Autogenous Osteochondral Mosaicplasty for the Treatment of Osteochondritis Dissecans of the Humeral Trochlea in a Judo Athlete: A Case Report
*Corresponding Author(s):
Shinsuke MorisakiDepartment Of Orthopaedics, Graduate School Of Medical Science, Kyoto Prefectural University Of Medicine, Kawaramachi Hirokoji, Kamigyo-ku, Kyoto 602-8566, Japan
Tel:+ 81 752515551,
Fax:+81 752517093
Email:morisaki@koto.kpu-m.ac.jp
Abstract
Osteochondritis Dissecans (OCD) of the humeral trochlea is a rare condition and is comparable to OCD of the capitellum. Owing to its low rate of occurrence, treatment strategy remains unclear. We present a case of OCD of the trochlea in a judo athlete, in a first-of-its kind report for this type of sport. The patient was a 21-year-old man with limited range of motion and the pain in his right elbow. Computed tomography revealed OCD at the lateral trochlea, measuring 13×15 mm, which came loose. We removed the lesion and performed osteochondral autograft transplantation harvested from the femoral condyle in a mosaic-like fashion. The pain subsided and the patient returned to work. The osteochondral autograft can be an effective source for large osteochondral defects of the trochlea.
Keywords
Humeral trochlea; Osteochondritis dissecans; Osteochondral mosaicplasty
INTRODUCTION
Osteochondritis Dissecans (OCD) is a lesion representing theseparation of cartilage from the subchondral bone at an articular surface [1]. Compared with that of the capitellum, OCD of the humeral trochlea is a rare condition, [2-6] that occurs mostly in young athletes such as young baseball players and gymnasts, whose elbows accept repetitive load bearing. However, the occurrence of OCD in judo athletes has, to our knowledge, not been reported previously, and, therefore, owing to limited number of cases, the treatment strategy remains unclear, especially for the large OCD [5]. Herein, we report OCD of the trochlea ina judo athlete, who was successfully treated with osteochondral autograft transplantation.
CASE PRESENTATION
A 21-year-old man presented with limited Range of Motion (ROM) and persistent pain in the right elbow for a month. Upon being admitted to our clinic, it was revealed that the patient had mild right elbow pain for several years, and also that he participated in judo, a martial art, between the ages of 6 and 18 years. Although he noticed pain when he played judo, he did not admit to a clinic. Presently, the patient’s principal hobby was bodybuilding six days a week. The ROM of the right elbow was 105° in flexion and −35° in extension with 10° cubitas valgus angle, whereas the ROM of the contralateral elbow was 140° in flexion and 7° in extension with 8° of cubitas valgus angle. Visual analogue scale score of pain was 30. Radiography demonstrated the narrowing of humeroulnar joint space and spur formation at the olecranon fossa (Figure 1). Computed Tomography (CT) showed a radiolucent area at the trochlea groove with posteriorly located small separated fragments (Figure 2). Magnetic Resonance Imaging (MRI) showed a low-intensity area on the lateral side of trochlea in coronal view of T1-weighted image and hyperintensity in the subchondral bone in sagittal view of T2-weighted image (Figure 3). Forapproaching the small fragment in the trochlea groove, surgery was performed using olecranon osteotomy. The small loose fragment (Figure 4A) was separated from the subchondral bone, which measured 13×15 mm. The lesion was diagnosed as OCD corresponding to type IV, according to the International Cartilage and Repair Society [7] (Figure 4B). To fill the trochleal defect, an osteochondral bone graft was harvested from the less weight-bearing part of the femoral condyle of the patient. The Osteochondral Transfer System (Smith & Nephew, Andover, MA) was used for the harvest and transfer of the cylindrical autografts. The recipient tunnel was drilled perpendicular to the articular surface and four grafts measuring 3.5 mm and one measuring 2.7 mm were press fit (Figure 4C). While the spur of the olecranon fossa was removed, the olecranon was fixed with tension band wiring (Figure 5A). After two weeks of immobilization, the patient exercised his elbowwith an active motion. After six months, the olecranon had united and the hardware was removed (Figure 5B). At one year post-surgery, the ROM improved to 122° in flexion and −12° in extension, with less pain. The patient returned to his job and continued bodybuilding. CT revealed resurfacing of the articular defect in the trochlea (Figure 5C).
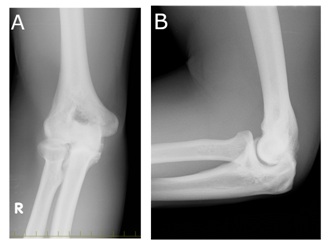 Figure 1: Pre-operative radiographs-anteroposterior view (A) and a lateral view (B). The osteophytes are seen in medial humeroulnar joint.
Figure 1: Pre-operative radiographs-anteroposterior view (A) and a lateral view (B). The osteophytes are seen in medial humeroulnar joint.
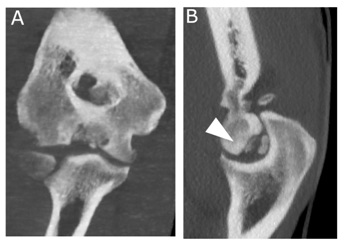 Figure 2: Computed Tomography (CT) of the elbow demonstrated radiolucent lesion in lateral trochlea groove in coronal view (A) and small fragments in posterior inferior portion in sagittal view (B). The Osteochondritis Dissecans (OCD) lesion was located between the 3 and 7 o’clock portions (arrowhead).
Figure 2: Computed Tomography (CT) of the elbow demonstrated radiolucent lesion in lateral trochlea groove in coronal view (A) and small fragments in posterior inferior portion in sagittal view (B). The Osteochondritis Dissecans (OCD) lesion was located between the 3 and 7 o’clock portions (arrowhead).
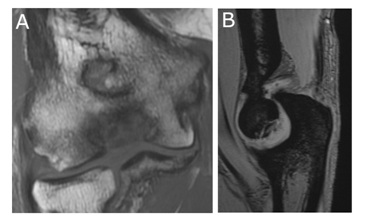 Figure 3: Magnetic Resonance Imaging (MRI) of the elbow showed a low-intensity area on the lateral side of trochlea in coronal view of T1-weighted image (A) and hyperintensity in the subchondral bone in sagittal view of T2-weighted image (B).
Figure 3: Magnetic Resonance Imaging (MRI) of the elbow showed a low-intensity area on the lateral side of trochlea in coronal view of T1-weighted image (A) and hyperintensity in the subchondral bone in sagittal view of T2-weighted image (B).
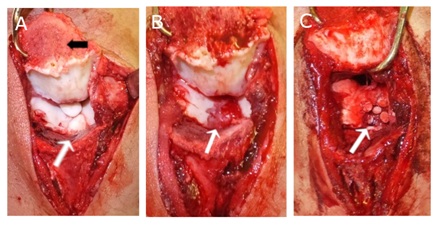 Figure 4: Surgical ?ndings. (A) The trochlea was visualized by displacing olecranon after osteotomy (black arrow). The loose fragment was separated from the subchondral bone of the trochlea (white arrow). (B) After the loose fragment was removed, there was a defect (white arrow). (C) To fill the defect, the osteochondral bone graft harvested from the femoral condyle was press fit (white arrow).
Figure 4: Surgical ?ndings. (A) The trochlea was visualized by displacing olecranon after osteotomy (black arrow). The loose fragment was separated from the subchondral bone of the trochlea (white arrow). (B) After the loose fragment was removed, there was a defect (white arrow). (C) To fill the defect, the osteochondral bone graft harvested from the femoral condyle was press fit (white arrow).
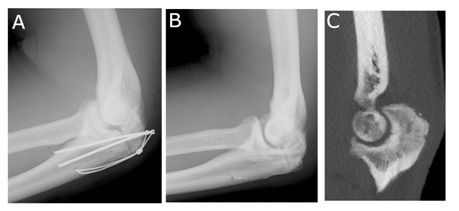 Figure 5: Post-operative radiograph-lateral view (A) showing the olecranon was fixated with tension band wiring. After six months post-surgery, the metal was removed (B). After a year post-surgery, CT showed that the osteochondral defect of trochlea was resurfaced (C).
Figure 5: Post-operative radiograph-lateral view (A) showing the olecranon was fixated with tension band wiring. After six months post-surgery, the metal was removed (B). After a year post-surgery, CT showed that the osteochondral defect of trochlea was resurfaced (C).
DISCUSSION
This case study revealed OCD, for the first time, in a judo athlete. As well, we were able to show that mosaicplasty using osteochondral autograft for the treatment of large defect of OCD of the trochlea, is an effective treatment for this lesion.
Although the exact etiology of OCD remains unknown, it is thought to result from the compounding effects of repeated valgus load to the elbow, accounting for its higher prevalence in throwers and gymnasts. In contrast, the OCD of the trochlea is much less uncommon. The OCD of the trochlea include medial and lateral types -medial lesions are small and are attributed to posteromedial abutment, whereas the lateral type, including our case, is larger and located on the posterior inferior aspect of the trochlea [5]. The latter lesion is in the hypovascular zone due to the blood supply, [8] which was observed as well in our case
Judo is one of several martial arts that originated in Japan, wherein the elbow accepts axial load in repetitive motion like gripping, throwing or pushing in order to defeat the opponent. Our patient practiced judo for 12 years and was the first to be diagnosed with OCD of the trochlea. Previously, Takahashi et al., reported that 36% of judo athletes experienced ligament injuries in the elbow [9]. Marshall et al., demonstrated that repetitive terminal extension abutment could lead to increased intraosseus pressure, decreasing blood supply, resulting in OCD of the trochlea [5]. Thus, OCD must be considered when judo athletes complain of elbow pain. In addition, our patient was bodybuilding in recent years, which contributes to mechanical stress that is manifested as osteoarthritic changes in the olecranon fossa.
We are the first to report treatment of OCD with mosaicplasty from the femoral condyle. Trochlear OCD lesions are difficult to access surgically, and initial management of rest andactivity modification should be considered [10]. When the conservative treatment is not effective, we should consider surgical treatment. In deciding the treatment for trochlea of OCD, it may be reasonable to adopt the treatment option for OCD of capitellum [1]. While Maruyama et al., reported that arthroscopic debridement/ loose body removal can be performed for small lesions (≤12 mm), Namba et al., reported that drilling gave good results [6]. However, for large lesions (>12 mm), reconstruction of the articular surface such as bone-peg fixation and osteochondral autograft transplantation or mosaicplasty, should be selected. Mosaicplasty was first applied for treating defects of the articular surface of the knee, [11,12] as well as for the capitellum [13]. The principle of mosaicplasty is the replacement of the missing articular cartilage of the defect using a mosaic of autogenous transplants. In this procedure, small cylindrical grafts are harvested and implanted in mosaic-like fashion into the focal cartilage defect of the articular surface. Solheim et al., reported that mosaicplasty resulted in a significant and better outcome than microfracture [12]. The advantage of the procedure is that, since the superficial structure of the trochlea is concave, small autografts are easily aligned to the shape of the surface. Regarding the surgical approach, because the posterior inferior portion was concealed by the surface of olecranon of the ulna, arthroscopic visualization and evaluation of the lesion was not possible. Therefore, it was necessary to use the olecranon osteotomy technique to approach the lesion, as described by Patel et al., [4] though their aim was to take biopsy without the reconstruction procedure. We are the thus, the first to report olecranon osteotomy for osteochondral graft used in the patient with OCD.
CONCLUSION
This case study revealed OCD, for the first time, in a judo athlete. As well, we were able to show that mosaicplasty using osteochondral autograft for the treatment of large defect of OCD of the trochlea, is an effective treatment for this lesion.
REFERENCES
- Maruyama M, Takahara M, Satake H (2018) Diagnosis and treatment of osteochondritis dissecans of the humeral capitellum. J Orthop Sci 23: 213-219.
- Vanthournout I, Rudelli A, Valenti P, Montagne JP (1991) Osteochondritis dissecans of the trochlea of the humerus. Pediatr Radiol 21: 600-601.
- Joji S, Murakami T, Murao T (2001) Osteochondritis dissecans developing in the trochlea humeri: a case report. J Shoulder Elbow Surg 10: 295-297.
- Patel N, Weiner SD (2002) Osteochondritis dissecans involving the trochlea: report of two patients (three elbows) and review of the literature. J Pediatr Orthop 22: 48-51.
- Marshall KW, Marshall DL, Busch MT, Williams JP (2009) Osteochondral lesions of the humeral trochlea in the young athlete. Skeletal Radio 38: 479-491.
- Namba J, Shimada K, Akita S (2009) Osteochondritis dissecans of the humeral trochlea with cubitus varus deformity. A case report. Acta Orthop Belg 75: 265-269.
- Brittberg M, Winalski CS (2003) Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 85-A Supp 2: 58-69.
- Haraldsson S (1957) The intra-osseous vasculature of the distal end of the humerus with special reference to capitulum; preliminary communication. Acta Orthop Scand 27: 81-93.
- Takahashi T, Itoh S, Kida M (2019) Availability of ultrasound screening for asymptomatic elbow injuries in judo athletes. Biomed Mater Eng 30: 49-59.
- Wang KK, Bixby SD, Bae DS (2019) Osteochondritis Dissecans of the Humeral Trochlea: Characterization of a Rare Disorder Based on 28 Cases. Am J Sports Med 47: 2167-2173.
- Hangody L, Kish G, Karpati Z, Szerb I, Udvarhelyi I (1997) Arthroscopic autogenous osteochondral mosaicplasty for the treatment of femoral condylar articular defects. A preliminary report. Knee Surg Sports Traumatol Arthrosc 5: 262-267.
- Solheim E, Hegna J, Inderhaug E (2017) Long-term clinical follow-up of microfracture versus mosaicplasty in articular cartilage defects of medial femoral condyle. Knee 24: 1402-1407.
- Funakoshi T, Momma D, Matsui Y, Kamishima T, Matsui Y, et al. (2018) Autologous osteochondral mosaicplasty for centrally and laterally located, advanced capitellar osteochondritis dissecans in teenage athletes: clinical outcomes, radiography, and magnetic resonance imaging findings. Am J Sports Med 46: 1943-1951.
Citation: Morisaki S, Tsuchida S, Oda R, Fujiwara H (2019) Autogenous Osteochondral Mosaicplasty for the Treatment of Osteochondritis Dissecans of the Humeral Trochlea in a Judo Athlete: A Case Report. Sport Med Inj Care 1: 002.
Copyright: © 2019 Shinsuke Morisaki, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.