
Evaluation of the Use of Neuro Muscular Taping (NMT) in the Treatment of Postoperative Edema in Acute ACL Repair Surgery
*Corresponding Author(s):
Andrea Del DucaOrthopaedic Unit And Kirk Kilgour Sports Injury Centre, S. Andrea Hospital, University Of Rome La Sapienza, Rome, Italy
Tel:+39 3391211498,
Email:andreadelduca13@gmail.com
Abstract
Background: Surgical techniques for the treatment of Anterior Cruciate Ligament (ACL) injuries are exponentially improved in the past few decades. Nevertheless, edema and pain commonly accompany post-surgical procedures and when excessive, can adversely affect the healing course. In recent years, Neuro Muscular Taping (NMT) has been proposed as a new technique for the treatment of post-operative edema.
Objective: In this study, we aimed to investigate the effects Neuro Muscular Taping (NMT) in the treatment of edema in the acute and post-acute postoperative phases of ACL repair surgery.
Methods: Thirty patients (19 M, 11F; mean age: 27 y/o) with ACL injury were randomly assigned to two groups for the rehabilitation program: (1) An experimental group to receive a NMT treatment; or (2) A control group which underwent the standard-of-care rehabilitation protocols. Both groups where weekly monitored for 4 weeks after the surgery. Swelling was assessed through measurement of the limb circumference; post-operative pain was evaluated with VAS. After collection, data were processed by means of the Mann-Whitney and Wilcoxon statistical tests, through which we evaluated the percentage decrease in knee swelling of the operated limb.
Results: In comparison to the control group, the experimental group showed significant improvements in swelling and pain. The circumference of the operated limb registered was: -2.4% ±0.1 in the NMT-treated group and + 0.3% ±0.2 in the control group in the first week (p = 0.030), -3.7% ±0.1 in the NMT-treated group and -0.63% ±0.3 in the control group in the second week (p = 0.038), -4.5% ±0.1 in the NMT-treated group and -1.2% ±0.3 in the control group in the third week (p = 0.019), -5.8% ±0.1 in the NMT-treated group and -2.4% ±0.3 in the control group in the fourth week (p = 0.019). VAS in the first week was 3.11 ±01.05 in NTM-treated group and 4.67 ±0.71 in the control group (p = 0.006). Our data showed a statistically significant reduction of the mean circumference of the lower limb at each time point and the reduction of mean VAS at the first week treated with NMT compared to the control group (p < 0.05).
Conclusion: Our results revealed that NMT technique applied in the acute rehabilitation program of ACL surgery is effective in the treatment of postoperative edema.
Keywords
Anterior Cruciate Ligaments (ACL) ruptures; Lachman test; Neuro muscular taping; Pivot Shift; Surgery
INTRODUCTION
Anterior Cruciate Ligament (ACL) injury is one of the most common knee injuries [1]. It is estimated to occur in more than 2 million subjects per year worldwide [2,3]. Those primarily affected are athletes between the ages of 15 and 30 [4]. Despite the high incidence of ACL rupture, a univocal strategy for the management of this condition is missing [5-7]. The therapeutic strategies include two main options which contemplate an early surgery within 24 hours after the trauma, or a more conservative approach aimed to stabilize the clinical conditions of the knee before surgery.
Several studies advocates for an early intervention approach as it is linked to more favorable outcomes such as reduction of immobilization time and muscle tone preservation, early rehabilitation process and consequently optimization of recovery time and return to sport [8-12]. The reduction of immobilization time allowed the implementation of accelerated rehabilitation treatment programs aimed to obtain a rapid recovery of daily life activities and early return to sports [13]. Nevertheless, edema and pain commonly accompany orthopedic post-surgical procedures and when excessive, can adversely affect the postoperative course [14]. Thus, effective rehabilitation strategies for the management of these common post-surgery side effects play a fundamental role in the proper healing after acute ACL surgery.
In recent years, Neuro Muscular Taping (NMT) has been proposed as a new effective technique for the treatment of post-operative edema [15]. NMT is a biomechanical, non-pharmacological technique consisting in the application on the skin of a mono-elastic adhesive tape that allows for improved blood and lymphatic circulation in the treated area [16]. The NMT applied to the skin form wrinkles which, by lifting the epidermis, facilitate lymphatic drainage, promote cellular metabolism and vascularization, reduce pain and improve the Range Of Motion (ROM) [17,18].
The hypothesis of the present study is that the application of NMT reduces postoperative edema after ACL repair surgery.
MATERIALS AND METHODS
Population characteristics
Thirty patients (19M, 11F; mean age 27, range 16-46 y/o) were enrolled in the study and randomized into an experimental group (treated with NMT, n=15, n=15; 11 male and 4 female) and a control group (treated according the standard-of-care, without NMT; 9 male and 6 female patients). Demographic characteristics are shown in table 1.
From January 2019 to November 2020 patients aged between 15 and 50 y/o, candidate to ACL repair surgery and who met the inclusion and exclusion criteria were enrolled in the study after institutional local IRB-approval. Exclusion criteria were Surgical Site Infection (SSI), non-intact skin, cancer and metastases, and deep vein thrombosis.
Study design
A standardized 2-phase-protocol was used in the postoperative days. The first phase (acute-phase), included from the first post-operative day until day 14 (week 2) and it was characterized by the application of 1cm-long draining tape strips, spaced 1cm apart and positioned, without anchorage, in the area affected by the edema (Figure 1A). The second phase (post-acute phase), went from week 2 until week 4 after surgery. In this phase, a fan taping was applied on the popliteal fossa along with a double-fan taping placed on the anterior part of the knee (Figures 1B-C).
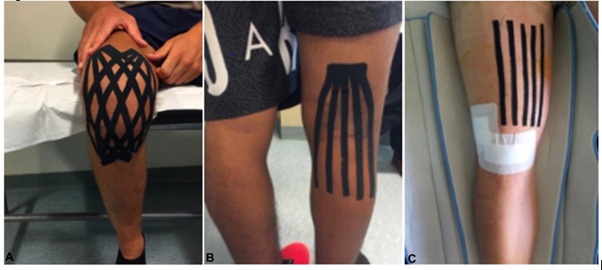 Figure 1: NMT positioning on the knee. 1A) Draining strips in the acute phase; 1(B-C)) fan-shaped strips in the post-acute phase.
Figure 1: NMT positioning on the knee. 1A) Draining strips in the acute phase; 1(B-C)) fan-shaped strips in the post-acute phase.
To assess the decrease in edema, the circumference of the operated lower limb was measured at T0 (first post-operative day) and every week for 4 weeks. The measurement was performed 2cm above the upper margin of the patella (Figures 2-3).
 Figure 2: Repair point for the measurement of the circumference of the knee.
Figure 2: Repair point for the measurement of the circumference of the knee.
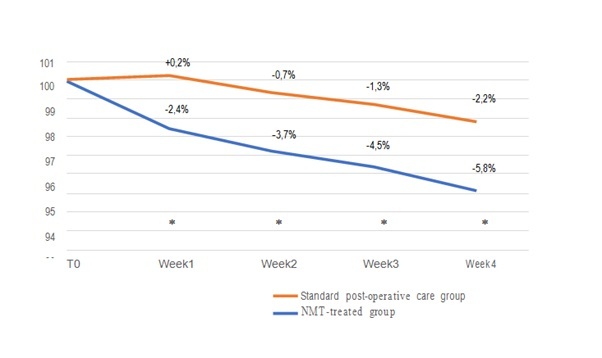 Figure 3: Edema reduction overtime in the NTM-treated group vs the control group after ACL surgery. Values are presented as a difference from T0 (the first post-operative day) at each time-point. Red Line: standard post-operative care group; Blue line: NMT-treated group (P < 0.05).
Figure 3: Edema reduction overtime in the NTM-treated group vs the control group after ACL surgery. Values are presented as a difference from T0 (the first post-operative day) at each time-point. Red Line: standard post-operative care group; Blue line: NMT-treated group (P < 0.05).
NMT application
All patients enrolled in the study received standard rehabilitation treatment according to the post-intervention ACL repair protocols. The NMT-treated group underwent additional treatment with NMT. The tape was applied to the knee surface area in order to form folds that lifted the skin layer, reducing the underlying pressure and removing congestion by normalizing the pressure of the capillaries as previously described [19]. The application of the tape produces an eccentric biomechanical action, which is activated by normal body movement [20]. The taping method used in the study consist in the application of fan-shaped taping and draining strips, with or without anchorage, spaced one centimeter apart, placed in the edematous area of the knee.
For the acute phase, five strips of 1cm-wide tape, without anchorage, were applied to the proximal area of the knee in order to drain the post-operative edema. Tape strips were applied one centimeter apart with patients lying in supine position. In the post-acute phase, 3 fan-shaped tapes were applied on the area of the knee. The first anterior fan was anchored 5cm above the patella, 1cm medial to the midline of the femur with 25° tilt. The patient was instructed to maintain a knee flexion angle of 90° in the anchoring phase, and then to hold a flexion angle of 110° while fixing the tape to the lower area of the knee. In case the patient could not reach 110° flexion angle, the tape was fixed at the maximum flexion feasible, pulling the quadriceps skin toward the groin area. The tape strips covered the area within the margins of medial and lateral collateral ligament. The second anterior fan was anchored on the quadriceps, 1cm lateral to the midline of the femur with 25° tilt. Finally, the posterior fan was anchored 10cm above the popliteal fossa and its length was 20-25 cm depending on patient’s height. To position the posterior fan, the patient was still standing with the knee extended as much as possible. The lateral strip was placed following the margin of the biceps femoris while the medial strips followed the margin of semitendinosus tendon. The tape was replaced every week to guarantee the adequate elasticity.
Statistical analysis
Data were processed using the Mann-Whitney and Wilcoxon statistical test and SPSS software, through which we evaluated the percentage decrease in knee swelling of the operated limb in the two different groups: the experimental group (treated with NMT) and in the control group (treated the standard-of-care). Statistical significance was assessed through Mann-Whitney test (p < 0.05).
RESULTS
A total of 18 patients admitted to our department with acute ACL injuries who met the inclusion and exclusion criteria were enrolled in this study. Patients were randomized either in the experimental group (NMT-treatment group) or in the control group (standard-of-care treatment group). The mean age of our cohort was 27 years old (range 16-46 years). No statistically significant differences were observed between the groups at baseline (demographic Table 1).
|
|
NMT-treated group (N=15) |
Standard-of-care treated group (N=15) |
P-value |
|
Gender (M/F) |
11/4 |
9/6 |
N.S. |
|
Age mean (range) |
26 |
28 |
N.S. |
|
Ethnicity |
100% Caucasian |
100% Caucasian |
N.S. |
Table 1: Demographic characteristic.
The circumference of the operated limb was measured in each patient as described in the methods, at T0 (first post-operative day) and every week until week 4. The results were recorded as the percentage respect to the circumference at time 0: circumference at T (1-2-3-4)/circumference at T0 x 100. Thus, the collected data were analyzed through Mann-Whitney and Wilcox on statistical tests.
The circumference of the operated limb registered in the NMT-treated group, was: -2.4% ±0.1 in the first week, -3.7% ±0.1 in the second week, -4.5% ±0.1 in the third week, -5.8% ±0.1 in the fourth week (Table 2). The circumference of the operated limb registered in the control group, was: +0.3% ±0.2 in the first week, -0.63% ±0.3 in the second week, -1.2% ±0.3 in the third week, -2.4% ±0.3 in the fourth week (Table 2). The differences between the two groups were statistically significant (p < 0.05) at all the different follow-up (Table 2).
|
|
All studied population |
Standard-care-treated group (N=15) |
NMT-treated group (N=15) |
P-value |
|||
|
Decrease % from T0 |
Mean |
Std. |
Mean |
Std. |
Mean |
Std. |
|
|
1 Week |
.9897 |
.02490 |
1.0028 |
.02679 |
.9754 |
.01548 |
.030 |
|
2 Week |
.9789 |
.02727 |
.9937 |
.02946 |
.9630 |
.01620 |
.038 |
|
3 Week |
.9718 |
.02828 |
.9877 |
.03084 |
.9552 |
.01577 |
.019 |
|
4 Week |
.9594 |
.02832 |
.9758 |
.02969 |
.9422 |
.01675 |
.019 |
Table 2: Mean percentage of reduction from T0 in the study groups at several time-points.
The VAS registered in NMT group was: 5.78 ±1.56 at T0 (first post-operatively day), 3.11 ±1.05 in the first week, 2.11 ±0.6 in the second week, 1.33 ±0.50 in the third week, 1.33 ±0.50 in the fourth week (Table 3). The VAS registered in the control group was: 6-78 ±1.39 at T0 (first post-operatively day), 4.67 ±0.71 in the first week, 2.33 ±0.71 in the second week, 1.44 ±0.53 in the third week, 1.22 ±0.44 in the fourth week (Table 3). The differences between the two groups were statistically significant (p<0.05) at all the different follow-up (Table 3).
|
|
Standard-care-treated group (N=15) |
NMT-treated group (N=15) |
P-value |
||
|
VAS |
Mean |
Std. |
Mean |
Std. |
|
|
T0 first day after surgery |
6,78 |
1,39 |
5,78 |
1,56 |
N.S. |
|
1 Week |
4,67 |
,71 |
3,11 |
1,05 |
0.006 |
|
2 Week |
2,33 |
,71 |
2,11 |
,60 |
N.S. |
|
3 Week |
1,44 |
,53 |
1,33 |
,50 |
N.S. |
|
4 Week |
1,22 |
,44 |
1,33 |
,50 |
N.S. |
Table 3: Mean VAS from T0 in the study groups at several time-points.
DISCUSSION
ACL injury represents one of the most common injuries in orthopedics and sports medicine in the athletically active population [1,4]. It often leads to instability, reduced function, and associated cartilage and meniscal injuries that contribute to the possible development of early post-traumatic arthrosis [21,22]. Several surgical therapeutic options are currently available for the reconstruction of the ACL [23].
Recently, the prompt repair of the Anterior Cruciate Ligament (ACL) has been proposed as therapeutic option. In this technique, the injured ligament is sutured without the use of tendon harvesting thus, avoiding any don site morbidity. Arthroscopic ACL repair performed acutely reveals many advantages such as avoiding loss of muscle strength and allowing an early rehabilitation process thus optimizing recovery time [24].
To date, there is no evidence in the literature regarding appropriate rehabilitation strategies after ACL repair. Rehabilitation protocols are therefore extrapolated from those described in the ACL reconstruction literature. Although subjects reported lower operative morbidity and faster recovery after ACL repair, no study provided data supporting the safety and efficacy of the accelerated rehabilitation pathway compared to that following reconstruction of the injured ligament. The main goal of rehabilitation treatment following ACL repair is to recover ROM, muscle strength and daily and sports specific activities.
In the first phase of rehabilitation study (1st to 4th week) the main objectives are: control of pain and edema, muscle recruitment and gradual restoration of ROM through active and passive mobilization of the operated limb. Moreover, strengthening of the quadriceps muscle through the execution of isometric exercises and stretching of the muscles of the posterior chain of the operated limb are required.
In this study we focus on the first phase of rehabilitation and the possible use of neuromuscular taping as a technique for the treatment of edema in the immediate post-operative period. The use of this technique allows acting from the outside, through the application of an elastic adhesive tape on the surface of the skin, to obtain a decompressive effect.
In this study, two groups of patients undergoing ACL repair surgery were compared: an experimental group treated with neuromuscular taping and a control group. The comparison of the data obtained showed that the correct use of the NMT technique allows reducing the edema present in the immediate post-operative period. Moreover, we also found a significative reduction of post-operative pain as evaluated with VAS in the experimental group at first week evaluation. We could speculate that the significative reduction in swelling at the first week, due to the application of the NMT, could also lead to the reported reduction in pain. To our knowledge there are no other papers evaluating the benefits of NMT in the reduction of postoperative edema after ACL repair. For this reason, it is difficult to find support in the literature for the positive result highlighted by this study regarding the percentage decrease in swelling of the operated knee.
This study presents a few limitations such as the small sample size due to the worldwide SARS-CoV pandemic and the choice of ACL repairs intervention. Nevertheless, we were able to detect significant differences between the studied groups.
In conclusion, the NMT technique, correctly used, seems to be effective in the treatment of edema secondary to ACL repair surgery. The neuromuscular taping was able to induce a rapid and significant reduction of the edema and pain of the operated limb, evaluated by measuring the circumference of the thigh at supra-traumatic level and with VAS, compared to the control group that did not receive the treatment.
REFERENCES
- Blaker CL, Zaki S, Little CB, Clarke EC (2020) Long-term Effect of a Single Subcritical Knee Injury: Increasing the Risk of Anterior Cruciate Ligament Rupture and Osteoarthritis. Am J Sports Med PubMed Id: 363546520977505.
- Renstrom PA (2013) Eight clinical conundrums relating to anterior cruciate ligament (ACL) injury in sport: recent evidence and a personal reflection. Br J Sports Med 47: 367-372.
- Friel NA, Chu CR (2013) The role of ACL injury in the development of posttraumatic knee osteoarthritis. Clin Sports Med 32: 1-12.
- Cancienne JM, Browning R, Werner BC (2020) Patient-Related Risk Factors for Contralateral Anterior Cruciate Ligament (ACL) Tear After ACL Reconstruction: An Analysis of 3707 Primary ACL Reconstructions. HSS J 16: 226-229.
- Lansdown DA, Riff AJ, Meadows M, Yanke AB, Bach BR Jr. (2017) What Factors Influence the Biomechanical Properties of Allograft Tissue for ACL Reconstruction? A Systematic Review. Clin Orthop Relat Res 475: 2412-2426.
- Chambat P, Guier C, Sonnery-Cottet B, Fayard JM, Thaunat M (2013) The evolution of ACL reconstruction over the last fifty years. Int Orthop 37: 181-186.
- Smigielski R, Zdanowicz U, Drwiega M, Ciszek B, Williams A (2016) The anatomy of the anterior cruciate ligament and its relevance to the technique of reconstruction. Bone Joint J 98: 1020-1026.
- Burnett RA, Westermann R, Duchman K, Amendola N, Hettrich C, et al. (2019) Intra-Articular Pathology Associated with Acute and Chronic Anterior Cruciate Ligament Reconstruction. Iowa Orthop J 39: 101-106.
- Filbay SR, Roos EM, Frobell RB, Roemer F, Ranstam J et al (2017) Delaying ACL reconstruction and treating with exercise therapy alone may alter prognostic factors for 5-year outcome: an exploratory analysis of the KANON trial. Br J Sports Med 51: 1622-1629.
- Medvecky MJ, Tomaszewski P (2015) Management of Acute Combined ACL-Medial and Posteromedial Instability of the Knee. Sports Med Arthrosc Rev 23: 7-14.
- Monk AP, Davies LJ, Hopewell S, Harris K, Beard DJ et al. (2016) Surgical versus conservative interventions for treating anterior cruciate ligament injuries. Cochrane Database Syst Rev 4: 011166.
- Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M (1991) Arthrofibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. Am J Sports Med 19: 332-336.
- Cavanaugh JT, Powers M (2017) ACL Rehabilitation Progression: Where Are We Now? Curr Rev Musculoskelet Med 10: 289-296.
- Nekoroski T, Paladini RD, Sauder DN, Frost GI, Keller GA (2014) A recombinant human hyaluronidase sustained release gel for the treatment of post-surgical edema. Int J Dermatol 53: 777-785.
- Pillastrini P, Rocchi G, Deserri D, Foschi P, Mardegan M, et al. (2016) Effectiveness of neuromuscular taping on painful hemiplegic shoulder: a randomised clinical trial. Disabil Rehabil 38: 1603-1609.
- Emery CA, Pasanen K (2019) Current trends in sport injury prevention. Best Pract Res Clin Rheumatol 33: 3-15.
- Rahlf AL, Braumann KM, Zech A (2019) Kinesio Taping Improves Perceptions of Pain and Function of Patients with Knee Osteoarthritis: A Randomized, Controlled Trial. J Sport Rehabil 28: 481-487.
- Edmonds DW, McConnell J, Ebert JR, Ackland TR, Donnelly CJ (2016) Biomechanical, neuromuscular and knee pain effects following therapeutic knee taping among patients with knee osteoarthritis during walking gait. Clin Biomech (Bristol, Avon) 39: 38-43.
- Martonick N, Kober K, Watkins A, DiEnno A, Perez C, et al. (2020) The Effect of Kinesio Tape on Factors for Neuromuscular Control of the Lower-Extremity: A Critically Appraised Topic. J Sport Rehabil 1-6.
- Yeung SS, Yeung EW, Sakunkaruna Y, Mingsoongnern S, Hung WY et al. (2015) Acute effects of kinesio taping on knee extensor peak torque and electromyographic activity after exhaustive isometric knee extension in healthy young adults. Clin J Sport Med 25: 284-290.
- Ferretti A, Conteduca F, De Carli A, Fontana M, Mariani PP (1991) Osteoarthritis of the knee after ACL reconstruction. Int Orthop 15: 367-371.
- McKeon BP, Bono JV, Richmond JC (2009) Knee Arthroscopy. Springer, New York, USA.
- Monaco E, Fabbri M, Lanzetti RM, Del Duca A, Labianca L, et al. (2017) Biomechanical comparison of four coupled fixation systems for ACL reconstruction with bone socket or full-tunnel on the tibial side. Knee 24: 705-710.
- Ferretti A, Monaco E, Annibaldi A, Carrozzo A, Bruschi M, et al. (2020) The healing potential of an acutely repaired ACL: a sequential MRI study. J Orthop Traumatol 21: 14.
Citation: Duca AD, Monaco E, Angí E, Duca MD, Marzilli F, et al. (2021) Evaluation of the Use of Neuro Muscular Taping (NMT) in the Treatment of Postoperative Edema in Acute ACL Repair Surgery. J Orthop Res Physiother 7: 051.
Copyright: © 2021 Andrea Del Duca, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

