Predicting the Short Term Outcome in Acute Organophosphorus Compound (OPC) Poisoning with Poison Severity Scale on Hospital Admission in Dhaka Medical College Hospital
*Corresponding Author(s):
Ahasan HAMNDepartment Of Medicine, Popular Medical College, Dhaka, Bangladesh
Tel:+880 1711184509,
Email:ahasanhamn@yahoo.com
Abstract
Introduction
Organophosphorus Compound (OPC) pesticide intoxication is estimated at 3 million per year worldwide with approximately 300,000 deaths mostly in Asia pacific region. Severe organophosphorus pesticides poisoning is a major clinical problem in Bangladesh.
Objectives
To assess the short term outcome OPC poisoning based on Peradeniya Organophosphorus Poisoning Scale (POP) soon after hospital admission into DMCH.
Study design
We evaluated the usefulness of the severity scale and Glasgow coma score by observational study for predicting the outcome.
Place of study
Medicine Ward of Dhaka Medical College Hospital, Dhaka.
Duration of study
July 2010 to December 2010.
Study materials
Study population - All patients with Acute OPC poisoning admitted in Medicine ward of Dhaka Medical College Hospital, Dhaka.
Study methods
Suspected cases of OPC poisoning were enrolled and observed for at least 96 hours. Detailed history and clinical manifestations of all enrolled cases were taken in a pre-design case record form. All admitted cases were treated with traditional antidote of atropine and pralidoxime and other supportive treatment also given.
Results
Fifty patients of OPC poisoning who attended in the medicine ward who fulfilled the inclusion criteria were enrolled in the study. 88% of study patients were used OPC for deliberate self harm and 12% were accidental. Common clinical presentation were Pupillary (90%), Vomiting (80%), Bradycardia (52%), Abdominal cramp (42%), Tachypnea (34%), Salivation (32%) and Altered consciousness (30%) and Fasciculation (8%) respectively. 64% patients got recovered completely, 12% recovered with minor symptoms, 16% died and 8% remained in life threatening condition. In our study, according to POP scale, 62.50% were fatal and only 11.76% patients were survived among the severe graded patients. In moderate grade, non fatal cases were 64.70% and fatal cases were 37.50%. No fatal case was detected in mild grade of POP scale.
Conclusion
In our study 16% patients died. It is one of the commonest causes of death in medicine ward. The POP scale appears useful in assessing the severity of poisoning in term of management plan. The patients with evidence of moderate and severe degree of poisoning need to be monitored closely.
INTRODUCTION
Poisoning is a common medical emergency. Self inflicted violence accounts for around half of the 1.6 million deaths that occur every year worldwide [1]. Currently self poisoning with pesticide has become a major clinical problem of the developing countries [2,3]. Bangladesh is a developing country of South Asia. Rural Population of this country is mostly dependant on agricultural cultivations. With the advancement of times, the limited availability of cultivating land results in widespread use of insecticides such as Organophosphorus Compound (OPC) [4] and these are readily available as Over the Counter (OTC) drugs in village shops and act as a common agent for suicidal purpose after trivial family problems [5]. Industrialized countries are also affected by it, where a significant proportion of suicidal deaths are caused by pesticide ingestion [6,7].
Organophosphorus Compound (OPC) intoxication is estimated at 3 million per year worldwide with approximately 300,000 deaths largely in Asia pacific region [8]. Fatality rate following deliberate ingestion of op pesticides in developing country in Asia is approximately 20% and may reach 70% during certain seasons and at rural hospitals [9]. According to annual report 2009, Department of Medicine DMCH, Bangladesh, it shown that about 18% of total poisoning patient are organophosphorus pesticides poisoning [10].
The basic mechanism of toxic effect of organophosphorus compound is the inhibition of acetyl cholinesterase at the nerve ending resulting accumulation of excess acetylcholine [4]. Most patient die from cardio respiratory failure [11].
ASSESSMENT OF SEVERITY
A number of systems have been proposed for predicting outcome in Organophosphorus Compound (OPC) poisoning. Many are reliant on laboratory tests [12-16] and are, therefore, less useful in resource poor locations. Others that use clinical parameters have only been validated using small numbers of patients.
The Peradeniya Organophosphorus Poisoning (POP) scale assesses the severity of the poisoning based on the symptoms at presentation and is simple to use. In a study by Senayeke et al., patients with a high score on the POP scale had a high rate of morbidity and mortality [17].
This study used to investigate whether it was possible to predict inpatient mortality in organophosphorus poisoning using a scoring system based on simple clinical parameters recorded only at admission. This might enable clinicians to identify patients at high risk of dying soon after presentation, allowing more intensive monitoring and treatment. A simple system based on clinical features is likely to be most useful in low income countries where the majority of organophosphorus poisoning occurs [18].
There is no universal consensus regarding diagnosis, grading of severity and management of this serious life threatening poisoning [19]. Different individualized spectrum of management is available around the world. The supportive and specific antidote are given and tuned according to individual patient. Psychological assessment and prevention strategies are lacking, ICU setup and logistic supports for proper management are also not available in all health facilities.
From this hospital based study the purpose was to see if this POP scale could predict mortality in organophosphorus pesticides poisoning using data collect prospectively on a patient's admission in Dhaka Medical College Hospital in Bangladesh.
The degree of severity is dependent on the degree of inhibition of synaptic cholinesterase, which can be indirectly assessed by serum cholinesterase activity [20]. The most serious manifestations and the usual cause of death are respiratory failure results from weakness of respiratory muscles and depression of the respiratory centre, aggravated by excessive bronchial secretion and bronchospasm.
Miosis is one of the most characteristic signs and is found in almost all patients of moderately severe and severely poisoning. Miosis may persist even after death. Transient hyperglycemia and glycosuria are found in severe OPC poisoning.
The Peradeniya Organophosphorus Poisoning (POP) scale [17], which is based on five cardinal manifestations of OPC poisoning (miosis, fasciculation, respiratory difficulty, bradycardia and impairment of consciousness), can be used to assess the severity OPC poisoning at bed side immediately after admission (Table 1).
| 1. MiosisPupil size > 2mmPupil size ≤ 2mmPupil pin point | 012 |
| 2. FasciculationNonePresent but no generalized or continuousGeneralized and continuous | 012 |
| 3. RespirationRespiratory rate ≤ 20/minRespiratory rate > 20/minRespiratory rate > 20/min with cyanosis | 012 |
| 4. BradycardiaPulse rate > 60/minPulse rate 41 - 60/minPulse rate ≤ 40/min | 012 |
| 5. Level of consciousnessConscious & rationalImpaired, responds to verbal commandImpaired, no response to verbal command | 012 |
| (If convulsion present add 1) | 1 |
| Total | 11 |
| Mild | 0-3 |
| Moderate | 4-7 |
| Severe | 8-11 |
Table 1: Peradeniya Organophosphorus Poisoning (POP) scale.
MATERIALS AND METHODS
The study was carried out in the Medicine Ward of Dhaka Medical College Hospital, Dhaka from July 2010 to December 2010. Our objectives were to predict the outcome OPC poisoning based on clinical parameters soon after hospital admission, to assess the severity of poisoning, to describe the outcome of OPC poisoning of hospital admitted patient.
All patients had a history of organophosphorus pesticide ingestion as stated by the patient or relatives, the transferring doctor or the pesticide bottle. Any cases with suspected OPC poisoning with clinical manifestations. Those patients were excluded who refused to give consent voluntarily and patients who had taken more than one poison were excluded. Purposive type non probability sampling technique was used in the study.
All data was collected by using a performed data sheet, this was done by detailed history from patient relatives, complete physical examination. Short term outcome of all the cases was recorded. Statistical analysis was done by SPSS. Results presented by choosing of variables in the form of tables, graph, percentage, chart etc. The frequency rates of various information were described & compared using statistical methods.
RESULTS
Regarding sources of OPC; 64% study patient prior purchased for household use, 26% purchased self. 88% study patient used OPC for suicidal, 12.0% happened accidentally.
Twenty three percent patients were admitted in hospital after one hour and 22% admitted after four hours of ingestion of OPC. Among them 68% taken initial treatment before hospitalization. Common clinical presentation were Pupillary (90%), Vomiting (80%), Bradycardia (52%), Abdominal Cramp (42%), Tachypnea (34%), Salivation (32%) and Altered consciousness (30%) and Fasciculation (8%) respectively. 24 (48%) patients were treated with > 400 ampoules of atropine and only 4 (8%) patient got < 100 amp. 32 (64%) patient got in between 5-10 ampoules of Pralidoxime (PAM). PAM, 10 (20%) patient > 10 amps and 8 (16%) patient got < 5 ampoules of Pralidoxime (PAM). Out of the 50 patients, 32 (64%) patients were completely recovered, 6 (12%) recovered with minor symptoms, 8 (16%) died and 4 (8%) remained in life threatening condition. Regarding death 3 (37.87%) patients died on 1st day. 2 (25%) on 4th day and 12.5% died respectively on 2nd, 3rd and 6th day respectively. 43.75% of fatal patients were admitted in hospital four hours after OPC poisoning. 73.52% of recovered patients were admitted within two hours of poisoning.
28 (82.35%) of recovered patients GCS were > 10 and among the fatal cases 12 (75%) patients GCS were < 10 at admission. 10 (62.50%) of fatal patients POP scale was in severe grade but only 4 (11.76%) of recovered patients POP scale was in severe grade.
Clinical presentation of OPC poisoning
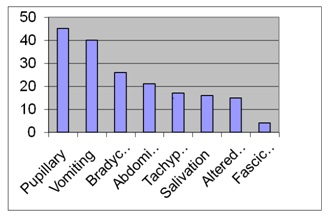 Figure 1: Bar chart showing clinical presentations of OPC poisoning.
Figure 1: Bar chart showing clinical presentations of OPC poisoning.Relationship of Glasgow Coma Scale (GCS) with fatality rate
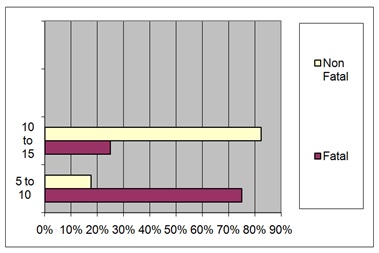 Figure 2: Relationship of GCS (Y axis) with fatality rate (X axis).
Figure 2: Relationship of GCS (Y axis) with fatality rate (X axis).Relationship of POP scale with outcome
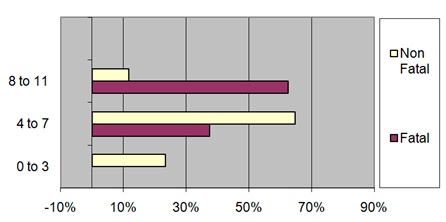 Figure 3: Relationship of POP scale (Y axis) grading with fatality rate(X axis).
Figure 3: Relationship of POP scale (Y axis) grading with fatality rate(X axis).Outcome of the OPC poisoning
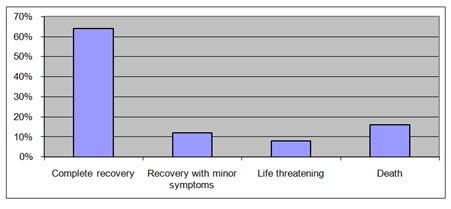 Figure 4: Bar chart shows outcome of OPC poisoning Patient.
Figure 4: Bar chart shows outcome of OPC poisoning Patient.In our study shows ages of the patients in OPC poisoning were as follows:
32% were in between 15-20 years, 28% were in between 20-25 years, 16% were in between 25-30 years and 24% were above 30 years. It reveals age distribution of 76% patients of OPC poisoning was below 30 years of age, reflecting that incidence of OPC poisoning is more common among young group. Ahmed et al. [21], reported maximum incidence of OPC poisoning (88.3%) were in between 10-30 years of age groups. Faiz MA et al. [22], reported 76% of OPC poisoning were among 11-30 years age group.
In this study out of 50 patients 36 (72%) were male and 14 (28%) were female giving male-female ratio 2.57:1. Faiz MA et al. [22], showed male-female ratio were 2.21:1, this was consistent with other studies done in Bangladesh. It may be due to male were main user OPI during cultivation. Out of 50 patients 14 (28%) were cultivators, 10 (20%) were students, 10 (20%) were service holders, other professions were housewives 8 (16%) and businessmen 6 (12%). This is consistent with the study done in national academy of medical science, Kathmandu, Nepal, by Rehiman S et al. [23]. It may be due to lack of awareness of farmers about OP intoxication, unemployment, conflicting relationship of young couple, stressful life events in developing country like Bangladesh. 64% patients received substances from prior purchased for household use, 28% patients received self purchased. The data suggested that readily available and widely used OPC was one of the common agents for suicidal use. Out of 50 patients 44 (88%) were Used OPC deliberate self harm 12% were accidental, no case was detected as homicidal. In study by Eddelston M et al., also showed similar data [18]. Out of 50 patients only 14% patients were known psychiatric patients.
In our study showing 90% patients present with Pupillary manifestation, 80% Vomiting, bradycardia 52%, Abdominal cramp 42%, Tachypnea 34%, Salivation 32%, Altered consciousness 30%, and Fasciculation 8%. In this data pupillary and GIT manifestation is an important guideline for diagnosis of OPC poisoning. In this study 44% patients required 100-300 ampoules of atropine, 28% patients required in between 400-500 ampoules, 20% in between 300-400 ampoules, and 20% in > 500 ampoules and 8% < 100 ampoules of atropine. So there is wide variation regarding the use of atropine. 64% patients required PAM in between 5-10 ampoules, 20% > 10 ampoules and 8% < 5 ampoules.
The study showing outcome of patients in OPC poisoning, 64% were completely recovered, 8% were in life threatening form and 16% died. In Bangladesh Ahmed R, et al. [21], showed the fatality rate is about 58.3% another study by Faiz MA et al. [22], found fatality 16.7%. In Nepal Rehiman S et al. [23], studies shows 14% patients were died. So still OPC poisoning is one of the commonest causes of death in medicine ward. This may be due to delay in transporting patients across long distances to hospital, paucity of health care workers compared with the large number of patients, lack of training for the management of OPC poisoning, the high toxicity of locally available poisons and lack of logistic support, efficient manpower, ICU availability and poisoning centre.
In this study showed 64.70% patients stayed hospital in between 2-5 days, 23.52% patients < 2 days and 11.76% patients stayed > 5 days. Among the fatal patients 37.5% died on 1st day of admission, 25% patients died on 4th day and 12.5% patients died on 2nd, 3rd and 5th day respectively. In this study most of the patients (37.5%) died on the 1st day of admission most likely due to respiratory failure with severe grading at presentation and lack of ICU availability. In this study 43.75% of fatal patients were admitted in hospital after 4 hours of ingestion of poison in comparison only 11.76% of recovered patients were admitted in hospital after 4 hours, 31.25% of fatal patients and 17.64% of nonfatal patients were admitted in hospital in between 2-4 hours. 25% of fatal patients and 41.17% of nonfatal patients were admitted in hospital in between 1-2 hours. No fatal patient was noted within 1 hour of poisoning, in comparison 29.4% of nonfatal patients were admitted in hospital within 1 hour of ingestion.
In our study showed 75.50% of fatal patients in comparison 17.64% of nonfatal patients GCS were in between 5-10. 25% of fatal patients and 82.35% of nonfatal patients GCS were > 10 on admission. This study shows that the GCS on admission are able to predict fatality in patients with organophosphorus poisoning, which is much easier to apply clinically. In Eddleston M [11], study GCS used as good indicator for predicting the outcome.
Regarding POP scale in our study; 10 (62.50%) of fatal patients and only 4 (11.76%) of nonfatal patients were in severe grade. In moderate grade of POP scale, fatal cases were 6 (37.50%) and nonfatal 22 (64.70%). None of fatal patients and 8 (23.52%) of nonfatal patients were in mild grade POP scale. In Senanayake N et al. [17], study showed, patients were graded as severely intoxicated had unfavorable outcome when compare to those who were graded as mildly or moderately intoxicated indicating POP scale was useful to assess the grading of severity of organophosphorus compound intoxication at first contact and help in predicting possible outcome. In our study 62.50% patients in severe grade and 37.50% patients in moderate grade were fatal indicating that patients with even moderate grade of poisoning had also fatality. So the patients with evidence of moderate and severe degrees of poisoning need close monitoring.
CONCLUSION
Organophosphorus compounds are widely used in agricultural and industrial area and as a domestic insecticide agent. It is the leading cause of morbidity and mortality due to poisoning specially agriculture based developing country like Bangladesh. In our study 16% patients died. Early diagnosis and treatment is essential to reduce the mortality and morbidity from this lethal compound. Resources for laboratory estimation of blood cholinesterase and organophosphorus level are not available in most area of developing countries. POP scale appears to be very useful to assess the severity of OPC poisoning in our study, as in severe grade showing more fatality than in mild grade. In moderate grade of POP scale also shows significant fatality. So patients with moderate and severe grade of POP scale need close monitoring to reduce the mortality.
REFERENCES
- World Health Organization (2002) The World Health Report 2002-Reducing risks, promoting Healthy life. WHO, Geneva, Switzerland.
- Jeyaratnam J (1990) Acute pesticide poisoning: a major global health Problem. World Health Stat Q 43: 139-144.
- Eddleston M (2000) Patterns and problems of deliberate self-poisoning in the developing world. QJM 93: 715-731.
- Faiz AM, Shakil A, Amin R, Aniruddha G, Hoque M (2008) Training manual of management of poisoning guideline 2008.
- Ahmad M, Rahman FN, Ashrafuzzaman M, Chowdhury DKP, Ali M (2009) Overview of Organophosphorus compound poisoning in Bangladesh and medico legal aspect related to fatal cases. JAFMC Bangladesh 5: 41-45.
- Bruyndonckx RB, Meulemans AI, Sabbe MB, Kumar AA, Delooz HH (2002) Fatal intentional poisoning cases admitted to the University Hospitals of Leuven, Belgium, from 1993 to 1996. Eur J Emerg Med 9: 238-243.
- Langley R, Sumner D (2002) Pesticide mortality in the United States 1979-1998. Vet Hum Toxicol 44: 101-105.
- Buckley NA, Roberts D, Eddleston M (2004) Overcoming apathy in research on organophosphate poisoning. BMJ 329: 1231-1233.
- Sarin SK, Kedarisetty CK, Abbas Z, Amarapurkar D, Bihari C, et al. (2014) Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific Association for the Study of the Liver (APASL) 2014. Hepatol Int 8: 453-471.
- Davies JOJ, Eddleston M, Buckley NA (2008) Predicting outcome in acute organophosphorus poisoning with a poison severity score or the glasgow coma scale. QJM 101: 371-379.
- Bardin PG, van Eeden SF, Moolman JA, Foden AP, Joubert JR (1994) Organophosphate and carbamate poisoning. Arch Intern Med 154: 1433-1441.
- Goel A, Joseph S, Dutta TK (1998) Organophosphate poisoning: predicting the need for ventilatory support. J Assoc Physicians India 46: 786-790.
- Grmec S, Mally S, Klemen P (2004) Glasgow coma scale score and QTC interval in the prognosis of organophosphate poisoning. Acad Emerg Med 11: 925-930.
- Lee P, Tai DY (2001) Clinical features of patients with acute organophosphate poisoning requiring intensive care. Intensive Care Med 27: 694-699.
- Matsumiya N, Tanaka M, Iwai M, Kondo T, Takahashi S, et al. (1996) Elevated amylase is related to the development of respiratory failure in organophosphate poisoning. Hum Exp Toxicol 15: 250-253.
- Senanayake N, de Silva HJ, Karalliedde L (1993) A scale to assess severity in organophosphorus intoxication: POP scale. Hum Exp Toxicol 12: 297-299.
- Eddleston M, Phillips MR (2004) Self poisoning with pesticides. BMJ 328: 42-44.
- Marina C, Furtado MD (2003) E-medicine Toxicities, Organophosphorus. Pg no: 1-13.
- Hayes W (1995) Toxicology of pesticides. Lippincott Williams & Wilkins, Baltimore, USA.
- Ahmed R, Shah R Amin MMM (1995) Pattern and mortality of poisoning in Dhaka Medical College Hospital. J Medical Teachers Federation 11: 10-12.
- Faiz MA, Hassan M (1998) Situation of poisoning in Bangladesh. Country report in SAARC meeting on poisoning, Colombo 1998.
- Rehiman S, Lohani SP, Bhattarai MD (2008) Correlation of serum cholinesterase level, clinical score at presentation and severity of organophosphorus poisoning. JNMA J Nepal Med Assoc 47: 47-52.
Citation: Ahasan HAMN, Faruk AA, Bala CS, Minnat B (2017) Predicting the Short Term Outcome in Acute Organophosphorus Compound (OPC) Poisoning with Poison Severity Scale on Hospital Admission in Dhaka Medical College Hospital. J Toxicol Cur Res 1: 002.
Copyright: © 2017 Ahasan HAMN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.