
Efficacy of a 6-Week Mindfulness Intervention in Underserved Residents Receiving Treatment for Opioid Use Disorder during the COVID-19 Pandemic in New Jersey: A Multisite Pilot Feasibility Study
*Corresponding Author(s):
Suchismita RayDepartment Of Health Informatics, School Of Health Professions, Rutgers University, Office 173, 65 Bergen Street, Newark, New Jersey 07107, United States
Email:shmita@rutgers.edu
Abstract
Introduction: The United States is going through an opioid epidemic. Although the Medication Assisted Treatment (MAT) is the gold standard treatment for Opioid Use Disorder (OUD), many individuals with OUD relapse during/after treatment. Some of the core processes that may explain drug relapse are stress induced craving and emotional dysregulation and the MAT may not target these processes adequately. This pilot study was the first multisite study in New Jersey during the COVID-19 pandemic that was designed to evaluate the feasibility and efficacy of a 6-week mindfulness intervention as an adjunct to opioid addiction treatment in improving emotional dysregulation, perceived stress, sleep, and drug craving, in underserved individuals with OUD. Our mindfulness intervention was unique: first, it followed the “train-the-trainer” model and second, as a modification of the 8-week Mindfulness-Based Stress Reduction (MBSR) curriculum, it was less time consuming compared to the traditional program.
Methods: Twenty-nine (7 female) underserved low-income individuals with OUD took part in this study. They completed questionnaires pre- and post-MBSR and received weekly intervention.
Results: The mindfulness intervention was well received by the community adults who were seeking treatment for OUD during the COVID-19 pandemic. At post-intervention, participants showed significantly decreased perceived stress, difficulty in emotion regulation and drug craving while experiencing significantly improved sleep.
Conclusion: Our 6-week mindfulness intervention was effective in improving mental and physical health and reducing drug craving in underserved low-income individuals with OUD. Results have important implications in conducting a randomized control trial in the future that will further validate the efficacy of this intervention in underserved populations with OUD.
Keywords
Drug craving; Emotion regulation; Mental health; Mindfulness-based stress reduction; Opioid use disorder; Stress; Underserved population
Introduction
The United States is going through an opioid epidemic [1]. However, while opioid misuse and overdose deaths are on the rise for all Americans, underserved individuals in New Jersey are particularly vulnerable to opioid addiction [1,2]. Despite Medication Assisted Treatment (MAT) being the gold standard for Opioid Use Disorder (OUD), long term sobriety remains challenging, and enhanced emotional dysregulation, perceived stress, and craving are identified as underlying target processes. Both preclinical and clinical findings support this by showing that opioid maintenance treatments, including buprenorphine, inadequately block stress-provoked craving and motivation for opioids [3,4].
Mindfulness-Based Stress Reduction (MBSR) is a mind body complementary health approach developed by Jon Kabat-Zinn [5], the originator of mindfulness in the US, which defines mindfulness as “paying attention on purpose, in the present moment and non judgmentally.” MBSR has been demonstrated to improve emotional dysregulation, attention and mood in non-substance using individuals [6,7]. While one meta-analysis of over 200 mindfulness-based therapies found mindfulness to be effective across a variety of study populations including individuals with physical and medical conditions, psychological disorders, and non-clinical populations [8], another meta-analysis examining MBSR interventions found study populations were generally healthy, White Non-Hispanic individuals with higher income status [9]. Studies on mindfulness in underserved substance using individuals are scarce. We are aware of one 9-week Mindfulness-Based Relapse Prevention intervention study with female minority substance-users that showed decreased addiction severity and perceived stress [10], and one 8-week MBSR study that demonstrated the efficacy of the intervention in improving the health-related quality of life in opioid-using men undergoing MAT [11].
The present pilot study was the first multisite study in New Jersey designed to evaluate the feasibility and efficacy of a 6-week Mindfulness intervention during the COVID-19 pandemic, as an adjunct to opioid addiction treatment, in an underserved population. Objectives were to improve perceived stress, emotional dysregulation, sleep and opioid/drug craving in this population. The Mindfulness intervention used was a modification of the 8-week MBSR curriculum, and participants were classified as being underserved according to their residence, as defined by a needs assessment performed by the New Jersey Department of Children and Families in 2020. As stress from social isolation may be particularly compounded in underserved individuals with substance use disorders, a brief intervention targeting emotion regulation and provoked craving may be integral to the health of these individuals. Our Mindfulness protocol differed from the typical MBSR program in ways that made it uniquely designed for substance using populations. First, this study used the “train-the-trainer” model wherein one MBSR expert first trained clinicians from three addiction treatment sites in New Jersey in the 8-week MBSR program. The trained clinicians then delivered the Mindfulness intervention to their patients. Second, the time burden of this intervention on the patients was greatly reduced compared to the typical MBSR program (6 weeks vs. 8 weeks; one-hour vs. 2.5 to 3-hour weekly session; 10-min vs. 45 to 60 minutes of mindfulness practice each day; no retreat vs an all-day silent retreat), making more suitable to the needs of women.
We hypothesized that the Mindfulness program would be well received by the community adults who were undergoing addiction treatment for OUD during the COVID-19 pandemic. In addition, they would show attenuated craving, emotional dysregulation, perceived stress and sleep problems at the completion of the program.
Methods
Design
Prospective, non-blinded, single arm, 6-week intervention with standardized assessments design.
Study participants
Twenty-nine participants (mean age = 43 [12] years; 6 females) with OUD (diagnosed by the treatment sites) who were receiving addiction treatment at three treatment sites in New Jersey during October 2021-February 2022 took part in this Mindfulness study. Nineteen participants took part from Site 1, 5 participants took part from Site 2, and 5 participants took part from Site 3. Seven additional participants completed the pre-intervention questionnaires but did not participate in the intervention. Four clinicians from three treatment sites delivered weekly Mindfulness sessions. The racial distribution of study participants consisted of 60% White, 30% Black and 10% other. The average income of the participants was $22,482 ($24,533) [average income of Black participants: $16,888($13,392); average income of White participants: $22,294 ($23,504)]. According to the US Census Bureau, from 2016 to 2020 Residents in New Jersey experienced a median household income of $85,254 (in 2020 dollars) and a per-capita income of $44,153 (in 2020 dollars), putting the study participants at low-income level for the State. Additionally, some of the participants experienced homelessness at some point in their lives and some were court-mandated to undergo treatment.
Procedure
The MBSR expert in this study was trained by Jon Kabat-Zinn [5], and is a Ph.D. level clinician. The Mindfulness intervention was modeled after the extensively researched Stress Reduction Program at the Center for Mindfulness at UMass Medical School where the program was founded in 1979 by Jon Kabat-Zinn. The modified 6-week Mindfulness protocol retained the main components of the MBSR program including sitting meditation, awareness of breath, sensation in the body, soundscape, body scan, stress reactivity and stress reduction, mindful eating exercise, yoga, mindful movement, standing body scan, mindful eating, mindful communication, impact of mindful movement on thought, walking meditation, dyads etc. Mindfulness intervention was administered by the clinicians in-person if participants were receiving inpatient treatment or through a virtual platform if they were receiving outpatient treatment. The study was approved by the Rutgers University Institutional Review Board. Participants completed questionnaires pre- and post-the whole Mindfulness intervention and received an hour-long weekly intervention from their clinicians for 6 weeks in a group set up. Furthermore, participants practiced MBSR on their own for 10 minutes daily for 6 weeks using two MBSR audio tapes that were developed by our MBSR expert who received input from the treating clinicians during the audio development phase to make the audio appropriate for the underserved participants.
Data collection
Several questionnaires were administered pre- and post-Mindfulness: Perceived Stress Scale (PSS) [13], Difficulties in Emotion Regulation Scale (DERS) [14] and Sleep Quality Scale [15]. Craving for opioids was also collected pre- and post-Mindfulness on a 7-point scale, with 1 being the lowest craving and 7 being the highest craving. The data collection was performed on paper copies or on REDCap data collection software.
The Perceived Stress Scale (PSS): The PSS measures how often general situations in the past week are appraised as being stressful. It comprises a likert scale of 14-items, with scores for each item response ranging from 0 (never) to 4 (very often). Positive items are reverse coded. The total score ranges from 0-56.
The Difficulties in Emotion Regulation Scale (DERS): The DERS is a 41-item self-report developed to examine clinical difficulties in ability to regulate emotion. Participants are requested to rate how often statements such as “I feel at ease with my emotions” apply to them, where 1 is “almost never” (0-10%), 2 is “sometimes” (11-35%), 3 is “about half the time” (36-65%), 4 is “most of the time” (66-90%), 5 is “almost always” (91-100%). Items reflect difficulties within the following subscales: a) Non acceptance of emotional responses; b) difficulties engaging in goal-directed behavior; c) impulse control difficulties; d) lack of emotional awareness; e) limited access to emotion regulation; f) lack of emotional clarity. Positive items are reverse scored.
The opioid craving rating: This is a visual analog scale with a statement asking participants “how much are you craving opioids now”, and answers are anchored from 1 (not at all) to 10 (extremely).
The sleep quality scale: Comprises 28 items, evaluating six domains of sleep quality: daytime symptoms, restoration after sleep, problems initiating and maintaining sleep, difficulty walking and sleep satisfaction. Using a four-point, Likert-type scale, respondents indicate how frequently they exhibit certain sleep behaviors (0 = “few,” 1 = “sometimes,” 2 = “often,” and 3 = “almost always”).
Data analysis
All data were analyzed using the IBM SPSS Statistical Software Version 28.0. First, for each participant, the raw PSS, DERS, sleep and craving scores were calculated. Then, a within subjects t-test was performed on each data set to compare participants’ performance from pre- to post-Mindfulness.
Results
Our Mindfulness intervention was well received by the community adults who were seeking opioid addiction treatment during the COVID-19 pandemic. Study completion rate was high compared with other behavioral intervention studies [10]. Out of 37 participants who consented and completed the pre-intervention questionnaires, 30 participants (81%) completed all study requirements. Results demonstrated that at post-intervention (compared to pre-intervention), participants showed significantly decreased perceived stress (pre-intervention mean=20.10, post-intervention mean= 16.28, t(28) =2.86, p=0.004; Cohen’s d=0.53) (Figure 1), and significantly decreased difficulty in emotion regulation (pre-intervention mean=24.22, post-intervention mean= 16.48, t(26) =2.78, p=0.005; Cohen’s d=0.54) (Figure 2). They also showed significantly decreased opioid craving post-intervention (pre-intervention mean=2.59, post-intervention mean= 1, t(28) =9.86, p<0.001), and significantly decreased sleep problem (pre-intervention mean=24.28, post-intervention mean= 19.86, t(28) =3.08, p=0.004; Cohen’s d=0.54) (Figure 3).
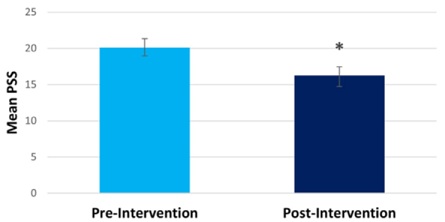 Figure 1: Compared to pre-intervention, participants experienced decreased perceived stress post-intervention.
Figure 1: Compared to pre-intervention, participants experienced decreased perceived stress post-intervention.
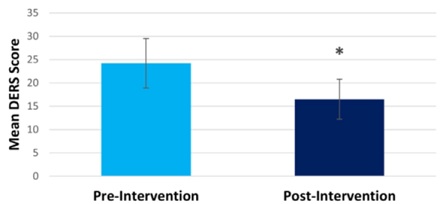 Figure 2: Compared to pre-intervention, participants experienced decreased difficulty in emotional regulation post-intervention.
Figure 2: Compared to pre-intervention, participants experienced decreased difficulty in emotional regulation post-intervention.
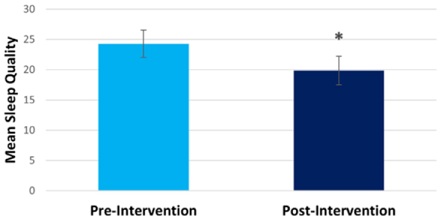 Figure 3: Compared to pre-intervention, participants experienced decreased sleep disturbance post-intervention.
Figure 3: Compared to pre-intervention, participants experienced decreased sleep disturbance post-intervention.
Discussion
The goal of this multisite study was to evaluate the feasibility and effectiveness of a brief Mindfulness intervention, modified from the 8-week MBSR curriculum, in underserved individuals with OUD who were undergoing addiction treatment in New Jersey. Our Mindfulness intervention was unique for two reasons: it utilized a “train-the-trainer” model, and it significantly reduced the time burden on the participants compared to the typical MBSR intervention. To the best of our knowledge, this pilot 6-week Mindfulness multisite study appears to be the first in New Jersey in an underserved low-income population of opioid users. Consistent with our first hypothesis, our intervention was well received by the community adults who were seeking treatment for OUD during the COVID-19 pandemic. Our first hypothesis was that the Mindfulness program would be well received by the community adults who were undergoing addiction treatment for OUD during the COVID-19 pandemic.
Consistent with our second hypothesis, the intervention was effective in reducing perceived stress and opioid craving in low-income patients with OUD. The intervention furthermore improved the patient’s sleep and participants’ ability to regulate their emotions. During the COVID pandemic while the study participants were undergoing additional stresses, this low-dose mindfulness intervention was efficacious in improving their mental and physical health as well as opioid craving. This study further highlights that although the participants were undergoing substance addiction treatment, they were still experiencing moderate perceived stress, dysregulated emotion, disturbed sleep and craving compared to norms at pre-intervention. This finding is consistent with the literature which indicates that substance addiction treatment including MAT alone may not be adequate in targeting regulatory and affective mechanisms underpinning emotional dysregulation, stress and drug craving; all of which are hallmark characteristics of relapse [3,4]. Thus, based on these findings we suggest that this 6-week intervention could be offered as an adjunct to the addiction treatment for individuals with OUD to improve treatment outcomes.
Significant clinical benefits using a 6-week Mindfulness protocol compared to the typical 8-week MBSR protocol is promising, and suggests that this behavioral intervention will be well received by the OUD patients and result in positive treatment outcomes in a shortened time frame in the future studies. Importantly, this 6-week Mindfulness intervention will be more suitable to the needs of women as women in general and particularly women with children face challenges in completing their addiction treatment. The present results will form the basis for a larger controlled clinical trial required to more thoroughly validate the efficacy of this brief intervention. The proposed trial will include substance use outcomes in addition to drug craving, mental and physical health outcomes in underserved low-income populations with substance use disorders. Finally, the train-the-trainer model can be convenient and cost-effective for the treatment centers; once their clinicians are trained in the MBSR program, they can use this intervention as an adjunct to their standard treatment protocols for their patients on an ongoing basis.
Declaration of Competing Interest
The authors declare that they have no known competing financial interest or personal relationship that could have appeared to influence the work reported in this article.
Funding Information
This project was funded by a Healthcare Foundation of New Jersey grant (Award# 3888) to Dr. Suchismita Ray.
Acknowledgement
We acknowledge Melanie Dejesus, Robert Budsock (President and CEO of Integrity House; Site1), Eman Gibson (Chief Clinical Officer of Integrity House; Site 1), Anthony Lucibello (Executive Director of Northwest Essex Community Healthcare Network; Site 2), Eucaris Montanez (CCBHC Projects Officer, Northwest Essex Community Healthcare Network; Site 2), Dr. Gregory Benson (Director of Psychology Training, Rutgers Biomedical and Health Sciences; Site 3), and Dr. Petros Levounis (Professor and Chair of the Department of Psychiatry at Rutgers New Jersey Medical School) for helping with the administrative aspects of this project. We also acknowledge Dr. Jim Handlin for training the clinicians in MBSR and developing the 6-week mindfulness intervention protocol for this project.
References
- Substance Abuse and Mental Health Services Administration (2020) Behavioral Health Equity. SAMHSA, Rockville, USA.
- Substance Abuse and Mental Health Services Administration (2020) The Opioid Crisis and the Hispanic/Latino Population: An Urgent Issue. SAMHSA, Rockville, USA.
- Sorge RE, Rajabi H, Stewart J (2005) Rats maintained chronically on buprenorphine show reduced heroin and cocaine seeking in tests of extinction and drug-induced reinstatement. Neuropsychopharmacology 30: 1681-1692.
- Leri F, Tremblay A, Sorge RE, Stewart J (2004) Methadone maintenance reduces heroin- and cocaine-induced relapse without affecting stress-induced relapse in a rodent model of poly-drug use. Neuropsychopharmacology 29: 1312-1320.
- Kabat-Zinn J (1982) An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. Gen Hosp Psychiatry 4: 33-47.
- Kilpatrick LA, Suyenobu BY, Smith SR, Bueller JA, Goodman T, et al. (2011) Impact of mindfulness-based stress reduction training on intrinsic brain connectivity. Neuroimage 56: 290-298.
- Goldin PR, Gross JJ (2010) Effects of Mindfulness-Based Stress Reduction (MBSR) on Emotion Regulation in Social Anxiety Disorder. Emotion 10: 83-91.
- Khoury B, Lecomte T, Fortin G, Masse M, Therien P, et al. (2013) Mindfulness-based therapy: A comprehensive meta-analysis. Clin Psychol Rev 33: 763-771.
- Khoury B, Sharma M, Rush SE, Fournier C (2015) Mindfulness-based stress reduction for healthy individuals: A meta-analysis. J Psychosom Res 78: 519-528.
- Amaro H (2014) Implementing mindfulness-based relapse prevention in diverse populations: Challenges and future directions. Subst Use Misuse 49: 612-616.
- Hosseinzadeh Asl NR, Hosseinalipour F (2014) Effectiveness of mindfulness-based stress reduction intervention for health-related quality of life in drug-dependent males. Iran Red Crescent Med J 16: 12608.
- Volkow ND (2020) Collision of the COVID-19 and Addiction Epidemics. Ann Intern Med 173: 61-62.
- Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24: 385-396.
- Gratz KL, Roemer L (2004) Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. J Psychopathol Behav Assess 26: 41-54.
- Yi H, Shin K, Shin C (2006) Development of the Sleep Quality Scale. J Sleep Res 15: 309-316.
Citation: Ray S, Kennelly N, Fox HC, Greendyk S, Hipol-Ligot C, et al. (2022) Efficacy of a 6-Week Mindfulness Intervention in Underserved Residents Receiving Treatment for Opioid Use Disorder during the COVID-19 Pandemic in New Jersey: A Multisite Pilot Feasibility Study. J Addict Addictv Disord 9: 104.
Copyright: © 2022 Suchismita Ray, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

