
A Systematic Review on The Effects of Tobacco Use in Diabetic Patients
*Corresponding Author(s):
Angela Sarah GrahamUniversity Of Oklahoma, Norman, Health And Exercise Science Department, United States
Tel:+1 4053255539,
Email:angela.s.graham-1@ou.edu
Abstract
Introduction
Chronic disease such as diabetes is a major cause of death worldwide. Unhealthy lifestyle such as tobacco use, lack of exercise, inappropriate use of alcohol contributes to one’s susceptibility to this disease. Smoking as a diabetic patient increases the risk of developing other health challenges associated with diabetes. Hence this study identifies and summarize existing literature on tobacco use in diabetic patients.
Methods
This study adopted a systematic search of database from EBSCO, MEDLINE, Pub Med, EMBASE and Psych INFO, as well as Google Scholar for scholarly reviewed literature.
Results
Diabetic patients are high risk of transmitting Tuberculosis (TB) as a result of addiction to smoking or tobacco use. One becomes susceptible to tobacco use and develops resistant to quit when he/ she is already insulin resistant (type 2 diabetes). Some believe is a means to reward themselves after a hard day work or to manage pain and reduce boredom from the illness. Smoking cessation and other Nicotine Replacement Therapy (NRT) methods such as patches, lozenges, inhalers, chewing gum and e-cigarettes are known strategies to quit but there is the need to increase patient’s knowledge on resources available to help them.
Conclusion
This review shows different tobacco usage prevalence in diabetes. There is limited education on health implication from tobacco use among diabetic patients. Ones decision to quit smoking when diabetic seems personal, but health care providers and diabetes management clinics should provide more serious and specific advice on the possible dangers as well as making known available resources of smoking cessation.
INTRODUCTION
According to World Health Organization, diabetes is one of the health concerns which contribute to over 70% of all deaths worldwide [1]. Most of these deaths happen prematurely with about 15 million aged between 30 and 69 fallen as victims. Unhealthy lifestyle such as tobacco use, lack of exercise, inappropriate use of alcohol and unhealthy diets are some of the major risk factors associated with non-communicable diseases [1]. This alarming rate of death resulting from such risk factors, needs to be assessed by public health officials as well as understanding the triggers and impacts on the community.
Diabetes Mellitus (DM) is a disorder which happens when one has a high level of blood sugar (glucose) which causes it to be impossible for beta cells in the pancreas to either produce enough or resist insulin production in the human body. Outcome of this disease include fatigue, weight loss, vulnerability of the kidney and other health effects [2]. The economic effects of diabetes could be in the form of higher medical costs, burden on family members, premature death, productivity lost which reduce quality of life. Estimated nationwide medical expenditures for diabetes in 2017 is 2.3 times higher than persons without diabetes. With economic cost of diabetes escalated from $245 billion to $327 billion in 2017 [3].
Reasons such as blood sugar response and insulin resistance make tobacco products pleasing to persons with diabetes [4]. There is the agreement of the usage of tobacco in diabetes to control appetite and cope with stress [5]. There is also behavioral needs towards smoking in diabetic patients [5,6]. One risks the chance of good health when addicted to tobacco usage and this can increase the risk of negative health outcomes if diagnosed with Type II Diabetes (T2D) [7,8]. The rewarding and pleasure effects of nicotine in persons with diabetes may encourage smoking initiation and its continuous usage [4].
Tobacco use is associated with persons with diabetes and their risk of developing other associated health challenges increases with increased smoking lifestyle. This idea has been supported by several reviews that have linked reduced response to glucose tolerance and insulin resistance [9-11].
The objective is to review and presents study outcomes of the incidence of active tobacco use among patients with diabetes. Three research questions are used to guide this structured review:
- Does being diabetic associated with tobacco use;
- Does depression from diabetes associated with smoking behavior;
- What interventions exist for diabetes and tobacco self -management programs.
METHODOLOGY
This study used a systematic search of literature from peer reviewed articles from 2009 to 2019.Search was conducted from database such as EBSCO, MEDLINE, Pub Med, EMBASE and Psych INFO database and Google Scholar. This study followed the Preferred Reporting of Systematic Reviews and Meta-Analysis (PRISMA) guidelines [12]. Key search terms used in this review includes the following: diabetes, smoking, adults, influence and tobacco use. For a mature topic such as tobacco use in diabetic patients, a systematic review methodology is particularly useful because of an already existing body of literature as well as diverse approaches. Based on the evidence currently available, it gives a conclusive answer on a study question (such as information about intervention, self-management for diabetes, physical therapy, prevention, causes of disease and other related diseases). Systematic reviews also enable researchers to find and select important related studies, reduce personal bias and more likely to produce reliable and accurate conclusions of a study. All eligible studies used in this study were published in English in a peer- reviewed journal from January 2009 to January 2019.
STUDY SELECTION
Inclusion and exclusion of study criteria
An independent review of titles and abstract from the above-mentioned database was used as a search strategy guideline for this review. Any study that did not meet one or more criterion was excluded, assigned a reason for exclusion (e.g., Geography, study focus, or outcome) this is seen in figure 1 below. Study search was limited to United State of America, Africa and Asia due to the review focus as well as to limit the scope of study. Studies whose focus doesn’t influence or add to the study objective was excluded. For instance, most diabetes studies were excluded because they didn’t assess the association of tobacco use in diabetes. A measure of inter-reliability test was done using Cohen’s- kappa in SPSS software where two coders independently evaluated 31 articles. Final evaluation of articles from the two coders came out with 20 articles which should be included in the final analysis of review with =0.929 measure of agreement. Final selection of studies is based on full-text peer review studies. The figure below provides an overview of the number of studies searched and final inclusion of studies.
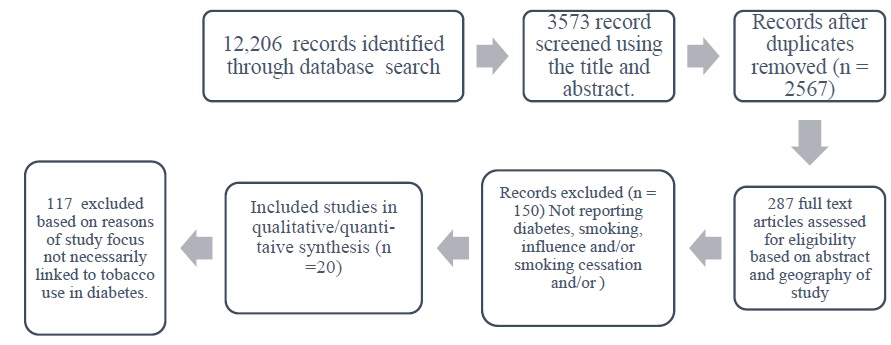 Figure 1: Flow chat of reviewed literature search.
Figure 1: Flow chat of reviewed literature search.
RESULTS
Effect of tobacco use in diabetic patients
Tobacco use is associated with many health outcomes such as T2D. In a cross- sectional study design to assess the development of diabetes in the smoking population of their study found that being an active smoker of tobacco can impact ones insulin sensitivity [13]. This affect the body’s ability to transform the usage of insulin and could lead to the development of diabetes [13-15]. Diabetic patients are high risk of transmitting Tuberculosis (TB) as a results of addiction to tobacco use [16]. Unhealthy eating lifestyle, tobacco usage and improper use of alcohol increase the risk of this disease [15]. This is because, cigarette contains some nicotine that causes inflammation in the body which risks one chance of developing TB [2]. The habit of smoking could lead to many health complications such as developing cardiovascular diseases among diabetic population [17]. Smoking and unhealthy lifestyle which leads to obesity are also seen as factors that cause T2D. From the study of Akter, Goto and Mizoue [18], every 10 cigarette sticks smoked a day leads to 16% increment of risk of T2D among those who smoke. Therefore, heavy usage of tobacco affects ones metabolism to control diabetes [19].
Diabetic is associated with tobacco use
Genetic, familial factors other than environmental factors contributes to smoking persistence or continuation than smoking initiation [20]. Overweight humans are most likely to develop insulin resistant due to their eating habits. Nicotine in cigarette provides an elevated reward that make diabetic patients initiate and continue to use tobacco products [21]. One becomes exposed to tobacco use and develops resistant to quit smoking when he/ she is insulin resistant (type 2 diabetes). This is as a result of the rewarding effect of nicotine found in tobacco products [4,21,22].
Depression from diabetes influence smoking behavior
Most genetic factors as well as relationship associations and persistence influence affect one’s desire to initiate and continue smoking behavior [20]. People with migrant background or experiencing health challenges such as diabetes intend to depend on tobacco usage to suppress their frustration as well as use it as a coping mechanism for stress. Some believe is a means to reward themselves after a hard day’s work or to manage pain and reduce boredom from the illness [23].
Interventions that exist for diabetes and tobacco self-management programs
Diabetes management programs that will include education on appropriate insulin regulation can help to educate patients to minimize tobacco use [21]. The benefit of a cessation program may not be immediate during the first 5 years of not smoking, but such risk is minimized when one engages longer in a smoking cessation program [18]. There is a perception among diabetic patients that smoking does not affects their health condition [24]. This implies limited education exists regarding the effects of tobacco use and diabetes. Healthcare providers engaged in diabetes management have a key role to play in smoking cessation programs [25]. There is gender difference and barriers to quit, hence smoking cessation for diabetes management should be structured in an appropriate format to meet these differences. There is limited awareness of resources such as Nicotine Replacement Therapy (NRT) or drug bupropion (Zyban) available at most clinics in diabetic patients [8,25]. Most of their knowledge about smoking cessation is the quit lines which they saw from the media rather than from healthcare providers. Most diabetes management includes the risk and measures to avoid other related health challenges such as hypertension, dyslipidemia, cardiovascular and hyperglycemia but such package should include support and encouragement to quit smoking since most of them lack the motivation to quit [8,23].
DISCUSSION
This review presents study outcomes of the incidence of active tobacco use among patients with diabetes. The desire to quit smoking in diabetes is limited by the rewards they get from nicotine in cigarette and the influence of external forces such as depression or issues of life makes patients to relapse to tobacco use [4,23]. Whiles some believe decision to quit is personal and they rather resort to the internet for more information about smoking cessation than to listen to people, there is the need for healthcare providers in diabetes management clinic to provide direct instructions and advice on the possible threats and health impact of tobacco use on diabetes to help bridge the education gab [23]. Suggestions on engagement in healthy eating lifestyle such as drinking tea, eating or snacking healthy, restriction of cigarette exposure at home and outings are some potential strategies that a diabetic smoker could engage in. Weight gain resulting from post smoking- cessations also discourages most diabetic patients [9]. There is the need to implement and enforce smoke-free legislation in various state to help reduce secondhand smoking as well as health promoters applying the principle of Extended Parallel Process Model (EPPM) to show the dangers of smoking and how such activities affect diabetic patients (example using messages and images that provides a negative fear stimulus causing people to re-think their action and to develop the efficacy of changing) [9,23].
Most people know the health risks of smoking such as respiratory and cardiovascular diseases but believe smoking not necessarily develop as a result of tobacco use but believe is primarily genetic [8,20]. Using the principles of Health Belief Model (HBM), patients who do not realize an impact of smoking on their diabetes management as a risk will not make any effort to quit. Only those who perceive a strong negative impacts such as erectile dysfunction (especially men) will be motivated to quit [5]. Risk of T2D increases during the first 5 years of engaging in smoking cessation but such risk reduces steadily when one engages longer in such program [18].
Most diabetes management includes the risk and measures to avoid other related health challenges such as hypertension, dyslipidemia, cardiovascular and hyperglycemia but such package should include support and encouragement to quit smoking as well as provision of resources to help patients self- manage efficiently. A structured interview of diabetic patients attending clinics to find their awareness of smoking cessation available to them found that smoking cessation and other NRT methods such as patches, lozenges, inhalers, chewing gum, and e-cigarettes are known strategies to quit but most patients are not informed by their healthcare services [8,23].
Health interventions for diabetes management should be tailored to meet the needs of patients not a one size fit interventions for all. For instance, there should be personalized smoking, health and lifestyle intervention that address the specific needs of the intended audience. This could be efficiently done when actual concerns and information is gotten form the patients either in a meeting or a focus group discussion. In case where interviews are used, there should be more options for open- ended questions aimed to get participants perception since closed ended questions streamlines participant responses.
This review was limited by time and scope of review publications. Less information was gained on the influence of depression in diabetes and it associated desire to use tobacco products. The focus of tobacco use was limited to smoking; hence this affected the review results of how other tobacco usage (such sniffing and sucking) influence diabetes.
Further study should examine why people are at risk of diabetes after short term engagement in smoking cessation. Also due to different gender risk, there is the need to examine especially women risk of developing diabetes as a result of using tobacco. Little knowledge is known about some of the triggers such as stress coping and depression in diabetes management hence this could be a great area of focus in diabetes management. Since other risk factors such as alcohol use affects health outcomes of diabetes, future studies should study such risk factors and their influence in diabetes.
CONCLUSION
This review demonstrates the lack of awareness and education of health implication of using tobacco products in diabetes. Even though decision to quit is personal and rather resort to internet for more information about smoking cessation, there seem to be a gab in education. There is the need for diabetes management clinics to provide advice on the possible dangers as well as making known available resources of smoking cessation. Health Interventions that screens for TB in diabetic patients and provides education on healthy lifestyle could help detect, prevent as well as decrease the transmission and delay progress of TB in diabetes.
REFERENCES
- WHO (2019) Ten threats to global health in 2019. World Health Organization, Geneva, Switzerland.
- Wagnew F, Eshetie S, Alebel A, Dessie G, Tesema C, et al. (2018) Meta-analysis of the prevalence of tuberculosis in diabetic patients and its association with cigarette smoking in African and Asian countries. BMC Res Notes 11: 298-298.
- American Diabetes Association (2018) Economic Costs of Diabetes in the U.S. in 2017.
- O’Dell LE, Nazarian A (2016) Enhanced vulnerability to tobacco use in persons with diabetes: A behavioral and neurobiological framework. Progress in Neuro-Psychopharmacology and Biological Psychiatry 65: 288-296.
- Georges A, Galbiati L, Clair C (2019) Smoking in men and women with type 2 diabetes: A qualitative gender-sensitive exploration of barriers to smoking cessation among people with type 2 diabetes. PLOS ONE 14: 0221783.
- Brathwaite R, Addo J, Smeeth L, Lock K (2015) A systematic review of tobacco smoking prevalence and description of tobacco control strategies in sub-Saharan African countries; 2007 to 2014. PLOS ONE 10: 0132401.
- Buse JB (2007) Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial: Design and methods. The American Journal of Cardiology 99: 21-33.
- Gill GV, Morgan C, MacFarlane IA (2005) Awareness and use of smoking cessation treatments among diabetic patients. Diabetic Medicine 22: 658-660.
- Pan A, Wang Y, Talaei M, Hu FB, Wu T (2015) Relation of active, passive, and quitting smoking with incident type 2 diabetes: A systematic review and meta-analysis. The lancet. Diabetes & endocrinology 3: 958-967.
- Warren GW, Alberg AJ, Kraft AS, Cummings KM (2014) The 2014 surgeon general's report: "The health consequences of smoking--50 years of progress": A paradigm shift in cancer care. Cancer 120: 1914-1916.
- Willi C, Bodenmann P, Ghali WA, Faris PD, Cornuz J (2007) Active smoking and the risk of Type 2 Diabetes a systematic review and meta-analysis. JAMA 298: 2654-2664.
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLOS Medicine 6: 1000100.
- Indumathi G (2017) A study of impact of smoking on glycemic index status among patients who are attending Government Dharmapuri Medical College Hospital, Dharmapuri. International Archives of Integrated Medicine 4: 25-31.
- Jae Woong S, Tae Yong L, Sun Ha J (2018) Effect of smoking on the association of HHEX (rs5015480) with diabetes among Korean women and heavy smoking men. BMC Medical Genetics 19: 1-6.
- Teratani T, Morimoto H, Sakata K, Oishi M, Tanaka K, et al. (2012) Dose-response relationship between tobacco or alcohol consumption and the development of diabetes mellitus in Japanese male workers. Drug and Alcohol Dependence 125: 276-282.
- Bai KJ, Lee JJ, Chien ST, Suk CW, Chiang CY (2016) The influence of smoking on pulmonary tuberculosis in diabetic and non-diabetic patients. PLOS ONE 11: 1-12.
- Kar D, Gillies C, Zaccardi F, Webb D, Seidu S, et al. (2016) Relationship of cardiometabolic parameters in non-smokers, current smokers, and quitters in diabetes: A systematic review and meta-analysis. Cardiovascular Diabetology 15: 1-15.
- Akter S, Goto A, Mizoue T (2017) Smoking and the risk of type 2 diabetes in Japan: A systematic review and meta-analysis. Journal of epidemiology 27: 553-561.
- Tarnowski M, Duda-Sobczak A, Lipski J, Zozulinska-Ziolkiewicz D, Wyganowska-Swiatkowska M (2018) Tobacco smoking decreases clinical symptoms of gingivitis in patients with type 1 diabetes-a cross-sectional study. Oral Dis 24: 1336-1342.
- Carlsson S, Kuja-Halkola R, Magnusson C, Lagerros YT, Andersson T (2019) Tobacco and type 2 diabetes: Is the association explained by genetic factors? International Journal of Epidemiology 48: 926-933.
- Richardson JR, Pipkin JA, O’Dell LE, Nazarian A (2014) Insulin resistant rats display enhanced rewarding effects of nicotine. Drug and Alcohol Dependence 140: 205-207.
- Barnason S, White-Williams C, Rossi LP, Centeno M, Crabbe DL, et al. (2017) Evidence for therapeutic patient education interventions to promote cardiovascular patient self-management: A scientific statement for healthcare professionals from the American heart association. Circ Cardiovasc Qual Outcomes 10: 000025.
- Abu Ghazaleh H, Mulnier H, Duaso M (2018) A qualitative approach exploring the experiences of smoking and quitting attempts in type 1 diabetes. Journal of Clinical Nursing 27: 3091-3103.
- Thresia CU, Thankappan KR, Nichter M (2009) Smoking cessation and diabetes control in Kerala, India: An urgent need for health education. Health Education Research 24: 839-845.
- Noubiap JJ, Nansseu JR, Endomba FT, Ngouo A, Nkeck JR, et al. (2019) Active smoking among people with diabetes mellitus or hypertension in Africa: A systematic review and meta-analysis. Sci Rep 9: 588.
Citation: Graham AS (2020) A Systematic Review on The Effects of Tobacco Use in Diabetic Patients. J Addict Addictv Disord 7: 46.
Copyright: © 2020 Angela Sarah Graham, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

