Chronic Urticaria: A novel approach in Treatment
Abstract
To investigate the prevalence of pollen sensitization in patients with chronic spontaneous urticaria (CSU) and to observe the clinical efficacy of specific immunotherapy in patients when pollen sensitization was the only identifiable cause.
Methods
Patients who were diagnosed with CSU between 2005 and 2012 were included in a prospective study. Only patients who had urticaria at least 5/7 days of the week were included. Patients were evaluated by history, duration, severity and frequency of symptoms, drugs used, total and specific IgE for local pollens. Those who were pollen sensitive were observed for 2 weeks before starting specific immunotherapy (SCIT) and monthly follow up at least for one year. The end point was asymptomatic at least for 6 months compared to controls who did not receive SCIT.
Results
Thirty three patients, 23 females and 10 males were included and 15 patients controls. Seven patients had urticaria alone and 26 patients had urticaria with AR or BA or both. Four patients were lost to follow up. Seven patients (24%) became symptom-free compared to 15 controls (p<0.0001), 22/29 (76%) their urticaria became far spaced or went into remission with p<0.001, Visual analogue for 7/24 was 100% and 22/29 visual analogue was between 50% and 95%. In 4 patients there was no improvement. The overall improvement in SCIT patients for one year or more was 80% (25/29).
Conclusion
Patient with CSU, were pollen sensitization is the only identifiable cause may benefit from SCIT. This study is the first to show the benefit of IT in CSU.
Keywords
BACKGROUND
OBJECTIVE
METHODS
RESULTS
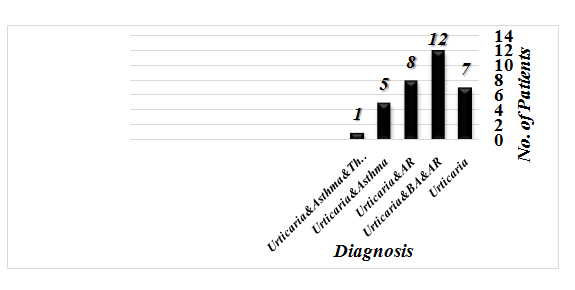 Figure 1
Figure 1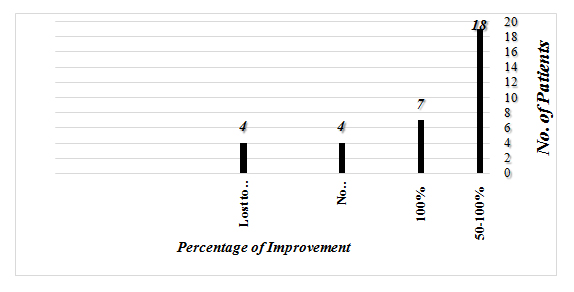 Figure 2
Figure 2Table (2) shows the characteristics of patients who were lost to follow up and (Table 3) shows the characteristics of patients who did not improve with immunotherapy. The overall improvement in patients who received SCIT for one year or more was 86% (25/29) patients. Table (4) is the characteristics of patients who had 100% improvement. Some patients started to show significant improvement as early as seven months of after the start of treatment.
|
Male |
Female |
Total of Patient |
|
10 |
23 |
33 |
|
Age Range: |
Average: |
|
|
8-56 years old |
30.68 years |
|
|
Duration of Urticaria |
Patient |
|
|
10-17 years |
8 |
|
|
< 1year |
12 |
|
|
1-3 years |
3 |
|
|
6 weeks-3 months |
6 |
|
|
Unknown |
4 |
|
|
Age |
Sex |
Total IgE |
Specific IgE |
Duration of Disease |
Duration of IT |
Other Diagnosis |
|
1 |
42 y |
F |
106 KU/L |
Weeds + Grass |
6 M |
8 Months |
Eczema for 6 months |
|
2 |
52 y |
M |
4055 KU/L |
Weeds + Grass |
10 M |
4 Months |
AR, BA, High Anti Thyroid Antibody |
|
3 |
42 y |
F |
151.5 KU/L |
Weeds |
2 M |
2 months |
AR |
|
4 |
13 y |
F |
399 KU/L |
Weeds + Grass |
3 Y |
4 months |
AR, BA |
|
|
Age |
Sex |
Total IgE |
Specific IgE |
Duration of Disease |
Duration of IT |
Other Diagnosis |
|
1 |
56y |
M |
1574 KU/L |
Weeds + Grass |
? |
14 Months |
AR, Hypothyroid |
|
2 |
40y |
F |
407 KU/L |
Weeds + Grass |
10 years |
43 Months |
BA, AR, Drug Allergy |
|
3 |
43 y |
F |
174 KU/L |
Weeds |
7 Months |
29 Months |
|
|
4 |
40 y |
M |
254 KU/L |
Weeds + Mesquite |
? |
12 Months |
AR, BA |
Table 3: Characteristics of patients who did not improve.
|
|
Age |
Sex |
Total IgE |
Specific IgE |
Duration of Disease |
Duration of IT |
Comments |
|
1 |
31 |
F |
142 |
Weeds + Mesquite |
14 years |
15 Months |
Mild AR, |
|
No Treatment |
|||||||
|
2 |
39 |
F |
50.5 |
Weeds + Grass |
2 years |
36 Months |
BA,ARAsypmtomatic No treatment |
|
3 |
35 |
M |
260 |
Weeds |
10 years |
36 Months |
AR Asypmtomatic No treatment |
|
4 |
33 |
M |
38.8 |
Weeds + Grass |
9 months |
30 Months |
Asypmtomatic |
|
5 |
33 |
F |
ND |
Weeds + Grass + Mesquite + Cat |
15 months |
60 months |
Asypmtomatic |
|
6 |
12 |
F |
1215 |
Weeds + Grass |
2 years |
19 months |
Asypmtomatic |
|
7 |
21 |
M |
141 |
Weeds + Grass + Food |
3 months |
36 months |
BA,ARAsypmtomatic |
Table 4: Characteristics of patients with 100% improvement.
DISCUSSION
None of these modes of treatments gave long lasting remission of chronic urticaria. We asked ourselves what to do with patients with chronic urticaria, where the only identified cause is sensitivity to pollens, especially when urticaria is associated with other symptoms of allergy such as allergic rhinitis, or allergic asthma or both. The most common sensitizing allergens in our patients were Mugwort, Russian Thistle, Amaranthus and Atriplex. Some patients were sensitized to weeds, grasses and Mesquite trees. Because sunshines 12 months a year in our region, plants pollinate all year around. Therefore, we decided to treat those patients with local allergens vaccine starting with the low concentration the patient can tolerate without reactions. We are aware some allergist use higher concentrations of vaccine for maintenance, our patient were unable to tolerate concentration more than 1:500 w/v without reaction. This may be due to the fact that pollen is in the air all the time, in addition to the finding that pollens are crushed by sand particles which make them more potent. All patients were informed that this is a new approach before we got their consent. In one year after starting SCIT the majority of our patient had remarkable improvement and most stopped symptomatic treatment. Xing DR, et al., [8] treated 2885 patients who had chronic urticaria and dust mite allergy, with immunotherapy with good to excellent results; with efficacy of 91.1% (226/248) with 66.1% of excellent or good results. Collins found more mugwort and birch sensitization in patients with chronic urticaria compared to allergicrhinitis but no allergy vaccine was given [9]. Similar studies by other authors showed the same [10,11]. There is one case report by Kasperska-Zajak where a patient with respiratory allergy and CU his Urticaria flared up during Immunotherapy with dust mite suggesting that Immunotherapy is beneficial in sensitized chronic urticaria [12]. Mahesha, et al., found high sensitivity among patients with urticaria to dust mite suggesting that allergy may play a role in the cause of chronic urticaria [13].Our patients had overall efficacy of immunotherapy of 86% with 14% (4/29) patients showed 100% remission of their urticaria compared to patient who stayed on symptomatic treatment. Although some cases of chronic urticaria go into remission even without treatment, our patients were symptomatic all the time and they did not benefit from other forms of treatment. Furthermore, we observed the continuity of their urticaria two weeks before SCIT. Their remission after SCIT cannot be attributed to natural course of remission and relapse. We believe our study proves that chronic urticaria is amenable to treatment with allergy vaccine when pollens are the main or the only underlying cause.This novel approach has no previous similar study in the English literature. Therefore, more studies are needed to confirm our findings. Although some authors mentioned that chronic urticaria is not allergic [14].
REFERENCES
- Tedeschi A, Airaghi L, Lorini M, Asero R (2003) Chronic urticaria: a role for newer immunomodulatory drugs? AM J Clin Dermatol 4: 297-305.
- Kaplan AP, Joseph K, Maykut RJ, Geba GP, Zeldin RK (2008) Treatment of chronic autoimmune urticaria with omalizumab. J Allergy Clin Immunol 122: 569-573.
- Cooke A, Bulkhi A, Casale TB (2015) Role of biologics in intractable urticaria. Biologics 9: 25-33.
- Kocaturk E (2017) Role of Biologics and Future Perspective in Treatment of Urticaria. Current Treatment Options in Allergy 4: 428-437.
- Kocatürk E, Zuberbier T (2018) New biologics in the treatment of urticaria. Curr Opin Allergy Clin Immunol 18: 425-431.
- Xiu MG, Wang DF (2011) Observation on therapeutic effect of acupoint injection desensitization with autoblood on chronic urticaria. Zhongguo Zhen Jiu 31: 610-612.
- Vena GA, Maurer M, Cassano N, Zuberbier T (2017) Alternative treatments for chronic spontaneous urticaria beyond the guideline algorithm. Curr Opin Allergy Clin Immunol 17: 278-285.
- Xing DR, Wen TH, Yu YL, Wei ZP, et al. (2008) Urticaria in relation to mite sensitivity and immunotherapy with Injection dermatophagoidei farinae. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi 26: 422-427.
- Collins JS (2009) Increased Pollen Sensitization In Patients With Chronic Urticaria. J Allergy Clin Immunol 123: 106.
- de Vos G (2012) More Mugwort sensitization in CU with Allergic Rhinitis. Dermatology 225: 141-146.
- Hesselmar B, Eriksson B, Aberg N (2007) Urticaria is associated with birch-pollen sensitization. Pediatr Allergy Immunol 18: 692-695.
- Kasperska-Zajac A (2011) Exacerbation of chronic urticaria in the course of house dust mite immunotherapy. Hum Vaccin 7:417-418.
- Mahesh PA, Kushalappa PA, Holla AD, Vedanthan PK (2005) House dust mite sensitivity is a factor in chronic urticaria. Indian J Dermatol Venereol Leprol 71: 99-101.
- KV Godes (2009) CHRONIC urticaria and treatment options. Indian J Dermatol 54: 310-312.
Citation: Harfi HA (2019) Chronic Urticaria: A novel approach in Treatment. J Allergy Disord Ther 5: 012.
Copyright: © 2019 Harb A Harfi, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.