M=37 |
| BMI | 27.9 (23.1 to 34.8) |
| Follow-up | 7.2 months (4.1 to 18.1) |
Table 1: Patient demographics, 95 patients (n=100).
*NOF = Neck of Femur