
Assessment of Long Term Effects of COVID-19 in the Southern Part of Bangladesh – A Retrospective Observational Study
*Corresponding Author(s):
HN SarkerProfessor Of Medicine, MBBS, FCPS(Medicine), MRCP(UK), MRCP(Neuro), FRCP(Edin), FRCP(Glassgo), Sher-E-Bangla Medical College, Barishal, Bangladesh
Email:hnsarker@gmail.com
Abstract
Background
Post-COVID-19 syndrome is characterized by a number of new, recurring, or persistent symptoms that individuals suffer for more than four weeks after contracting COVID-19. In some individuals, the post-COVID-19 condition might linger for months or years or result in impairment.
Objective
To assess long-term effects of COVID-19 in patients who were affected with COVID -19 (RT-PCR +ve) from 1st July to 30th December, 2020 recorded in PCR Lab of Sher-E-Bangla Medical College Hospital, Barishal i.e. six months or more before the initiation of study and recovered fully.
Method and materials
This was a retrospective observational study done between July 1 and December 30, 2020 at the PCR Lab of Sher-e-Bangla Medical College Hospital in Barishal.
Results
Toal 519 patients have been selected for this study. The average age of the patient was 39 years. Among them, 28% were female and 72% were male. Among all of these patients, 16.18% (84) had comorbidity. Only 60 patients (11.57%) had different symptoms after six months of COVID-19 infection. Those patients who had both diabetes and hypertension, had more these symptoms (p<0.05) after six months of the COVID-19 infection.
Conclusion
Some patients experienced different symptoms even after they had fully recovered from COVID-19. People over 65 and those with numerous chronic health issues (such as diabetes, COPD, heart disease, kidney disease, etc.) are more likely to develop long-term conditions.
Keywords
COVID-19; Comorbidity; Long-term effects.
Introduction
On December 31, 2019, Hubei province, Wuhan, China, reported the discovery of an outbreak of the novel coronavirus nCoV-19 (SARS-CoV-2), which is the cause of the coronavirus disease-19 (COVID-19). Up till May 7th, 2021, there were 3,278,510 fatalities and about 157,343,044 confirmed cases worldwide [1]. On March 11, 2020, the World Health Organization (WHO) proclaimed COVID-19 a pandemic.
The second wave of the Coronavirus Disease 2019 (COVID-19) pandemic, which was the greatest problematic threat to public health, affected the entire planet. It posed a serious problem for the fields of science, medicine, and public health [2].
The World Health Organization estimated that 80% of infections were minor or asymptomatic, 15% had moderate to severe symptoms (requiring oxygen), and 5% had critical infections that needed ICU care. In Bangladesh, COVID-19 cases were confirmed 2,031,797 cases between 3 January 2020 and 14 October 2022, and 29,393 deaths were reported to the WHO [3].
Numerous clinical investigations have shown that a significant fraction of COVID-19 hospital patients still experience one or more health issues months after leaving the hospital [4,5]. The name "Post COVID-19 condition" has just been recommended by a working group under the WHO as a preliminary clinical case definition. This criterion is predicated on the presence of a structured consensus process three months from the onset of symptoms or the date of the SARSCoV2 infection, which lasts for at least two months [6,7]. Numerous studies have shown that between 50 and 87% of hospitalized patients around the world experienced at least one post-COVID-19 symptom for a few weeks after convalescence or hospital discharge, and that 20% of COVID-19 patients continued to experience symptoms for longer than three months despite a lessened severity [8].
Following COVID-19, such enduring and incapacitating symptoms suggest that the outbreak's negative effects did not end with recovery from the acute phase of the illness and that the pandemic is likely to continue to have an effect on people, families, and social groupings [9]. Less than 20% of COVID-19 patients require hospital admission, but more than 80% of them require therapy ranging from oxygen to ventilator support [10,11].
Objective
To assess long-term effects of COVID-19 in patients who were affected with COVID -19 (RT-PCR +ve) from 1st July to 30th December 2020 recorded in PCR Lab of Sher-E-Bangla Medical College Hospital.
Materials And Methods
- Study Design
An observational retrospective study.
- Study Population
COVID -19 (RT-PCR +ve) patients from 1st July to 30th December, 2020 recorded in PCR Lab of Sher-E-Bangla Medical College Hospital, Barishal.
- Inclusion Criteria
COVID-19 (RT-PCR +ve) patients age 2 years and above.
Those patients whose mobile numbers are recorded in the register.
Those patients who/their attendants are available on mobile phone.
- Exclusion Criteria
Persons below 2 years of age.
Those patients whose mobile numbers are not recorded in the register.
Those patients who/their attendants are not available on mobile phone.
Those who died by this time from causes unrelated to COVID-19.
- Sample Size (n)
To determine the sample size the following formula was followed

n= the desired sample size
z= Standard normal deviate usually set at 1.96
p= Proportion in the population; if not known, it is regarded as 0.5 (50.0%), here p is 0.27
q= 1-p
d= Degree of accuracy which is considered as 0.05
According to this formula the targeted sample was 302.
But attempt will be taken to take more sample population as far as possible.
According to this formula our final sample size for this study was 519.
- Sampling Technique
Simple random sampling.
- Place of Study
Sher-E-Bangla Medical College, Barishal, Bangladesh.
- Duration of the Study
The duration of the study was 6 months, from 1st July to 30th December 2021.
- Statistical Analysis
Statistical analyses carried out by using the Statistical Package for Social Sciences version 23 for Windows (SPSS Inc., Chicago, Illinois, USA). The mean and Standard deviation values calculated for continuous variables and t- test employed for continuous data. P values < 0.05 was considered as statistically significant.
Results
Table 1 shows the age distribution of the patients. Age of the patients in our study ranged from 2 to >75 years. Minimum age was 2 years and highest age was 82 years. The mean age was 39 years. Most of the patients were in 31 to 45 years age group, which was 194 (37.4%) of the studied patients
|
Age range in years |
Frequency |
Percent (%) |
Valid Percent (%) |
Cumulative Percent (%) |
|
2 to 15 years 16 to 30 years 31 to 45 years 46 to 60 years 61 to >75 years Total |
22 |
4.2 |
4.2 |
4.2 |
|
138 |
26.6 |
26.6 |
30.8 |
|
|
194 |
37.4 |
37.4 |
68.2 |
|
|
123 |
23.7 |
23.7 |
91.9 |
|
|
42 |
8.1 |
8.1 |
100.0 |
|
|
519 |
100.0 |
100.0 |
|
Table 1: Age distribution of the patients
Figure 1 shows that majority of the patients in our study was male. Among our study population, 72% were male and 28% were female.
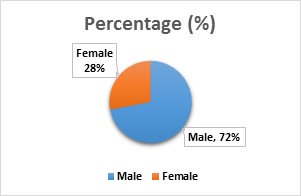 Figure 1: Age distribution of the patients.
Figure 1: Age distribution of the patients.
- Sex distribution
Among the 519 patients only 84 (16.18%) had Co-morbidities. Majority of the patients were suffering from hypertension (78.44%) and diabetes (50.22%). Significant number of patients were also suffering from heart disease (33%). Common co-morbidities of the patients are shown in Table 2.
|
Co-morbid conditions |
Frequency |
Percentage (%) |
|
|
Diabetes mellitus |
42 |
50.22% |
|
|
Hypertension |
67 |
78.44% |
|
|
Ischemic heart disease |
28 |
33.00% |
|
|
Cancer |
9 |
10.33% |
|
|
Chronic kidney disease |
9 |
10.89% |
|
|
Bronchial asthma |
20 |
23.78% |
|
|
Hypothyroidism |
8 |
9.78% |
|
|
Leukemia |
4 |
5.12% |
|
Table 2: Co-morbidities of the patients (n=84)
Only 60 (11.57%) patients had post-COVID symptoms after six months of COVID-19 infection. Most common complications among the patients after six months were weakness 30 (5.78%), shortness of breath 21 (4.04%), cough 6 (1.16%), memory loss 4 (0.77%) and swelling of legs 3 (0.58%) etc. (Table 3). Those patients who had comorbidities of both diabetes and hypertension had a significant correlation (p< 0.05) with weakness six months after the COVID-19 infection.
|
Symptoms |
Frequency (%) |
|
Weakness |
30 (5.78%) |
|
Breathless |
21 (4.04%) |
|
Cough |
6 (1.16%) |
|
Memory loss |
4 (0.77%) |
|
Swelling of legs |
3 (0.58%) |
|
Alopecia |
2 (0.39%) |
|
Chest pain |
1 (0.20%) |
|
Anorexia |
1 (0.20%) |
|
Constipation |
1 (0.20%) |
|
Excessive Sweating |
1 (0.20%) |
|
Allergy |
1 (0.20%) |
|
Others |
2 (0.39%) |
Table 3: Post-COVID symptoms after six months of COVID-19 infection
Discussion
The 2019nCoV is the seventh known coronavirus that can infect humans, and the remaining 6 are human coronavirus (HCoV)-229E, HCoV-OC43, HCoV-NL63, HCoV-HKU1, severe acute respiratory syndrome-related coronavirus (SARS-CoV), and Middle East respiratory syndrome-related coronavirus (MERS-CoV). The 2 highly pathogenic viruses, SARSCoV and MERSCoV, cause severe respiratory syndrome in humans and the other 4 human coronaviruses induce mild upper respiratory disease. Similar to SARS-CoV and MERS-CoV, the outbreak of COVID-19 has been declared by the WHO as a global public health emergency [12].
SARS-CoV-2 is one of the most virulent pathogens causing severe acute respiratory illness along with MERS and swine flu in humans. Initial case studies from China demonstrated COVID-19 to be a respiratory illness with a spectrum ranging from mild illness (81%), severe respiratory distress (14%) and critical illness in five per cent with a case fatality rate of around 2.4 per cent [13]. Considerable disparities in demographic and clinical patterns have been observed between countries across different continents.
In our retrospective study, a total of 519 patients were selected. Age of the patients in our study ranged from 2 to >75 years and the mean age was 39 years. In another study [14] from our country showed mean age was 42.59years. Data from the Institute of Epidemiology, Disease Control, and Research (IEDCR) [15] revealed that 42% of the Bangladeshi COVID-19 cases were aged between 21 and 50 years. 72% of our study population were male and 28% were female. Similar male preponderance was found in other studies, 73% of the first reported study of China [16] or 63% of a study in DMCH, Bangladesh [17]. It has been found that more males were infected by SARS-CoV [18].
Among the patients with co-morbidities, majority of the patients were suffering from hypertension (78.44%) and diabetes (50.22%). Only 11.57% patients developed comorbid symptoms after six months of COVID-19 infection. Most common symptoms after six months were weakness (51.1%) and shortness of breath (34.8%) Most common post-covid symptoms found in this study were weakness 30 (5.78%), shortness of breath 21 (4.04%), cough 6 (1.16%), memory loss 4 (0.77%) and swelling of legs 3 (0.58%) etc. Other symptoms were alopecia 2 (0.39%), chest pain 1 (0.20%), anorexia 1 (0.20%), constipation 1 (0.20%), excessive Sweating 1 (0.20%), allergy 1 (0.20%) and others. These findings coincide with findings of other several studies [19-22].
Conclusion
In most cases, people who contract COVID-19 make a full recovery in a matter of weeks. Yet, even after a full recovery, some people continue to have symptoms from their illness. Those over the age of 65 and those with many chronic health problems (such as diabetes, HTN, COPD, heart disease, renal illness, etc.) are at greater risk of developing long-term COVID-19 symptoms.
References
- https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- Wit E, van Doremalen N, Falzarano D, Munster VJ (2016) SARS and MERS: Recent insights into emerging coronaviruses. Nat Rev Microbiol 14: 523-534.
- https://covid19.who.int/region/searo/country/bd
- Chippa V, Aleem A, Anjum F (2022) Post-Acute Coronavirus (COVID-19) Syndrome. StatPearls.
- Roessler M, Tesch F, Batram M, Jacob J, Loser F, et al. (2021) Post COVID-19 in children, adolescents, and adults: Results of a matched cohort study including more than 150,000 individuals with COVID-19. Berlin, Germany. Cold Spring Harbor Laboratory 19: e1004122.
- Perego E, Callard F, Stras L, Melville-Johannesson B, Pope R, et al. (2020) Why the patient-made term “long COVID” is needed. Wellcome Open Res 5: 224.
- https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1)
- Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, et al. (2021) Post-acute COVID-19 syndrome. Nat Med 27: 601-615.
- Senjam SS, Balhara YPS, Kumar P, Nichal N, Manna S, et al. (2021) Assessment of post COVID-19 health problems and its determinants in north India: A descriptive cross-sectional study. Delhi, India: Cold Spring Harbor Laboratory.
- https://apps.who.int/iris/handle/10665/331446
- Bhuiyan AKMI, Sakib N, Pakpour AH, Griffiths MD, Mamun MA (2021) COVID- 19-related suicides in Bangladesh due to lockdown and economic factors: Case study evidence from media reports. Int J Ment Health Addict 19: 2110-2115.
- Su S, Wong G, Shi W, Liu J, Lai ACK, et al. (2016) Epidemiology, genetic recombination, and pathogenesis of coronaviruses. Trends Microbiol 24: 490-502.
- Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 323: 1239-1242.
- Hasan JM, Khan MAS, Rahman M, Islam MS, Debnath S, et al. (2020) Sociodemographic profile, clinical characteristics, anxiety, and depression of 74 patients infected with COVID-19: first report from Bangladesh. Preprint 1-17.
- https://www.iedcr.gov.bd/
- Chen N, Zhou M, Dong X, Qu J, Gong F, et al. (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study Lancet.
- Mowla SGM, Azad KAK, Kabir A, Biswas S, Rafiqul Islam M, et al. (2020) Clinical and Epidemiological Profile of 100 Confirmed COVID-19 Patients Admitted in Dhaka Medical College Hospital, Dhaka, Bangladesh. J of BCPS June.
- Channappanavar R, Fett C, Mack M, Ten Eyck PP, Meyerholz DK, et al. (2017) Sex-based differences in susceptibility to severe acute respiratory syndrome coronavirus infection. J Immunol 198:4046-4053.
- Richardson S, Hirsch JS, Narasimhan M, McGinn T, Davidson KW, et al. (2020) Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 323: 2052-2059.
- Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, et al. (2020) Characteristics and outcomes of 21 critically ill Patients with COVID-19 in Washington State. JAMA. 323: 1612-1614.
- Asadi-Pooya AA, Simani L (2020) Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci (2020) 11: 116832.
- Hossain M, Das SC, Raza MT, Ahmed IU, Eva IJ, et al. (2021) Immediate and post-COVID complications of symptomatic and asymptomatic COVID-19 patients in Bangladesh: a cross-sectional retrospective study. Asian J Med Biol Res 7: 191-201.
Citation: HN sarker (2023) Assessment of Long Term Effects of COVID-19 in the Southern Part of Bangladesh – A Retrospective Observational Study. J Pulm Med Respir Res 9: 080.
Copyright: © 2023 HN Sarker, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

