Can Congruent Arc Latarjet Procedure Be Done On Indian Population?
*Corresponding Author(s):
Nikhil Joseph MartinOrtho One Orthopaedic Speciality Centre, 657, Trichy Road, Singanallur, Coimbatore-641005, Tamil Nadu, India
Email:docnikortho@gmail.com
Keywords
Bone graft; Congruent arc Latarjet; Coracoid process
Introduction
Bone loss is a recognised cause of failure of Arthroscopic Soft tissue procedure. Glenoid bone loss more than 20% is an indication for a bony procedure such as the one described by Latarjet and popularised by Walch. The procedure involves harvesting the coracoid process along with the conjoined tendon and transferring to the anterior-inferior glenoid neck by splitting the subscapularis tendon and then fixing the graft flush to the glenoid articular surface with two screws [1].
The classic conventional Latarjet technique involves fixation of inferior surface of the coracoid to the anterior glenoid (Figure 1) [2]. Mizuno et al [3] reported that long-term results of the Latarjet procedure was found to be excellent in the treatment of recurrent anterior glenohumeral instability with a follow-up for twenty years. Later De Beer et al. [4] described a modification in the Latarjet procedure called Congruent arc modification. This technique involves the coracoid graft being rotated by ninety degrees, resulting in its medial face being fixed to the anterior glenoid (Figure 2).
 Figure 1: Coracoid Length.
Figure 1: Coracoid Length.
 Figure 2: Coracoid Breadth.
Figure 2: Coracoid Breadth.
The idea of developing this technique was the similarity in the radius of curvature of both inferior coracoid and the anterior-inferior glenoid. This allowed placement of the coracoid flush with the bony surface of the glenoid, avoiding the need to slightly recess the coracoid medially after it has been secured in place. The arrangement of coracoid in this fashion has shown to decrease glenohumeral contact pressures and have a definite edge over the classic Latarjet technique in biomechanical studies. This would theoretically decrease the risk of arthrosis in the clinical setting [5].
The congruent arc modification does has its potential challenges. The surface area is less for bony apposition between the coracoid and anterior glenoid. The width of the graft surrounding the screw fixation is also less raising concerns for potential nonunion and fracture of the graft, respectively.
It is imperative to achieve bony union of the graft to the glenoid for a desirable for long-term success of the operation. [6] Intra- or postoperative fracture of the coracoid is always a challenging complication for the surgeon to manage. A smaller width of bone surrounding the screw may always increase the likelihood of this complication.
The aim of our study was to assess and measure the dimensions of coracoid process in dry bone scapular specimens in indian population. To establish whether congruent arc Latarjet procedure can be done in indian population. We hypothesized that the congruent arc modification of the Latarjet technique will not be possible in indian population due to thin coracoid morphology.
Materials And Methods
The study was performed on 75 human dry bone scapular specimens. The dimensions of coracoid process were done using digital vernier caliper accurate up to 0.01 mm. The parameters taken were as follows.
- Maximum length: Distance between most anterolateral to most posteromedial extension of coracoid process [7] (Figure 1).
- Maximum breadth: Distance from lateral border to medial border of coracoid process [7] (Figure 2).
- Maximum thickness: Measured in supero- inferior direction 1cm posterior to tip of coracoid process [7]. (Figure 3).
 Figure 3: Coracoid Tip Thickness.
Figure 3: Coracoid Tip Thickness.
The measurements were done by two different independent observers and the average value was calculated.
Results
The anatomic dimensions of the coracoid bony anatomy are reported in (Table 1). The average coracoid length in indian population was 39.40 + 4.93. Thickness of coracoid was 7.88 + 0.94 mm. Average thickness of the coracoid bone graft has been shown in the graph (Figure 4). Average breadth of the coracoid was 13.25 + 1.8 mm respectively. Maximum height of the coracoid was 18.49 + 3.06mm.
|
PARAMETER |
RIGHT |
LEFT |
|
LENGTH |
39.40 + 4.93 |
39.1 + 5.78 |
|
THICKNESS |
7.88 + 0.94 |
7.71 + 0.59 |
|
BREADTH |
13.25 + 1.8 |
13.32 + 1.67 |
|
HEIGHT |
18.49 + 3.06 |
18.16 + 4 |
Table 1: The average coracoid length in indian population.
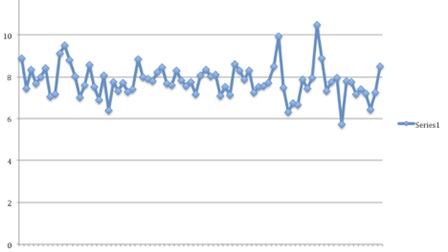 Figure 4: Average Thickness of the Graft in Indian Population.
Figure 4: Average Thickness of the Graft in Indian Population.
Discussion
The principal findings of this study are the coracoid graft dimensions in Indian population indicate that the surface area available for bony union of the coracoid to the glenoid is significantly larger when the traditional Latarjet technique is used compared to congruent arc modification and (2) the bone bridge on either side of the 3.5-mm screws used for fixation is will also be significantly less when the congruent arc technique is used compared with the traditional Latarjet technique. Therefore, our original hypothesis was affirmed.
Measurements of total coracoid thickness in the literature vary with ethinic population. The reported mean coracoid thickness is 8.2+/-1.0 mm (Salzman et al [8]), 11.5 +/- 0.9 mm Dolan et al [9], 7.88 mm (our study). The reported mean coracoid breadth is 13.6 +/- 2.1 mm (Salzman et al [8]), 15.9 +/-2.2 mm, and 18.3 +/- 1.8 mm Dolan et al [9] and (13.25+/-1.8) our study.
The dimensions of coracoid process in our population is different when compared to western population. Average thickness of coracoid process in our study was 7.88mm. Various studies with the dimensions of coracoid process reported in the literature has been summarized in (Table 2).
|
|
LENGTH (mm) |
BREADTH (mm) |
THICKNESS (mm) |
HEIGHT (mm) |
|
Our Study |
39.40 |
13.25 |
7.88 |
18.49
|
|
Dolan et al 8 |
45.6 +/- 4.2
|
18.3
|
11.5 +/- 0.9
|
|
|
Verma et al [7] |
35.54
|
14.50
|
7.95
|
20.10
|
|
Salzmann [8] |
43.1 +/- 2.2 |
13.6 +/-2.1 |
8.2+/-1.0 |
|
|
Nizlan et al [10] |
37.94 ± 4.30 |
11.63±2.12 |
9.24 ± 1.16 |
|
|
Silva et al [11] |
27 ± 3.8
|
|
9.16 +/-6.38 |
|
Table 2: Comparison of Coracoid Dimensions in Various Studies.
Few of the associated complications of this procedures are 1) non-union of the coracoid process due to the instability resulting from single screw fixation and less bone contact between surfaces, 2) Osteolysis of the coracoid graft, 3) Intra or post-operative fracture of the coracoid.
Coracoid orientation may have an impact on these complications, given the differences in the medial lateral width and inferior-superior thickness. The importance of this study lies here. Our study tries to analyse the morphology and dimensions of coracoid process in Indian population and to identify whether the of coracoid process in our Indian population gives us the surface área to insert adequate screws.
Several fixation devices using various techniques have been proposed: 2 metallic screws, [11] interference screws, [12] and plating. [13] Reports of fixation of the coracoid transfer to the glenoid with screws have shown good long-term [14] outcomes and high healing rates. [3,12].
Griesser et al. [15], in his analysis of 45 studies (1904 shoulders) demonstrated 174 cases of nonunion or fibrous union, an overall nonunion rate of 9.1 %. Walch et al., studied 68 patients with a mean follow-up of 20 years, have reported a fibrous nonunion rate of 1.5 % with no recurrence of instability. [16] Lafosse et al. [17] reviewed 62 patients, in their 5-years noted that 1 patient (1.7 %) required a reoperation as a result of graft nonunion.
For the graft to primarily get incorporated the undersurface of the should be decorticated as well as the anterior inferior glenoid rim should be made into a flat surface. As described before the graft needs to be fixed with at least two screws [11] and the screws should be placed parallel to the glenoid face to minimize the risk of nonunion of the graft. Excessive decortication of the undersurface of the coracoid while preparing the graft might weaken the graft and may predispose to an iatrogenic graft fracture. The reported rate of graft fracture is 1.5 % [15].
Care must also be taken to space the drill holes wide apart. Even though the minimum distance in between the screws is not well established, Walch et al. [18] noted in their cohort the mean distance to be 7.8 ± 1.9mm. Lafosse et al. [19] used a specific coracoid jig (Mitek, USA) to optimize the distance between the screws to 9 mm.
However, nonunion and hardware failure have been reported as few of the complications in Latarjet procedure Revision surgery in this scenario will be extremely difficult and challenging. [14] The most common choice of fixation is the screw construct and 2 bicortical screws fixation is the ideal option of fixation.
Armitage et al. [20] found that the coracoid could reconstitute a 36% defect when oriented in its classic fashion, compared with a 53% defect when rotated ninety degrees such as in the congruent arc technique. The mean width of bone on each side of a 3.5-mm screw was 7.1 +/- 1.0 mm using the traditional Latarjet technique compared with 4.1 +/- 1.0 mm using the congruent arc modification (P < .001). The two screws should be placed parallel to the glenoid face to minimize the risk of nonunion [21].
Hence to accommodate two 4 mm screw will not be possible as the average thickness of coracoid in indian population is only 7.88 mm
Limitations
This study has few limitations. All measurements were based on dry bone scapula models. Although probably negligible, measurements on cadaveric specimens would have helped in taking more accurate measurements with the help of the footprints. The curved shape of coracoid makes it difficult to measure accurately. To minimize measurement discrepancies, we have used a standard measuring technique using digital Vernier caliper.
Conclusion
The dimensions of coracoid process in our population are different when compared to western population. Average thickenss in indian population is 7.88mm and to accommodate a 4 mm screw will not be possible in this thickness. There is high chance of fracture of coracoid graft if congruent arc latarjet is attempted in all patients without measuring the thickness of the graft. Use of a single screw might lead to non-union of the graft. Hence it is recommended to perform classic latarjet procedure in our patients. If Congruent arc modification is used it would be ideal to use a smaller dimension screw. The possibility of a smaller coracoid must be kept in mind and when Congruent arc is attempted, smaller screws must be kept in standby.
Author Contribution
Dr Nikhil Joseph Martin (NJM): Study concept and design, data collection, data analysis, writing the paper.
Dr Karthik M Selvaraj (KMS): Study concept and design, data analysis, writing the paper.
Dr David V Rajan (DVR): Study concept and design, writing and reviewing the paper.
Dr. CJB Gnanaraj (CJBG): Study concept
The authors thank Ms. Sowbhaghya S Prabhu for her help in preparing the data analysis in this study.
The authors thank all the staff and management of Ortho One Orthopedic Speciality Center for completing the study.
References
- Giles JW, Degen RM, Johnson JA, Athwal GS (2014) The Bristow and Latarjet procedures: Why these techniques should not be considered synonymous. J Bone Joint SurgAm 96: 1340-1348.
- Latarjet M (1954) Treatment of recurrent dislocation of the shoulder. Lyon Chir 49: 994-997.
- Mizuno N, Denard PJ, Raiss P, Melis B, Walch G (2014) Longterm results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg 23: 1691-1699.
- De Beer JF, Roberts C (2010) Glenoid bone defectsd Open Latarjet with congruent arc modification. Orthop Clin North Am 41: 407.
- Ghodadra N, Gupta A, Romeo AA, Bach BR, Verma N, et al. (2010) Normalization of glenohumeral articular contact pressures after Latarjet or iliac crest bone-grafting. J Bone Joint Surg Am 92: 1478-1489.
- Di Giacomo G, Costantini A, de Gasperis N, Vita AD, Lin BKH, et al. (2011) Coracoid graft osteolysis after the Latarjet procedure for anteroinferior shoulder instability: A computed tomography scan study of twenty-six patients. J Shoulder Elbow Surg 20: 989-995.
- Verma U, Singroha R, Malik P, Rathee SK (2017) A study on morphometry of coracoid process of scapula in north Indian population. Int J Res Med Sci 5: 4970-4974.
- Salzmann GM, Paul J, Sandmann GH, Imhoff AB, Schottle PB (2008) The coracoidal insertion of the coracoclavicular ligaments: An anatomic study. Am J Sports Med 36: 2392-2397.
- Dolan CM, Hariri S, Hart ND, Mcadams TR (2011) An anatomic study of the coracoid process as it relates to bone transfer procedures. J Shoulder Elbow Surg 20: 497-501.
- Shin JJ, Hamamoto JT, Leroux TS, Saccomanno MF, Jain A, et al. (2017) Biomechanical Analysis of Latarjet Screw Fixation: Comparison of Screw Types and Fixation Methods. Arthroscopy 33: 1646-1653.
- Shah AA, Butler RB, Romanowski J, Goel D, Karadagli D, et al. (2012) Short-term complications of the Latarjet procedure. J Bone Joint Surg Am 94: 495-501.
- Weppe F, Magnussen RA, Lustig S, Demey G, Neyret P, et al. (2011) A biomechanical evaluation of bicortical metal screw fixation versus absorbable interference screw fixation after coracoid transfer for anterior shoulder instability. Arthroscopy 27: 1358-1363.
- Giacomo GD, Costantini A, de Gasperis N, Vita AD, Lin BKH, et al. (2013) Coracoid bone graft osteolysis after Latarjet procedure: A comparison study between two screws standard technique vs mini-plate fixation. Int J Shoulder Surg 7: 1-6.
- Gupta A, Delaney R, Petkin K, Lafosse L (2015) Complications of the Latarjet procedure. Curr Rev Musculoskelet Med 8: 59-66.
- Griesser MJ, Harris JD, McCoy BW, Hussain WM, Jones MH, et al. (2013) Complications and re-operations after Bristow- Latarjet shoulder stabilization: A systematic review. J Should Elbow Surg 22: 286-292.
- Leroux T, Wasserstein D, Veillette C, Khoshbin A, Henry P, et al. (2014) Epidemiology of primary anterior shoulder dislocation requiring closed reduction in Ontario, Canada. Am J Sports Med 42: 442-450.
- Bachy M, Lapner PL, Goutallier D, Allain J, Hernigou P, et al. (2013) Coracoid process x-ray investigation before Latarjet procedure: A radioanatomic study. J Should Elbow SurgAmerican Should Elbo Surg 22: e10-4.
- Young AA, Baba M, Neyton L, Godeneche A, Walch G (2013) Coracoid graft dimensions after harvesting for the open Latarjet procedure. J Should Elbow Surgery / Am Should Elbow Surg 22: 485-488.
- Rosso C, Bongiorno V, SamitierG, Dumont GD, Szollosy G, et al. (2014) Technical guide and tips on the all-arthroscopic Latarjet procedure. Knee Surg Sports Traumatol Arthroscopy: Official journal of the ESSKA 24: 564-572.
- Armitage MS, Elkinson I, Giles JW, Athwal GS (2011) An anatomic, computed tomographic assessment of the coracoid process with special reference to the congruent arc Latarjet procedure. Arthroscopy 27: 1485-1489.
- Dumont G, Vopat BG, Parada S, Cohn R, Makani GS, et al. (2017) Traditional Versus Congruent Arc Latarjet Technique: Effect on Surface Area for Union and Bone Width Surrounding Screws. Arthroscopy 33: 946-952.
Citation: Martin NJ, Selvaraj KM, Rajan DV, Gnanaraj CJB (2022) Can Congruent Arc Latarjet Procedure Be Done On Indian Population?. Sport Med Inj Care 3: 012.
Copyright: © 2022 Nikhil Joseph Martin, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.