Community Acquired Pneumonia in the Kingdom of Bahrain
*Corresponding Author(s):
Jameela Al SalmanInfectious Disease Consultant, Salmaniya Medical Complex, Manama, Bahrain
Tel:+973 17288888,
Email:jalsalman@hotmail.com
Abstract
Community acquired pneumonia is a major health problem, it has always been. It is one of the major causes for mortality and morbidity among all age groups. A retrospective study done in the Kingdom of Bahrain about the incidence, type of pathogens, treatment and outcome of patients admitted between the periods of 1st of October 2013 till the 31st of March 2014 with the admission diagnosis of pneumonia. A total 159 patients were enrolled without any exclusion criteria. The patients were 97 males (61.0%) and 62 of them females (38.99%). The diagnosis on admission of community acquired pneumonia for 124 patients out of the 159 (77.98%). Blood cultures were sterile in 139 (86.42%) of them and positive in 12. Deep tracheal aspirates have grown an organism(s) in 35 of them (25.55%) and they were sterile in 101 cultures (74.45%). The main organism grown was gram negative Multi-drug Resistant (MDR) organisms with 13 out of the 35 positive samples. Multiple medications were used for the same patient whether at the same time or on successive periods during the same illness and hospital stay. The majority of patients were on Ceftriaxone (68.55%). The average stay for the patients was 15 days. The mortality was 13.21% with an average age of 75 years for the period of the study. In conclusion, the majority of cases did not grow the most common types of microorganisms and most of these cases were covered only with the third generation cephalosporin. The severity of the cases on admission was not categorized based on any pneumonia scoring system. Therefore, there is a need for proper categorization of the sick patient who will need Intensive care admission. The anti-microbial were not based on any culture results but on clinical assessment in most of the cases for possible community acquired pneumonia. Therefore, this study could be an opportunity to improve the clinical pathway for treating these cases in order to improve their mortality and morbidity.
Keywords
INTRODUCTION
Community Acquired Pneumonia (CAP) is infection of the lung parenchyma acquired in the community in contrast to hospital acquired infection and a third group known as health care associated pneumonia. CAP is a leading cause of mortality and morbidity in the community particularly in elderly population, those with multiple co-morbidities and immunocompromised [1]. It affects 450 million people globally per year and results in 4 million deaths yearly [2]. The advances in antibiotic therapy and vaccines has improved survival in the 20th century after being regarded the “the captain of men death” in the 19th century [2]. The approach to patients with suspecting CAP begins with clinical evaluation combined with chest radiograph. The presence of a consolidation of or an infiltrate on any form of chest imaging is considered the gold standard in diagnosing pneumonia with the support of clinical evaluation and microbiological investigation(s) [1]. Pneumonia is caused mostly by bacteria and viruses and less commonly by fungal and parasite. Many strains are identified, but only few which are mainly responsible for the majority of the cases. In addition, mixed infection with bacteria and viruses are identified in 45% in children and 15% in adults. Approximately more than 50% of cases no organism is isolated [3].
A study conducted in Kingdom of Bahrain about patients admitted with CAP. It was designed to assess the main characteristics of the cases, the most prevalent organisms and the clinical outcome. In addition, the study would help in identifying the empiric antibiotic treatment, the antibiotic sensitivity of the most common organisms and the clinical response of the patients. This study should give us an idea about the epidemiology of the community acquitted pneumonia and appropriateness of the management in what considered to be the major tertiary care hospital in the kingdom.
MATERIALS AND METHODS
The study was conducted in Salmaniya Medical Complex in Kingdom of Bahrain. The hospital is the biggest tertiary care hospital on the island from the bed capacity (around 1200 beds) and technical perspective too. The study period was conducted from the 1st of October 2013 till the 31st of March 2014. This included the fall and the winter seasons where there is usually the highest rate of admission for CAP. It included all patients above 14 years of age who were admitted with diagnosis of pneumonia, based on the admitting physician’s diagnosis and according to ICD-10. The data was collected retrospectively going through the patients’ files. The hospital is paper based for documentation of patients’ records.
The data was gathered in a form designed by the study authors. It includes, in addition to the biographical data, the signs and symptoms on admission, the initial antibiotics used and whether they were adjusted during their hospital stay, all types of cultures, other relevant laboratory investigations results and the finally the outcome and complication of each patient. The ethical committee of the research committee in the hospital received the proposal of the study and an acceptance was gained before going ahead with the study. We included all patients that were admitted under the medical department with the diagnosis of pneumonia in that period. No patients were excluded. No consent was required as it was a retrospective study with no interference to patients’ management was done in any way. The patients’ confidentiality was maintained throughout the data collection and analysis. The diagnosis of pneumonia was based on the clinical impression of the admitting medical physicians and chest physician taking care of the patients. The data entrance and interpretation was done in an Excel program
RESULTS
The data collected was for patients diagnosed with pneumonia and were admitted during the study period. A total number of 159 were included.
The patients were 97 males (61.0%) and 62 of them females (38.99%). The average age of the patients was 58 years with the age ranging between 15 and 89 years. Those less than 20 years were 6 patient, 20-40 years were 31, 41-65 years were 51 and 71 patients 65 years or above. A significant number of patients had different co-morbidities. The co-morbidities were identified from the patients and from the previous medical records of the patients. The major co-morbidity which affected the patients was diabetes mellitus, in which 52 out of the 159 had it (32.70%). The next main chronic illness was underlying cardiac disease including hypertension with 28.30%. Chronic lung disease such as chronic obstructive airway and bronchial asthma was seen in 15.09% only. The rest of the patients had no co-morbidity with an estimate of 38.36%. Few of them had various chronic diseases such as heamoglobinopathy mainly sickle cell disease, chronic kidney disease, cancer and chronic liver disease (14.47%). Only one was known case of Human Immunodeficiency Virus. From the 159 patients only 31 of them were smokers but the number of cigarettes/packs/day was not documented in the files (Figure 1).
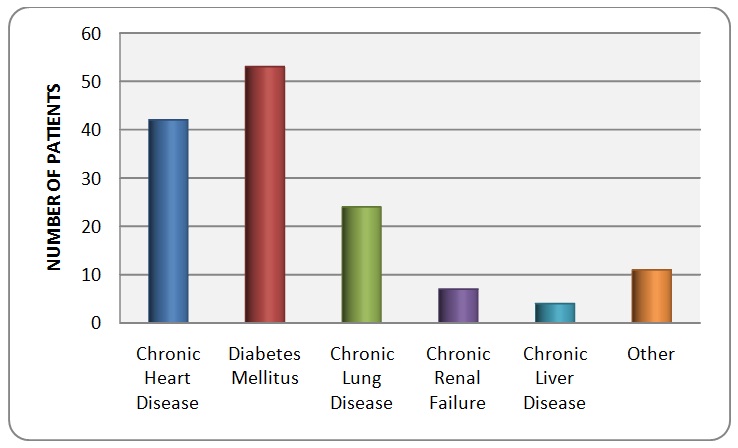
Figure 1: The co-morbidities present in the sample patients.
Regarding the symptoms upon presentation, 108 of them reported to have cough (67.90%). Of those, the cough was productive in 53, of them with only three had hemoptysis. Nine of the patients had dry cough and one patient on tracheostomy with excessive secretions via the tracheal opening. The rest of them (42.59%) nature of the cough was not specified due to errors in documentation in the medical records.
Other presenting symptoms were fever which was the main complaint in 91 of the patients (57.23%) and 62 complained of shortness of breath (62%). Other non specific symptoms were there too, such as decrease appetite which was mainly seen in the elderly population, non localized chest pain, rigors and decrease activity.
On reviewing the medical records of the patient, CURB-65 score was only calculated in seven patients upon admission. The score was ranging between 0-5 according to the patients’ clinical presentation. Two patients had score of five, two patients with a score of zero, one with a score of two; one had score of three and one with a score of one. Two of those seven patients who had a score of 5 and 3 were reported as mortality. Two who had a score of zero, one with a score of 2 and one had a score 5 were discharged home. So, those with higher CURB-65 score on admission had a worse outcome compared to the other group with the exception of one patient who was only 15 years old and according to the records had a rapid response to broad spectrum antimicrobials and no specific organism isolated.
The impression on admission of community acquired pneumonia for 124 patients out of the 159 (77.98%). On the other hand, 6 were admitted with hospital acquired pneumonia and twelve to rule out the possibility of Tuberculosis. The confirmation of the diagnosis of community acquired pneumonia versus hospital acquired pneumonia was done by an infectious disease specialist. Furthermore, 17 of the patients were admitted initially with different diagnosis but to be labeled later on during admission as pneumonia as they were misdiagnosed on fist encounter in the emergency department. Some of those known cases with sickle cell disease were admitted and managed initially as acute chest syndrome. Others admitted with acute kidney injury of unknown cause, left ventricular failure, fever for investigation or electrolyte imbalance.
Septic work-up was collected to all patients admitted and this included blood culture, urine culture and sputum/deep tracheal aspiration. Blood culture is done for 151 of the patients only. They were sterile in 139 (86.42%) of them and positive in 12. Those which were positive have grown different pathogens like Staphylococcus epidermidis (4 cases), Streptococcus pneumonia (1 case), Enterococcus vancomycin resistant (1 case), Acinetobacter multi-drug resistant (2 cases), carbapenem resistant klebsiella (2 cases) and providencia (1 case) (Figure 2).
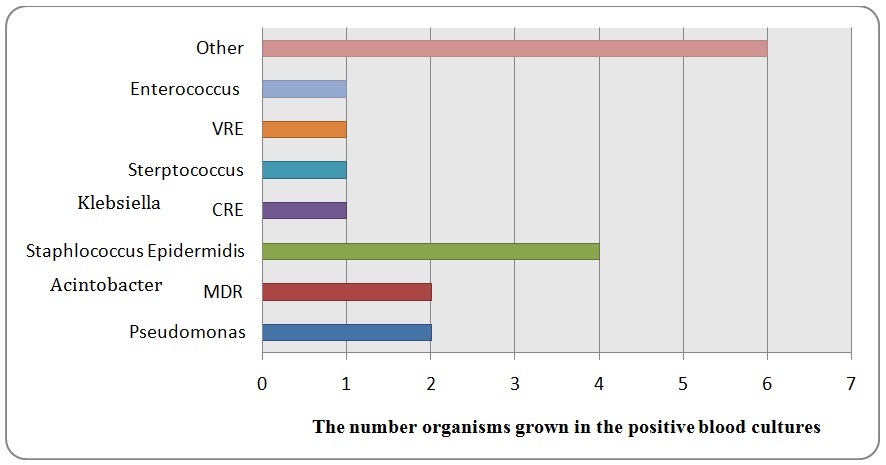
The blood cultures which have grown Staphylococcus epidermidis were repeated to all patients and the new sets were sterile. Therefore, most probably the first set was only skin contamination.
Deep tracheal aspiration or sputum culture and sensitivity was done in 137 out of the 159 patients. The rest, the test was not done or sample rejected from the laboratory. It has grown an organism(s) in 35 of them (25.55%) and they were sterile in 101 cultures (74.45%).
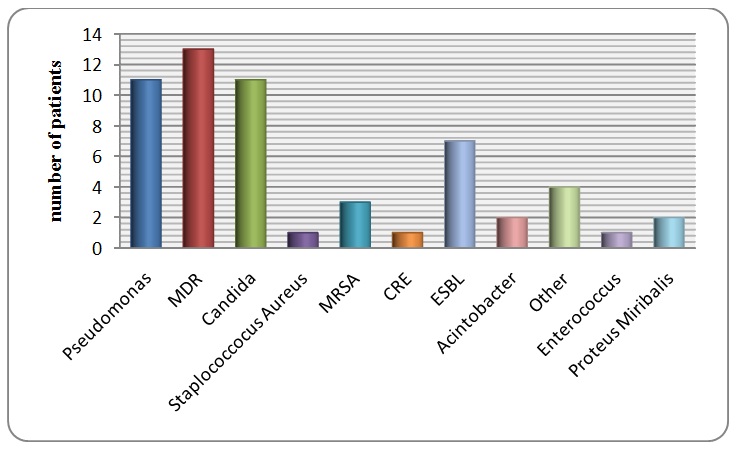
The main organisms grown were gram negative Multi-drug Resistant (MDR) organisms with 13 out of the 35 positive samples and they were Klebsiella, Acinetobacter or E coli. Other organisms grown were Candida (31.43%) which is most probably colonization of the tract, Pseudomonas (pan-sensitive and MDR) (31.43%) and gram negative Extended Spectrum B-lactamase (ESBL) (E coli, Klebsiella, and Proteus). Two cases grew Stenotrophomonas maltophili. Furthermore, four cases grew pan-sensitive gram negative organisms (E coli, Klebsiella and Enterobacter). Acid fast bacilli were not isolated even in the patients who were admitted with impression to rule out tuberculosis (Figure 3). Bronchial wash through bronchoscopy was done to seven patients and they grew organisms only in two of the samples. One grew Staphylococcus aureus (MSSA). On the other hand, H1N1 and corona virus Polymerase Chain Reaction (PCR) was done to ten patients and all samples were negative. Respiratory profile for other viruses and atypical organisms was done to 33 patients. It was positive to acute infection in seven patients where IgM antibody was isolated. They have shown Liogenella IgM in six and Coxiella Burntii IgM in one patient. However, 18 out of the 33 were either negative or positive to previous viral infections (i.e., IgG antibody) such as adenovirus. In addition, ten samples there were no results. However, the information of whether the septic work up collection was done before or after giving any dose of antibiotics could not be retrieved from the medical records.
Chest x-ray was done for total 157. The majority of the patients had lobar pneumonia (50.94%), 37 of them had bilateral infiltrates, two with multi-lobar patches, and 17 with pleural effusion of varying extent. On the other hand, 20 of the admitted patients had normal chest x-ray on admission (Figure 4).
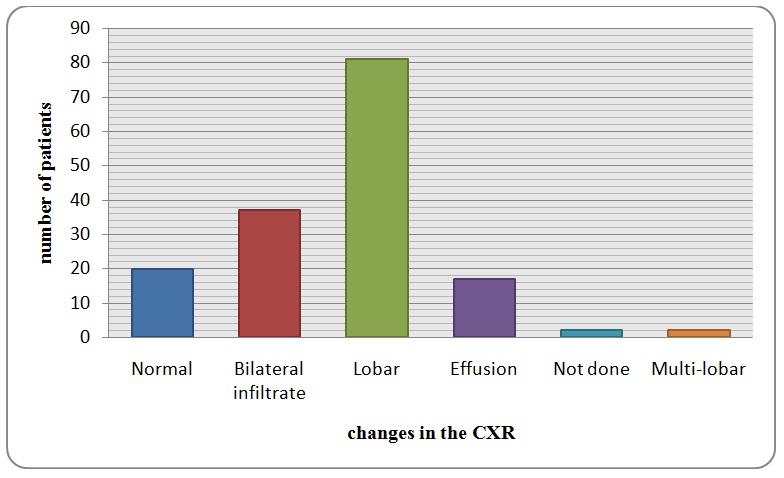
Figure 4: The pattern of lung involvement on the chest x-ray on admission.
Antibiotics were used to treat the underlying pneumonia. Multiple medications were used for the same patient whether at the same time or on successive periods during the same illness and hospital stay. The majority of patients were on Ceftriaxone (68.55%) and it was started as the first antimicrobial in almost all of the patients. it was used concurrently with macrolides group as Erythromycin (39.62%), clarithromycin (37.11%) or Azithromycin (19.50%). The initiation of ceftriaxone +/- macrolide was based on the international guidelines and recommendation as first line therapy for in-patients with CAP. Peperacillen/Tazobactam was the used frequently among the patients with 29.60%. It was prescribed usually as second line therapy once the Ceftriaxone fails to treat the underlying infection or with poor clinical response. Meropenem and Colistin were prescribed too with percentage of 21.39% and 8.18% respectively. They were started based on the isolation of MDR or ESBL organisms from the cultures. Vancomycin was used to cover the possibility of gram positive organism mostly empirically without isolating an organism even of subsequent cultures but due to clinical deterioration or persistent fever. Linezolid was used in three patients only as replacement to Vancomycin. Oseltamivir was prescribed in six patients to cover possibility of H1N1 or corona virus due to initial clinical suspicion. Anti-fungals prescribed just for two patients and they were Fluconazole and Capsofungin but unfortunately no clear explanation was mentioned in the patients’ records. Those who were discharged on oral antibiotics were given mostly Cloxacillin, Ciprofloxacin and Cefuroxime. Other antimicrobials were used infrequently such as Tigacyline and TrimeThoprim/Cotrimaxazole (Figure 5 and table 1).
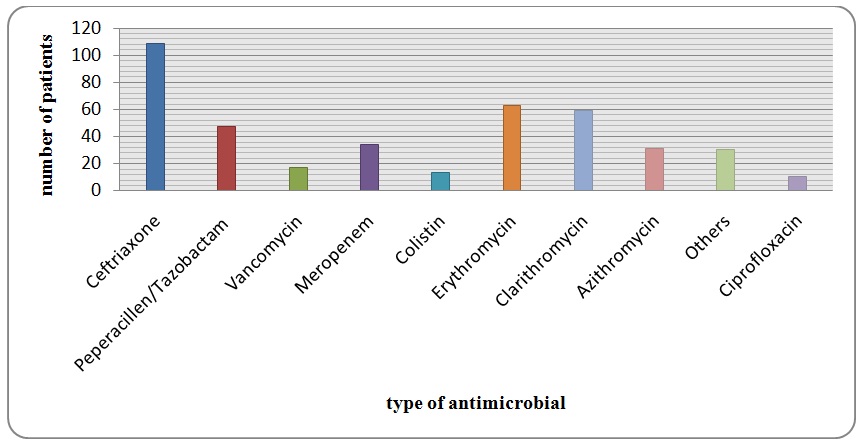
Figure 5: It summarizes the antimicrobials used among the patients.
| Antibiotics | Frequency used per patient | Antibiotics | Frequency used per patient |
| Ceftriaxone | 87 | Tegacycline | 11 |
| Erythromycin | 54 | Ciprofloxacin | 8 |
| Clarithromycin | 50 | Amoxicillin/ cluvanic acid | 6 |
| Meropenem | 30 | Oseltamivir | 5 |
| Azithromycin | 29 | Other | 19 |
| Peperacillen/Tazobactam | 39 | ||
| Vancomycin | 13 | ||
| Colistin | 11 |
Table 1: The frequency of antibiotics used among the patients.
The average stay for the patients was 15 days and only four of them who required Intensive Care Unit (ICU) admission during their hospital stay due to deterioration of their condition in the general medical ward. The case mortality rate was 13.21% with average age of 75 years. All mortalities took place in the hospital. There is no obvious correlation with the blood or DTA/sputum culture results. However, none of the mortality cases were admitted to the ICU and those who were admitted to the ICU had zero mortality.
DISCUSSION
The aim of our study was to evaluate the cases of CAP over a certain period and to appreciate the characteristics that would let us know where we stand in the diagnosis and management of the disease. What can be noticed that admissions assessment was not based on any scoring system particularly not on the CURB-65 scoring system? This would point to several down points which are: the admissions were based on personal judgment rather than scientific purposes, un-necessary admission which could add to the financial burden without any cost effectiveness. Similarly, Karmakar et al., showed only 5% application of the CURB65 score in a New Zealand hospital [4]. Another observation quality control study, which was done between 2001-2012 in Switzerland to show the effect of combining the prognostic biomarker Pro-adrenomedullin (ProADM) with CURB65 on the hospital stay of adults with pneumonia. The conclusion was that the use of ProADM in combination with CURB65 reduces the length of stay compared to the CURB65 score alone without apparent negative effects on patient safety [5].
Recently in the several few years the frequency of antimicrobial resistant organism has increased in the community and hospitals. This antimicrobial resistance is associated with increased mortality, morbidity and hospital cost [6]. The increased frequency of their spread is due to increase frequency of antimicrobial combination use and due to societal and technologic changes [6]. That was noticed by the results in our study in which the main organism isolated from the patients’ DTA/sputum was multi-drug resistant organisms. Antibiotic-resistant pathogens are not more virulent than sensitive ones: the same numbers of resistant and susceptible bacterial cells are required to produce the disease [7]. However, the resistant forms are harder to destroy. Those that are slightly insensitive to an antibiotic can often be eliminated by using more of the drug; those that are highly resistant require other therapies [7]. A study done in 2012 to test the effectiveness of using Tegacyline on patients with ventilator associated Acinetobacter MDR infection. The results showed that almost all the enrolled patients responded to the drug either alone or in combination with other antimicrobials [8]. Based on that, in our study actually Tegacyline was among medications least prescribed for the patient despite that most of the patient isolated MDR organism regardless of their mode of ventilation.
Few agents are available for the treatment of MDR infections especially when dealing with severe infections. The traditional antibiotics for MDR gram positive organisms are declining in efficacy gradually. What are currently available to treat them are Linezolid, Daptomycin, Tigecycline and Talavancin which is under trial. On the other hand for the gram negative pathogens the only available antimicrobials are Colistin and Tigecyline [9].
The traditional treatments for CAP are B-lactam and macrolides. New agents have been tested too and added to the standard treatment of pneumonia such as doxycycline and fluoroquinolones. Multiple studies have been done to compare different drug regimens but there were problems with interpretation of the results related to the study design. Such problem were: 1) small number of patients; 2) many of the studies were open label trials; and 3) the definition of CAP was not defined as in some studies no CXR was done or they were treating bronchitis’s [10].
Several retrospective studies have suggested that the addition of macrolides to the initial antibiotic regimen (usually cephalosporin) for in-patients is associated with decreased mortality and less hospital stay [11].
Another observational study done on patients with CAP requiring ICU care due to shock found that those who were treated with combination antibiotics (58 percent with a third-generation cephalosporin plus a macrolide) to a group treated with monotherapy (42 percent fluoroquinolone) had a higher 28-day in-ICU survival [12].
Looking at our results, the first line treatment were mostly a combination of drug rather than a monotherapy and B-lactams and Macrolides were the first drugs of choice. This reflects that the management is more of evidenced based rather than just a random choice at least on first encounter of the patient.
Mortality rates parallel the site of care of the patient. While outpatients have a risk of dying of <5%, those in hospital have a mortality rate of 12% and those managed in the ICU can have a chance of dying that exceeds 30% [13]. Delayed recognition of severe illness can add to mortality rate. The patients admitted to the ICU late in the course of disease have a higher mortality than those admitted early. Therefore, patient outcome and rate of death is dependent on making an accurate assessment about where patients should be initially managed and the intensity of care that they should receive [14]. A study done in Alberta, Canada enrolled 3284 patients to asses 30-day pneumonia related mortality and its correlation to Pneumonia Severity Index (PSI). There conclusion was that the long term mortality and morbidity are high following hospitalization for pneumonia and it is strongly correlated to the initial PSI score done on admission. The study showed 15% of patient with PSI I-II while 82% with class V died [15]. Comparing it to our results unfortunately most of our mortalities were outside the ICU and they were in the elderly age group. There are no rules in our institution for any limitation or restriction for the treatment of the elderly age group patients. However, generally the intensivist prefers to prioritize those with a younger age or expected better outcome to be shifted to the ICU. In addition, as mentioned previously no scoring system was used to assess the patients on admission (particularly CURB-65) which could have contributed to the mortality in our discussed cases as they did not receive the proper medical care according to their disease severity as there could be under-estimation of the seriousness of the condition.
The study had a couple of limitations: first is the limited number of the patients due to difficulties in getting the medical records of several patients and therefore, a prospective study would be a better future choice to avoid any missing data. Second, of all some of the patients were included as a case of pneumonia but their CXR’s were normal upon admission so that we could be dealing with simple bronchititis rather than CAP. In addition, lack of proper documentation of the time the septic work up was collected makes the interpretation and correlation of the culture results inappropriate. It also prevents us from accurately estimating the prevalence of organisms in the community and to create a national epidemiological chart. As a recommendation, further studies needed over a longer period to assess the prevalence of certain organisms causing CAP as it was noticed that a significant number had virulent organisms such as MDR.
CONCLUSION
CAP is a common health issue in the Kingdom of Bahrain with a significant mortality and morbidity especially among the elderly and those with co morbidities. It is the highest cause of mortality in the medical department in the major secondary and tertiary care hospital. It is clear that there is a high incidence of gram negative multidrug resistant organisms as an etiology for CAP. This has to be reflected on the proper choice of empiric antibiotic choice. The mortality is comparable to other local and international studies. The results of this can be used as the base for further studies to improve the microbiology diagnosis in these cases and to cover a longer period.
REFERENCES
- Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, et al. (2007) Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 44: 27-72.
- American Thoracic Society, Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171: 388-416.
- Hopstaken RM, Witbraad T, van Engelshoven JM, Dinant GJ (2004) Inter-observer variation in the interpretation of chest radiographs for pneumonia in community-acquired lower respiratory tract infections. Clin Radiol 59: 743-752.
- Karmakar G, Wilsher M (2010) Use of the ‘CURB 65’ score in hospital practice. Intern Med J 40: 828-832.
- Widmer D, Drozdov D, Rüegger K, LItke A, Arici B, et al. (2014) Effectiveness of Proadrenomedullin Enhanced CURB65 Score Algorithm in Patients with Community-Acquired Pneumonia in “Real Life”, an Observational Quality Control Survey. J Clin Med 3: 267-279.
- Cohen ML (1992) Epidemiology of drug resistance: implications for a post-antimicrobial era. Science 257: 1050-1055.
- Levy SB (1998) The challenge of antibiotic resistance. Sci Am 278: 46-53.
- Schafer JJ, Goff DA, Stevenson KB, Mangino JE (2007) Early experience with tigecycline for ventilator-associated pneumonia and bacteremia caused by multidrug-resistant Acinetobacter baumannii. Pharmacotherapy 27: 980-987.
- Orsi GB, Falcone M, Venditti M (2011) Surveillance and management of multidrug-resistant microorganisms. Expert Rev Anti Infect Ther 9: 653-679.
- Read RC (1999) Evidence-based medicine: empiric antibiotic therapy in community-acquired pneumonia. J Infect 39: 171-178.
- Stahl JE, Barza M, DesJardin J, Martin R, Eckman MH (1999) Effect of macrolides as part of initial empiric therapy on length of stay in patients hospitalized with community-acquired pneumonia. Arch Intern Med 159: 2576-2580.
- Dwyer R, Ortqvist A, Aufwerber E, Henriques Normark B, Marrie TJ, et al. (2006) Addition of a macrolide to a ss-lactam in bacteremic pneumococcal pneumonia. Eur J Clin Microbiol Infect Dis 25: 518-521.
- Brito V, Niederman MS (2010) Predicting mortality in the elderly with community-acquired pneumonia: should we design a new car or set a new ‘speed limit’? Thorax 65: 944-945.
- Restrepo MI, Mortensen EM, Rello J, Brody J, Anzueto A (2010) Late admission to the ICU in patients with community-acquired pneumonia is associated with higher mortality. Chest 137: 552-557.
- Johnstone J, Eurich DT, Majumdar SR, Jin Y, Marrie TJ (2008) Long-term morbidity and mortality after hospitalization with community-acquired pneumonia: a population-based cohort study. Medicine (Baltimore) 87: 329-334.
Citation: Al Salman J, Al Agha R, Al Tajer Z, Ali F, Al Junaid H, et al. (2015) Community Acquired Pneumonia in the Kingdom of Bahrain. J Infect Non Infect Dis 1: 008.
Copyright: © 2015 Jameela Al Salman, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.