A Study on Knowledge Attitude and Practices of Adult Vaccination in Western India
*Corresponding Author(s):
Mohakuda SSAsst Professor, Department Of Internal Medicine, General Medicine, AFMC, Wanaworie Road, Pune, Maharashtra - 411040, India
Email:souryasourabh@gmail.com
Abstract
Background
Adult vaccination is an important issue in India where there is a high incidence of adult infective diseases which are preventable by vaccination. With the increasing number of elderly people; adult vaccination will become even more relevant. However, its importance is neither known by our clientele nor is it a focus area of our healthcare providers.
Primary objectives
To study the awareness of population about adult vaccination and the extent of counselling done by doctors for the same.
Secondary objective
To study specifically the awareness and vaccination status for tetanus, influenza and pneumococcal infections.
Materials and Methods
This descriptive study was conducted at various outpatient departments (OPDs) of a tertiary care hospital in Pune between Apr 2017 and Apr 2018 in which 230 patients were asked to fill a questionnaire to assess their awareness about adult vaccination and the counselling done by the doctors for the same.
Results
Only thirty eight percent of population who warranted vaccination were counselled for the same. Thirty three percent of total general study population were counselled for vaccination. Amongst the common adult vaccine preventable disease (tetanus, pneumococcal pneumonia and influenza), individuals were counselled least for pneumococcal pneumonia and influenza (12.8%) and were vaccinated least for pneumococcal pneumonia (5.12%).
Conclusion
This single-centre study reveals that awareness about adult vaccination is low. This may be due to the lack of counselling on the merits of adult vaccination by health-care professionals to the lay public. Increased counselling and awareness can help reduce the morbidity and mortality associated with vaccine preventable diseases in adults.
Keywords
Adult vaccination; Influenza; Pneumococcal pneumonia; Tetanus
INTRODUCTION
Infections continue to be a cause of concern for health care providers especially in the context of growing anti–microbial resistance. The only silver lining is the availability of vaccines for common infections. Wide spread data collection on infections and their prevention strategies have revealed that vaccines are the only cost effective method to combat infections. Vaccination in children has been in practice for a long time. Adult vaccination can act as a booster for vaccines administered in childhood and can also prevent life threatening infections in immune compromised patients and ageing population. According to a study in Netherland, Pneumococcal vaccine 13 (PCV 13) gives protection to 45 in 100 healthy individuals from pneumonia. Similarly the 23-valent pneumococcal vaccine gives protection to 50-85 in 100 healthy individual [1].The introduction of travellers’ vaccine has led to decreased incidence in infections in large public congregations like the Kumbhmela and Haj Similarly vaccines for pregnant women and health care workers have led to a significant decline in infection-related morbidity in these population subsets. However the uptake of adult vaccines in general population is low. In a 2016 study, PJ Lu and colleagues showed that although there was a high level of awareness about adult vaccines amongst people in US, the self-reported vaccination coverage was suboptimal [2]. A lot more needs to be done to increase the coverage of adult immunisation.
Vaccines are the cornerstone for improving the overall health of a community. There have been numerous studies which have conclusively shown the benefits of adult vaccination. Lower incidence of liver cancer and cervical cancer in Hepatitis B and HPV vaccinated individuals respectively, the lower rate of influenza-related complications in vaccinated people and the lower incidence of pneumonia in individuals with prior vaccination against pneumococcal pneumonia are just a few examples [3,4]. Apart from the direct advantages of vaccines, adult vaccines also contribute to decrease transmission of infections. A case in point is tetanus immunisation for pregnant woman that prevents lethal complications in children. From a social point of view, adult vaccination prevents people from being unwell at times when they cannot afford to be and also prevents them from cutting down on their active life years [5].
The recommendations and current status of adult immunisation has been evolving since the introduction of these vaccines. Inactivated Influenza Vaccine (IIV) or Recombinant Influenza Vaccine (RIV) has been recommended annually for all individuals above 6 months of age. Special attention for influenza vaccine is to be given to the individuals who are at risk for developing complications of influenza such those with bronchial asthma and heart disease [6]. Tetanus, diphtheria, and pertussis vaccines are recommended for adults without history of receiving tetanus toxoid, reduced diphtheria toxoid, and a cellular pertussis vaccine as an adult or child. Pregnant women are recommended 2 doses of tetanus vaccination at 20 and 24 weeks in their first pregnancy and a single dose in subsequent pregnancies. Measles, mumps, or rubella vaccines are administered to people with no evidence of protection to the same. Two doses of the same have to be administered four weeks apart. Similarly varicella vaccine is indicated in individuals with no prior history of varicella infection. Two doses of varicella vaccine are given 4-8 weeks apart. The vaccination against herpes zoster is indicated in adults above 50 years of age irrespective of prior infection [7]. 2 doses are given 08 weeks to 24 weeks apart. Immunisation against human papilloma virus is indicated in males up to 21 years of age and females up to 26 years of age. The number of doses is dependent upon the age at initial vaccination and the immunity status of the individual [4]. Pneumococcal vaccine is indicated in individuals aged 65 years or more. A 13-valent vaccine is given initially and the 23-valent vaccines are given as a booster after a period of one year. In no circumstance should both 23-valent and 13-valent pneumococcal vaccines are given at the same time. Smokers and people with a set of specified comorbidities such as immune compromised state, chronic heart, liver, kidney and lung conditions, sickle cell anaemia, those with cochlear implants and those having CSF leaks are advised immunisation with the 23-valent vaccine through ages 19 to 64. These individuals should also receive the pneumococcal vaccine as per the schedule for elderly when they cross the age of 65 years [3]. The recommendations for hepatitis A vaccination are two doses at a time to individuals who prone for infection like those travelling to endemic places or handling samples in laboratories. Hepatitis B vaccine is advised for all individuals and three doses should be given at 0, 1 and 6 months. In case of individuals with higher risk of Hepatitis B infection, for example, patients likely to be started on dialysis, an extra dose at 2 months is given and the individual dosage is doubled [8]. Two doses of meningococcal vaccine are to be given two weeks apart. Revaccination every five years is recommended for high-risk patients like those with asplenia till underlying risk persists [9]. Haemophilic Influenza type b vaccine (HIB) is advised for adults with anatomical or functional asplenia or for individuals undergoing elective splenectomy. One dose of vaccination is given, preferably 14 days prior to splenectomy [9].
MATERIALS AND METHODS
Study population and setting: This study was conducted at various OPDs in a tertiary care hospital in Pune, Maharashtra, India. The study was conducted over a period of 1 year from Apr 2017-Apr 2018. In this descriptive study the study population comprised of all adults 35 years or more visiting the outpatient department and consenting to being interviewed. The subjects were asked to fill a questionnaire on vaccine awareness. History of pre-existing comorbid conditions and clinical status of the subjects was elicited and recorded. History of their vaccination status and history of having received vaccination counselling by doctors were also recorded.
Individuals with age greater than 65 years of age or/and having co morbid conditions leading to a compromised immune status were considered warranting vaccination.
Institution ethics committee approval was taken at the commencement of the study. Identity of study subjects was kept confidential and there were no therapeutic interventions.
RESULTS
The mean age of the study population was 69 years {18 years to 88 year RANGE}. 134 out of 230 study populations were over the age of 65 years. The total study population comprised 80 females and 150 males. 78 individuals had no prior comorbidities. The distribution of comorbidities in 152 individuals is as shown in the chart below. The commonest comorbidities were hypertension (45%) and diabetes (30%). Twenty percent of the population interviewed had both. Among the immune-compromised states, 6% of the subjects were suffering from HIV/AIDS, 7% had chronic kidney disease and 5% chronic liver disease (Fig 1).
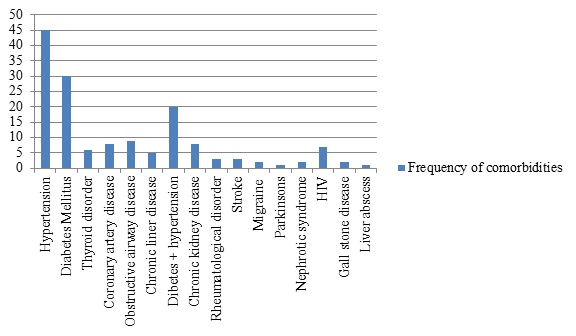
Figure 1: Distribution of comorbidity
Of the total population surveyed, 62% of the subjects thought that vaccination was necessary for people aged 65 years or more and 83% felt it was important to keep a record of immunization received. Further questioning on individual vaccines revealed that 62%, 80% and 51% of the subjects considered influenza, tetanus and pneumococcal pneumonia was vaccine preventable and 72%,77% and 66% population considered influenza, tetanus and pneumococcal vaccines to have an important impact on their health. Of all the subjects interviewed only 33% were informed by their doctors about adult vaccination and 18%, 48% and 13% of them were advised by their doctors to be vaccinated against influenza, tetanus and pneumococcal pneumonia respectively. On scrutiny, 70% of study population warranted adult vaccination based on their age and comorbidities. Of these, only 56% were advised some form of vaccination by their doctors. Specific to the disease, 33%, 39% and 59% were advised immunization against influenza, tetanus and pneumococcal pneumonia respectively. However only 22% were actually vaccinated for influenza, 77% for tetanus and 6% for pneumococcal pneumonia (Fig 2-3).
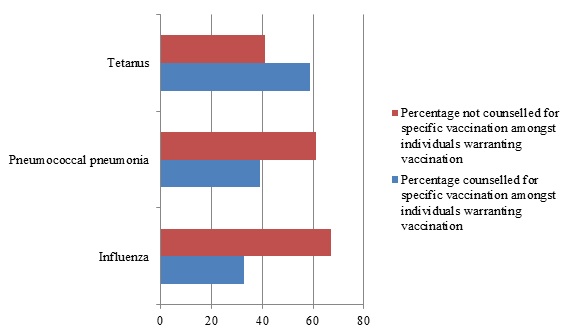
Figure 2: Counselling for adult vaccination specific for disease in individuals warranting the same
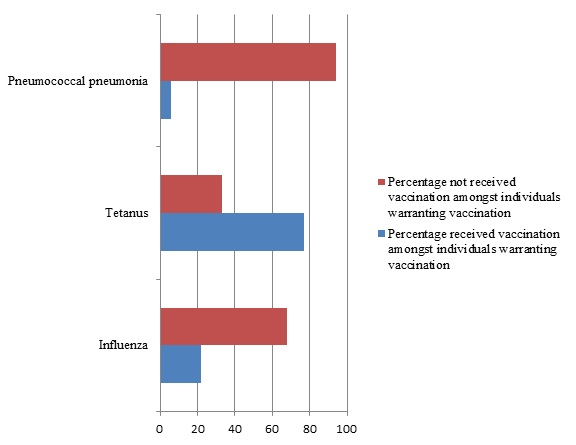
Figure 3: Vaccination status for adult vaccination specific for disease in individuals warranting the same
DISCUSSION
Infection is the leading cause of death in both the elderly people with comorbid conditions and the immune-compromised. The prevalence rate of infections in elderly patients with age greater than 65 years has been quite high in our day to day practise [10].
In our study, 62% patients thought it was necessary for an adult above 65 years of age to receive vaccination. However, only 33% patients out of the total study population had received information of the same from their doctors. 83% people thought it was important to keep a record of all their vaccinations. Peng-junlu et al in a study in 2016 found that among American adults, the awareness of vaccine preventable diseases ranged from 63.4% to 94.0%. This is comparable to the findings of our study. But our finding may not be truly representative of the general population in India, since our study population mainly comprising of serving personnel and veterans is relatively better educated and has had access to high-quality free health care service since the time of their engagement in the armed forces. We could not find any other study which looked at how often doctors counsel their patients on the importance of adult vaccines. In various studies the awareness of the need of maintaining records of vaccination data by patients has been high and was similar to our study [10,11].
When we questioned our subjects on the impact of common vaccine preventable diseases, 72%, 77% and 66% people respectively thought influenza, tetanus and pneumococcal pneumonia can have an important impact on the health of an adult. Out of the total study population, 62%, 80% and 51% patients respectively believed that Influenza, pneumococcal pneumonia and tetanus are preventable. However the rates of vaccination for these conditions were low. Only 16% and 8% of the study population were vaccinated against Influenza and pneumococcal pneumonia while 67% were vaccinated for tetanus. These findings were similar to those study published by Williams et al in 2014 in USA where vaccination for tetanus was significantly higher when compared to other infections [12].
In another study from Pune conducted by Neisha Sundaram et al during the influenza pandemic in 2009-10, only 25% of the population was aware of the availability of vaccination against influenza, though most of them (i.e. 94.7%) believed that vaccine could have a role in preventing swine flu. The same researchers found that only 8.2% received vaccination despite the widespread media coverage during swine flu epidemic [6].
Our study done around 8 years after the above quoted study has not shown a major improvement in the vaccination status of the individuals though there was a considerable increase in awareness amongst individuals. This low rate of vaccination is probably not only due to the lack of awareness which was comparable to the studies in the West but is probably due to affordability and availability of vaccines. Secondly the possibility of the study population being unaware of the above diseases having serious outcomes could be another reason. The trend and general practise in the society might also be a contributory factor. Whether to include of adult vaccination in the national immunisation schedule on the lines of childhood vaccination, would require cost benefit analysis studies. The system of reminder and recall can also have a role in increasing vaccine uptake amongst individuals. Dynanesh Limaye et al conducted a study in the University of Bombay and showed there was a direct correlation between educational and economic status and vaccine uptake [13] . There is thus a need to educate all strata of society and also make vaccines cheaper or freely available at least to the high risk population groups.
There was no significant rise in rates of vaccination in individuals warranting vaccination (i.e. age greater than 65 years or with an immune-compromised state) when compared to other population in the study. It was similar when studied for specific conditions like pneumonia, influenza and tetanus. This is most probably due to inadequate counselling and advice given by health care workers for the same. A study on awareness of adult vaccination protocols in medical practitioners can help in pin pointing the exact cause of low vaccination status in individuals warranting the same.
CONCLUSION
This single-centric study reveals a low level of awareness among general population about adult vaccination. This is partly due to the lack of adequate counselling by health-care professionals about the merits of adult vaccination.
Outreach programmes through print and audio-visual media and involving nursing and paramedical staff in adult vaccination awareness counselling can help raise awareness of this aspect of public health.
An effective adult vaccination programme will not only decrease infectious morbidity and mortality among adults but will also decrease economic burden on their families. More so, the cost of the adult vaccination programme will be very miniscule when compared to the savings made by the healthcare systems, general public and the state. As human life expectancy increases, adult vaccination will become a key public health intervention in maintaining a healthy adult population. And to achieve that, there has to be a significant increase in awareness both among the lay public and health-care worker. In order for this to happen, adult vaccination should be given the same importance as childhood vaccination in our public health programme.
REFERENCES
- Pneumococcal Vaccination | What You Should Know | CDC [Internet]. 2019
- Lu PJ, O'Halloran A, Kennedy ED, Williams WW, Kim D et al. (2017) Awareness among adults of vaccine-preventable diseases and recommended vaccinations, United States, 2015. Vaccine 35: 3104-3115.
- Tomczyk S, Bennett NM, Stoecker C, Gierke R, Moore MR, et al. (2014) Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine among adults aged ≥65 years: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep 63: 822-825.
- Markowitz LE ,Dunne EF, SaraiyaM,Lawson HW, Chesson H, et al.(2007) Quadrivalent human papillomavirus vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 56:1-24.
- Stewart AM Lindley MC, Chang KH, Cox MA (2014) Vaccination benefits and cost-sharing policy for non-institutionalized adult Medicaid enrolees in the United States. Vaccine 32: 618-623.
- Sundaram N, Purohit V, Schaetti C, Kudale A, Joseph S, et al. (2015) Community awareness, use and preference for pandemic influenza vaccines in Pune, India. Hum Vaccin Immunother 11: 2376-2388.
- Yawn BP, Saddier P, Wollan PC, St Sauver JL, Kurland MJ, et al. (2007) A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc 82:1341-1349.
- Schillie S, Murphy T V, Sawyer M, Ly K, Hughes E, et al. (2013) CDC guidance for evaluating health-care personnel for hepatitis B virus protection and for administering post exposure management. MMWR Recomm Rep Morb Mortal Wkly Rep Recomm Rep Cent Dis Control 62: 1-19.
- Centers for Disease Control and Prevention. Recommended adult immunization schedule - United States - 2015. Ann Intern Med.; 162: 214–223.
- Shieh C, Broome ME, Stump TE. (2010) Factors Associated with Health Information-Seeking in Low-Income Pregnant Women. Women Health 50: 426- 442.
- Shieh C, Mays R, McDaniel A, Yu J (2009 ) Health Literacy and Its Association With the Use of Information Sources and With Barriers to Information Seeking in Clinic-Based Pregnant Women Health Care for Women International 30 : 971- 988.
- Williams WW, Lu P-J, O’Halloran A, Kim DK, Grohskopf LA, et al. (2016) Surveillance of Vaccination Coverage Among Adult Populations -United States, 2014. MMWR Surveill Summ 65: 1-36.
- Limaye D, Limaye V, Fortwengel G (2017) A study to assess the vaccination coverage of university students in Mumbai. International Journal of Pharmaceutical Sciences and Research 8: 2667-2676.
Citation: Mohakuda SS, Sashindran VK, Murari T, Setlur R, Bansal V, Devdas N (2020)A Study on Knowledge Attitude and Practices of Adult Vaccination in Western India J Vaccines Res Vaccin, 6: 011.
Copyright: © 2020 Sashindran VK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.