
Feasibility of Virtual Reality-Delivered Transcending Self Therapy in Veterans Undergoing Residential Substance Use Treatment
*Corresponding Author(s):
Zaur AJRichmond Veterans Administration Medical Center, 800 E Leigh Street, PO Box 980126, Richmond, VA 23298, United States
Tel:+1 6306052954,
Email:angelazaur@gmail.com
Abstract
Substance Use Disorder (SUD) is common among military veterans, where post-traumatic stress disorder and other comorbidities stemming from deployment or other military experiences increase the severity of SUD and incidence of relapse. It is thus critical to discover and evaluate potential advances in SUD treatment, such as methods for enhanced patient engagement in treatment. Transcending Self Therapy (TST) was developed as a specialized individual or group cognitive behavioral therapy with psychoeducation content that focuses on a person’s moral compass and ideal as a beacon when solving psychosocial challenges and stressors that are common in veterans. We recently developed a program for potentially enhancing patient engagement in TST that offers an aesthetically appealing Virtual Reality (VR) environment for engaging in TST material (TST-VR). The therapeutic contents are available ad libitum and are navigable by VR goggles and hand controls. In a feasibility study of 37 veterans in residential treatment, we report here that veterans found VR-based TST (TST-VR) engaging and well-tolerated, with many veterans engaging in ad libitum VR sessions in addition to group therapy sessions programmed as standard of care. These promising results echo the feasibility of VR for SUD treatment in previous cue-exposure interventions with VR, and demonstrate the feasibility of VR-based SUD psychotherapy delivery in a controlled residential environment. Future work will explore feasibility of VR-based psychotherapy in other SUD care settings and, from there, assess its effectiveness in randomized clinical trials.
Keywords
Feasibility study; Integrative therapy; Substance use disorder; Treatment outcome; Veterans; Virtual reality
Introduction
Substance Use Disorders (SUDs) are becoming an increasing concern to the Department of Veterans Affairs (VA) and the Department of Defense (DoD) due to their pervasiveness among veterans [1,2] and their detrimental effects and costliness [1,3]. For example, due to frequent deployment-related comorbidities such as Post-Traumatic Stress Disorder (PTSD) and Traumatic Brain Injury (TBI), SUD frequently has a more severe presentation and resistance to treatment in veterans [4-6]. A nationwide analysis using data collected from the National Survey on Drug Use and Health found that veterans are more likely than those in the general population to have a substance abuse disorder. Despite the VA offering comprehensive SUD care [7], many veterans do not seek or receive SUD treatment [8]. Treatment for SUD in the private and public sector frequently do not provide the best treatments, and the notion of what constitutes the best treatment is not always clear in some settings. A study of evidence-based SUD treatment programs found that of the available SUD treatment programs outside of the VA, most programs are not evidence-based treatments, and those that are evidence-based are typically not implemented how the treatments were designed [9].
To address the need for an effective, easily disseminated SUD treatment program, the evidence-informed Transcending Self Therapy: Four-Session Individual Integrative Cognitive Behavioral Treatment and Transcending Self Therapy: 20-Session Group Integrative Cognitive Behavioral Treatment (TST) was developed [10,11]. TST complies with a client-centered perspective, acknowledges the need for connecting with others, and for the patient to develop a passionate pursuit that aligns with their moral and spiritual beliefs [10]. TST has consistently improved treatment outcomes such as greater treatment adherence, increased abstinence, and decreased depression, while clients also demonstrated high levels of comprehension of fundamental therapy lessons [11,12]. Furthermore, a dissemination study of TST at three different VA Medical Centers (VAMC) found TST to be implemented effectively with high inter-provider fidelity, where providers were consistently satisfied with TST results [10].
Virtual Reality (VR) is a computer-generated environment with scenes and objects that appear real, immersing the user in their surroundings. This environment is viewed through a device known as a VR headset. VR headsets typically have screens in front of each eye and motion-tracking sensors to detect the user’s movements and adjust the display accordingly, creating a sense of presence and interaction with the virtual environment. VR has received notoriety in the past few years for its use in healthcare. Numerous studies have found VR effective in a healthcare setting for such areas as: improving phobias through exposure therapy, reducing stress and anxiety, and decreasing pain [13-15]. Indeed, the use of VR in SUD treatment has essentially been entirely for implementing cue exposure therapy (reviewed in [16,17]). To our knowledge, no previous VR intervention has used VR to present Cognitive Behavioral Therapy (CBT) psychoeducation or to offer a virtual space to complete therapeutic exercises such as CBT homework.
In light of technical advances, the possible advantages of using VR to support SUD treatment have become apparent. According to the 2021 U.S. Department of VA and U.S. DoD Clinical Practice Guideline, it was recommended to use technology/telehealth in addition to standard SUD treatment to manage patients remotely and effectively treat these disorders [18]. This need was further reinforced during the distancing requirements of the COVID-19 pandemic. However, the field of psychology would benefit from additional evidence supporting the clinical practice guideline panel recommending a technology/telehealth intervention for SUD, specifically the use of VR. Also, the panel found that extant technology-based interventions focused on Alcohol Use Disorder (AUD), not other SUDs [18]. Thus, highlighting a significant gap in transitioning evidence-based treatment into a technological platform.
Although AUD shares many genetic, environmental, and temperamental risk factors as other SUDs, persons with disordered use of harder drugs are frequently characterized by poorer executive function than AUD [19,20]. Moreover, as a component of their generally greater psychiatric severity, residential-treated individuals have been shown to have lower empirically-measured frustration tolerance than ambulatory care patients [21]. Therefore, it cannot be assumed that technical fluency or ad libitum engagement in technically-driven psychoeducational material would be feasible in a residential SUD treatment population with other comorbid SUD besides or in addition to AUD. The present study examined the feasibility of expanding TST into a virtual reality environment (TST-VR) for veterans in the residential Substance Abuse Treatment Program (SATP) at the local VAMC. We sought to determine 1) providers’ impressions of TST-VR effectiveness for patient treatment outcomes; 2) whether veterans found TST-VR easy to use; 3) whether veterans found TST-VR experiences were helpful to their recovery.
Methods
All recruitment and experimental methods herein were reviewed and approved by the Institutional Review Board (IRB) of the Richmond Veterans Affairs Medical Center.
- Prototype and program development
TST-VR was initially developed based on clinical study designs that utilized the principles of a human-centered design approach Birckhead et al., [22] to improve the development and evaluation of VR treatments. The first phase of this suggested framework is developing VR content based on patient and provider end-user input [22]. This study was primarily a feasibility study following the suggested framework established by Birckhead et al., [22], focusing on provider and patient feedback as a preliminary step to determining if TST in a VR setting is feasible and valuable for learning treatment skills. The study began as a single-session prototype used for feedback sessions from providers and patients. This version led to the development of a four-session TST-VR experience. This full four-session program was initially tested in 15 veterans and was perceived by the veterans to have a difficult start-up procedure and interface. The software (see below) was then upgraded to smooth out the user experience. The following data pertain to the experiences and ratings of subsequent veterans. Finally, amid the feasibility data collection herein, the TST content itself was expanded into ten sessions based on feedback from providers and patients who expressed desire for increased content.
- Participants
Veterans (N= 37) were recruited from patients newly admitted to the 28-day residential SATP at a VAMC in the Mid-Atlantic region. The inclusion criteria were admission to SATP and English-speaking. The exclusion criteria included legal blindness and a history of seizures. Participants were recruited by research personnel, who briefly described the TST-VR intervention to all newly admitted SATP patients, typically on a weekly basis. Interested participants were assessed for eligibility. Following informed consent, each participant was issued a passcode-protected TST-VR headset for the duration of their stay at SATP. They then underwent individual or group training in VR launch and navigation by the research staff person. From there, participants were able to use the VR set as often as desired outside of regular therapeutic activities.
During the final week of their stay, headsets were collected, and participants completed a brief self-report questionnaire of their impression of the headset in several aspects, using a Likert scale of 1 to 7 for each question (e.g., Extremely difficult to Effortless; Very uncomfortable to Comfortable). One question was reverse-coded to ensure consistent participant responses (e.g., “How bothersome were the VR activities?”). This questionnaire was administered within three days before discharge to maximize the chance that each participant would have engaged in multiple TST-VR activities (from which to form an impression). For participants who left treatment prematurely, against medical advice, or did not complete the questionnaire at the time of discharge for other reasons, research staff attempted to reach the veteran by phone after discharge to complete the questionnaire items in an interview format.
In addition to participant self-report, providers of the SATP who had at least one patient participating in TST-VR were invited to complete an anonymous electronic survey (written informed consent was not collected from providers) on which to rate their impressions of its benefit to patient engagement in different facets of psychoeducation and behavior change (five-point scales).
- TST-VR headset intervention
- Hardware
The Pico Neo 3 Pro VR headset and hand control sets were chosen for cost/performance balance, durability, and ease of use in setting up a “kiosk mode” where users can put on the headset and instantly be taken to the TST-VR program. The Pico headset also comes with a standard facial interface that is currently easier to clean than commercially available headsets in the same price range. A Cleanbox CV1 system was used to facilitate UV sanitation of the headsets. Custom cases were selected to contain each headset with a highly rugged exterior to protect the headsets from potential damage while in the patient’s care.
- Therapeutic content
TST-VR is built upon the Lighthouse XR Retreat Software Platform and centers on a scenic virtual therapeutic “retreat” nature landscape. Virtual stations a patient can navigate include multiple VR instructional videos with a virtual presenter explicitly created to explain several key concepts of TST (Figures 1 and 2). The program also enables the patient to navigate teleport to meditation and psychoeducational videos for participants to further engage in these essential SUD recovery skills. Participants would alternate between moving around a virtual world based around a cabin on a lake and, based on cues, select two to five VR videos per session that pertain to the skills and lessons being taught in the residential unit’s primary TST group therapy treatment program. A vital aspect of The Retreat Platform is that it is designed to be “self-contained” and can be experienced without an internet connection. Although the software does support “standing” modes, it was decided to design the content and virtual ambulation specifically for a seated experience for safety and logistical reasons.
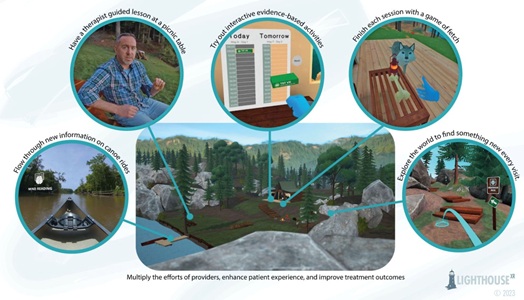 Figure 1: Images of the TST-VR treatment activities within the Retreat Platform.
Figure 1: Images of the TST-VR treatment activities within the Retreat Platform.
 Figure 2: Images of the Retreat Platform virtual world.
Figure 2: Images of the Retreat Platform virtual world.
- Data analytic plan
Although this is a qualitative and descriptive feasibility study, we nevertheless calculated and presented the level of patient engagement and enjoyment based on mean participant self-report questionnaire responses.
Results
The completed feasibility study sample consisted of 37 adults admitted to SATP (mean age 52.3 years; 95% male; 5% female; Table 1). In addition, 23 veterans signed consent to participate in the study and were issued headsets but did not complete the exit questionnaire. Therefore, the results presented herein were derived from those participants from whom self-report questionnaires (completed by participants the week of discharge from SATP) were completed on paper or by phone.
|
Characteristic |
N (%) |
|
Sex |
|
|
Male |
35 (94.6) |
|
Female |
2 (5.4) |
|
Race |
|
|
Caucasian |
20 (54.1) |
|
African American |
16 (43.2) |
|
Latino |
1 (2.7) |
Table 1: Demographic characteristics of study sample (N=37).
Participants rated the VR headset favorably concerning ease of use and comfortability (Table 2). The overall visual appearance of TST-VR activities and scenes were also rated high, with an average rating of 6.27. Only one participant stated that the TST-VR “made them dizzy,” and two stated that the joystick did not respond naturally or efficiently to their movements (Supplementary Table 1). Regarding how bothersome participants found using TST-VR to be, the overall average rating was low, meaning most participants found TST-VR easy to use (average item rating= 2.00; Table 2). Participants also rated the TST-VR activities favorably for how helpful they were to their recovery efforts and how helpful they were to understand the TST material. Two participants said they thought they would enjoy TST-VR better if they were incorporated into their group sessions for greater personal interactions (Supplementary Table 1). However, participants rated highly their willingness to complete VR activities (Table 2).
|
Question |
Question Category |
Average Participant Ratings (1-7) |
|
How easy was it to use the VR headset, such as to turn it on, to physically adjust it, and to navigate and find your way to virtual therapy sessions or other spaces after the first couple times you used it? |
Headset |
5.86 |
|
Overall, how physically comfortable was the VR helmet on your head? |
Headset |
6.08 |
|
How visually appealing were the VR activities and scenes? |
Headset |
6.27 |
|
How bothersome were the VR activities? |
Headset |
2.00 |
|
How important or useful were the VR activities to your recovery? |
Treatment |
5.35 |
|
How helpful were the VR activities in understanding TST (blue book group with Dr. J) material? |
Treatment |
5.51 |
|
Weighing these pros and cons, how willing were you to complete the VR activities? |
Treatment |
6.08 |
|
How much did the VR activities help you in your recovery? |
Treatment |
4.78 |
|
How likely are you to recommend the VR activities to other individuals working towards recovery? |
Continuing Use |
6.41 |
|
How much would you like to continue using VR activities as part of your ongoing recovery efforts? |
Continuing Use |
5.76 |
|
Would you choose an addiction treatment program with VR activities versus the same program without VR activities? |
Continuing Use |
|
|
It doesn’t matter |
6 (16.2%) |
|
|
Yes |
31 (83.8%) |
|
|
No |
0 |
Table 2: Patient feedback from exit questionnaires.
Note. Patient feedback questions with what category they fall under (e.g., questions in regard to the headset, their treatment, or continuing VR use/recommendation) and the average ratings for each question.
The overwhelming majority (83.8%) of participants who completed the protocol would choose an addiction treatment program that included VR activities, while 16.2% expressed indifference to the availability of VR. No patients indicated that they would prefer a treatment program without TST-VR. Finally, participants rated a high likelihood to recommend TST-VR to other individuals working towards recovery and wanting to continue using TST-VR in their ongoing recovery efforts (Table 2). In a complementary assessment, providers (N=31 anonymous survey respondents) also reported that the TST-VR activities were beneficial for their patient’s treatment progress and rated highly the overall ability to incorporate TST-VR into their clients’ treatment (Table 3). The providers’ motivation to include TST-VR in their treatment practices was also rated high, as well as the belief that TST-VR would be helpful and a valuable tool in promoting recovery. Providers rated TST-VR highly for improving the quality of their patients’ therapy and for readily adopting TST-VR into treatment programs. Providers stated that TST-VR has the “ability to engage patients differently and that the immersion and interaction could increase engagement” (Supplementary Table 2). Providers’ rated highly their belief that the VAMC organization would benefit from including TST-VR and their belief that other treatment programs should have the option for TST-VR.
|
Question |
Question Category |
Average Provider Ratings (1-5) |
|
I would recommend TST VR to my clients. |
Recommendation |
4.87 (0.34) |
|
I would like to have TST VR as an option for my |
Recommendation |
4.90 (0.31) |
|
I am motivated to include TST VR as part of |
Motivation/Belief |
4.90 (0.31) |
|
I believe TST VR will be helpful and useful in |
Motivation/Belief |
4.97 (0.19) |
|
I believe my organization/program may benefit on |
Treatment/Organization |
4.93 (0.25) |
|
TST VR will improve the quality of the therapy I |
Treatment/Organization |
4.72 (0.53) |
|
TST VR can be readily adopted into treatment |
Treatment/Organization |
4.74 (0.44) |
|
I think other treatment programs should have the option |
Treatment/Organization |
4.90 (0.40) |
Table 3: Provider feedback on a Likert-scale.
Note. Averages of provider feedback responses on a Likert-scale from 1-5, separated into categories (e.g., recommendation, motivation/belief, treatment/organization).
Discussion
Essentially all previously published interventions for SUD using VR have been variants of cue exposure or craving induction therapy (reviewed in [16,17]), wherein the patient is exposed to substance cues in the virtual environment but cannot consume the substance and, in some applications, can engage in gamified alternative behavior (like crushing cigarettes) [23]. This ostensibly leads to replacement learning with de-coupling of cue and outcome. In contrast, to our knowledge, this is the first study of using VR to deliver an effective cognitive behavioral therapy to help treat SUD. This feasibility study was conducted to obtain critical provider and patient feedback about the prospects for integrating TST-VR into SATP. The results demonstrate that TST-VR is viewed positively by most providers and patients as a potential avenue for bolstering treatment efforts. A majority of patients and provider survey respondents would recommend other patients to use TST-VR to support their ongoing recovery efforts, and patients had a high average rating of wanting to continue to use TST-VR to support their recovery (average item rating= 5.74 on a scale of 1 to 7).
Previous studies investigating the barriers and challenges to integrating VR into treatment settings have either not probed or have disregarded provider feedback in developing VR applications, limiting its clinical usefulness [24]. In the current study, we sought provider feedback early in the development and implementation process to avoid such barriers (in accordance with the human-centered approach guidelines). Overall, providers’ ratings were overwhelmingly positive regarding the impact TST-VR could provide on their patient's treatment quality (Table 3) and the ease with which TST-VR could be integrated into their treatment programs. Providers stated that the VR experience’s “peaceful scenes could calm veterans with PTSD,” could “engage patients so they spend more time in therapy,” while providing the “ability to engage patients differently,” and would allow for “consistency in providing therapy and novelty for patients” (Supplementary Table 2). Furthermore, providers rated a strong desire to have TST-VR as a treatment option and believed that the Veterans Health Administration could benefit from utilizing the technology. These novel findings demonstrate the providers’ willingness and want to integrate TST-VR into their treatment programs and beliefs that it could improve their patients’ recovery efforts.
Numerous VR studies have stated that a major barrier to accessibility is the comfort participants feel while wearing the headsets and the ease of learning and working with the technology [25,26]. Thus, we focused initial efforts on ensuring that this potential hurdle was abated. Based on exit questionnaire responses at discharge, participants reported no major usability issues and that the headsets were comfortable. Updates to the program were occasionally phased in as software or hardware issues were identified. While minor technological issues were identified early in this feasibility study, participants still rated the overall usability high. Several studies have noted the importance of visually appealing VR environments to increase user experience, thus highlighting a key strength in the current TST-VR user experience [25,27]. In light of participant ratings indicating that they found the graphics visually appealing in the TST-VR activities (Table 2), it seems likely that appealing graphics contributed to the high ratings of engagement and utility. Furthermore, participants had an average age of 52.3, with a potential age-cohort barrier to using the VR technology; however, no such barriers were identified, highlighting a key strength for disseminating TST-VR.
Most importantly, the impact of TST-VR on the participants’ recovery efforts was rated at an average of 5.21 (on a scale of 1 to 7), indicating that most found it helpful to their recovery efforts. One participant stated that TST-VR helped to reinforce their cognitive-behavioral therapy (TST) classroom work as part of SATP and their meditation skills (Supplementary Table 1). Our participants’ perceptions of VR's utility align with findings in other VR studies that have also found VR helpful for a patient's recovery efforts. A systematic review by Taubin et al., [17] found that most studies evaluating VR as a tool for treating SUDs effectively reduced participant’s use of substances and cravings. They also found some positive results for VR improving the patient’s anxiety and emotional regulation [17]. Worley [28] found that SUD treatment-seeking patients using VR not only learned to manage their substance cravings but that VR psychoeducation and other experiences reduced anxiety and stress, conveyed life skills, and increased their exercise efforts [28]. These novel findings demonstrate that using VR in treatment settings could improve the patient’s well-being above and beyond substance use outcomes.
We caution that there are several limitations of this feasibility study. Due to staff scheduling limitations, some participants were not provided a headset until one to two weeks into their treatment. As a result of this delay, many participants may not have had an opportunity to fully incorporate the TST-VR into their daily schedules at SATP as they had already established a routine and needed more unstructured time available to engage the VR program. One participant stated that they needed more time to explore the virtual environment in its entirety, limiting their enjoyment (Supplementary Table 1). Secondly, our present sample was limited to only veterans in a residential treatment center, limiting the ability to generalize these results to other populations. Relatedly, our sample size was relatively small due to the small residential treatment program available and the limited number of headsets. Future studies of VR-TST engagement and feasibility in other treatment populations (with a larger sample size) would be beneficial.
Because our analyses are based on patient feedback on the treatment exit questionnaire, it is important to note that many consented participants did not complete their questionnaire, either on paper or by telephone after discharge. We believe the demands and stressors of discharging could have interfered with participants’ motivation to complete the exit questionnaires (e.g., participants may not have viewed completing the questionnaires as valuable, participants could have been overwhelmed with the prospect of leaving the SATP environment, and there are numerous competing tasks on the day of discharge). Furthermore, as this was a feasibility study, no compensation was provided for completing study procedures, which could have limited the participant’s motivation. It is possible that some participants who did not complete the anonymous questionnaire may have declined due to ambivalence about the TST-VR program or a perception that it was not helpful. This hypothesis would require future research.
Conclusion and Future Directions
As stated previously, this study was created following the suggested framework established by Birckhead et al., [22], focusing on continuous provider and patient feedback and iterative prototyping based on this feedback. During the study, we began the refinement process in the 10-session TST-VR based on feedback from the 4-session TST-VR, and the 4-session was based on a 1-session prototype. The study team intends to continue refining and expanding study procedures based on the feedback received thus far. We will also investigate the length of time that participants spent interacting with the TST-VR experience over time, what virtual activities participants tend to visit among their palette of options, and how their virtual activities relate to their treatment outcomes, as done in similar VR studies [29,30].
We caution that this was primarily a descriptive feasibility study, not a randomized controlled clinical trial that would provide evidence sufficient for approval for SUD treatment by the US Food and Drug Administration or other regulatory agencies and professional bodies as an evidence-based treatment. Based on the high ratings of tolerability and potential utility of the majority of consented participants, the next step may be a controlled clinical trial of TST-VR, such as with a comparison arm with alternative VR content [22,31] or treatment as usual.
In conclusion, this initial feasibility study demonstrates the usefulness and the demand for this technology in treatment settings by providers and patients. These initial findings clearly indicate that patients are willing to engage in TST-VR in conjunction with their regular treatment and find it a good opportunity for other patients to engage with them during their treatment. These findings also indicate the accessibility of TST-VR in a wide range of patients (e.g., age, race, sex). Although this initial study was interested in the provider and patient feedback, evaluating how the participant’s headset use and time in headsets relate to their treatment outcomes is a necessary avenue of research to expand on these initial findings.
Declaration of Conflicting Interests
James M. Bjork and Angela J. Zaur declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Jarrod Reisweber has the potential to receive future royalties regarding Transcending Self Therapy. Mark Lambert, as a co-founder of Lighthouse XR, which has licensed Transcending Self Therapy for XR use, acknowledges a financial interest in the success of TST-VR.
Grant Information
This work was supported by the VHA Innovation Network and VCU Office of Research and Innovation.
Acknowledgment
Anne Bailey, Stephanie Bertucci, Mary Bradshaw, Monica Bridgeforth-Merrick, Patricia Curry, Dale Dejarnette, Brent Fagg, Ronald Johnson, Gina Lambert, David Lekberg, Susan Molano, Sara Patterson, Caitlin Rawlins, and Megan Welu.
References
- Lan CW, Fiellin DA, Barry DT, Bryant KJ, Gordon AJ, et al. (2016) The epidemiology of substance use disorders in US Veterans: A systematic review and analysis of assessment methods. Am J Addict 25: 7-24.
- Teeters JB, Lancaster CL, Brown DG, Back SE (2017) Substance use disorders in military veterans: Prevalence and treatment challenges. Subst Abuse Rehabil 8: 69-77.
- Hawkins EJ, Grossbard J, Benbow J, Nacev V, Kivlahan DR (2012) Evidence-Based Screening, Diagnosis, and Treatment of Substance Use Disorders Among Veterans and Military Service Personnel. Mil Med 177: 29-38.
- Boden MT, Hoggatt KJ (2018) Substance Use Disorders Among Veterans in a Nationally Representative Sample: Prevalence and Associated Functioning and Treatment Utilization. J Stud Alcohol Drugs 79: 853-861.
- Caldwell TM, Rodgers B, Jorm AF, Christensen H, Jacomb PA, et al. (2002) Patterns of association between alcohol consumption and symptoms of depression and anxiety in young adults. Addiction 97: 583-594.
- Holahan CJ, Schutte KK, Brennan PL, Holahan CK, Moos RH (2014) Episodic Heavy Drinking and 20-Year Total Mortality Among Late-Life Moderate Drinkers. Alcohol Clin Exp Res 38: 1432-1438.
- DeMarce JM, Gnys M, Raffa SD, Kumpula M, Karlin BE (2021) Dissemination of Cognitive Behavioral Therapy for Substance Use Disorders in the Department of Veterans Affairs Health Care System: Description and Evaluation of Veteran Outcomes. Subst Abus 42: 168-174.
- Golub A, Vazan P, Bennett AS, Liberty HJ (2013) Unmet Need for Treatment of Substance Use Disorders and Serious Psychological Distress Among Veterans: A Nationwide Analysis Using the NSDUH. Mil Med 178: 107-114.
- Lundgren L, Amodeo M, Cohen A, Chassler D, Horowitz A (2011) Modifications of evidence-based practices in community-based addiction treatment organizations: A qualitative research study. Addict Behav 36: 630-635.
- Polak K, Reisweber J, Bjork JM (2021) Multi-Site Dissemination of Four-Session Individual Transcending Self Therapy: An Integrative Cognitive-Behavioral Therapy for Substance Use Disorders. J Addict Addict Disord 8: 1-10.
- Reisweber J, Polak K, Domm D (2020) Transcending Self Therapy. Transcending Self Therapy: Four-Session Individual Integrative Cognitive Behavioral Treatment. Book for Facilitators.
- Polak K, Reisweber J (2019) Transcending Self Therapy: Four-Session Individual Integrative Cognitive Behavioral Treatment. Book for Clients.
- Aziz H (2018) Virtual Reality Programs Applications in Healthcare. J Health Med Inform 9: 305.
- Guazzaroni G, Pillai AS, Mathew PS (2019) Impact of Virtual Reality in Healthcare: A Review. In: Guazzaroni G, Pillai AS, Mathew PS (eds.). Virtual and Augmented Reality in Mental Health Treatment. IGI Globalp, Pennsylvania, USA.
- Snoswell AJ, Snoswell CL (2019) Immersive Virtual Reality in Health Care: Systematic Review of Technology and Disease States. JMIR Biomed Eng 4: 15025.
- Segawa T, Baudry T, Bourla A, Blanc JV, Peretti CS, et al. (2019) Virtual Reality (VR) in Assessment and Treatment of Addictive Disorders: A Systematic Review. Front Neurosci 13: 1409.
- Taubin D, Berger A, Greenwald D, Greenwald H, Burke C, et al. (2023) A systematic review of virtual reality therapies for substance use disorders: Impact on secondary treatment outcomes. Am J Addict 32: 13-23.
- Perry C, Liberto J, Milliken C, Burden J, Hagedorn H, et al. (2022) The Management of Substance Use Disorders: Synopsis of the 2021 U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guideline. Ann Intern Med 175: 720-731.
- Fernández-Serrano MJ, Pérez-García M, Perales JC, Verdejo-García A (2010) Prevalence of executive dysfunction in cocaine, heroin and alcohol users enrolled in therapeutic communities. Eur J Pharmacol 626: 104-112.
- van der Plas EA, Crone EA, van den Wildenberg WP, Tranel D, Bechara A (2009) Executive control deficits in substance-dependent individuals: A comparison of alcohol, cocaine, and methamphetamine and of men and women. J Clin Exp Neuropsychol 31: 706-719.
- Ramirez-Castillo D, Garcia-Roda C, Guell F, Fernandez-Montalvo J, Bernacer J, et al. (2019) Frustration Tolerance and Personality Traits in Patients With Substance Use Disorders. Front Psychiatry 10: 421.
- Birckhead B, Khalil C, Liu X, Conovitz S, Rizzo A, et al. (2019) Recommendations for Methodology of Virtual Reality Clinical Trials in Health Care by an International Working Group: Iterative Study. JMIR Ment Health 6: 11973.
- Pericot-Valverde I, Secades-Villa R, Gutiérrez-Maldonado J (2019) A randomized clinical trial of cue exposure treatment through virtual reality for smoking cessation. J Subst Abuse Treat 96: 26-32.
- Halbig A, Babu SK, Gatter S, Latoschik ME, Brukamp K, et al. (2022) Opportunities and Challenges of Virtual Reality in Healthcare – A Domain Experts Inquiry. Front Virtual Real 3.
- Motraghi TE, Seim RW, Meyer EC, Morissette SB (2014) Virtual Reality Exposure Therapy for the Treatment of Posttraumatic Stress Disorder: A Methodological Review Using CONSORT Guidelines. J Clin Psychol 70: 197-208.
- Wray TB, Emery NN (2022) Feasibility, Appropriateness, and Willingness to Use Virtual Reality as an Adjunct to Counseling among Addictions Counselors. Subst Use Misuse 57: 1470-1477.
- Shen YI, Nelson AJ, Oberlin BG (2022) Virtual reality intervention effects on future self-continuity and delayed reward preference in substance use disorder recovery: Pilot study results. Discov Ment Health 2: 19.
- Worley J (2019) Virtual Reality for Individuals With Substance Use Disorders. J Psychosoc Nurs Ment Health Serv 57: 15-19.
- Paul M, Bullock K, Bailenson J (2020) Virtual Reality Behavioral Activation as an Intervention for Major Depressive Disorder: Case Report. JMIR Ment Health 7: 24331.
- Paul M, Bullock K, Bailenson J (2022) Virtual Reality Behavioral Activation for Adults With Major Depressive Disorder: Feasibility Randomized Controlled Trial. JMIR Ment Health 9: 35526.
- Rizzo A, Koenig S, Lange B (2023) Clinical virtual reality: The state of the science. In: Rizzo A, Koenig S, Lange B (eds.). APA handbook of neuropsychology. American Psychological Associationp, Washington, DC, USA.
Supplementary Table
|
What do you like about the VR activities? (free response) |
What do you dislike about the VR activities? (free response) |
|
Some of the activities were very immersive and he got a lot out of it but thinks graphics could be better. |
Pace of introduction too slow. Suggested an option if they'd done VR at the beginning and can have faster/slower introduction. |
|
Easy to understand. |
Didn't have enough time to really explore. |
|
Very calming and lifelike. |
Confusing to figure out controls, participant felt aggravated and discontinued part way through the tutorial. |
|
Great to have during leisure time. |
Would have enjoyed VR more if it was incorporated into group. |
|
It was good. Enjoyed it. |
I like to use it during my free time, but sometimes the handhelds did not work. |
|
It helps to reinforce the CBT classroom work and meditation. |
Did not get to use headset much because it did not work properly. |
|
I liked the being able to talk with Dr. J virtually. I liked the visuals. I also like the piers and the landscape work. |
The joystick did not respond to natural hand movements, and it moved too fast sometimes. |
|
N/A |
It made me dizzy. |
|
N/A |
Not enough personal interaction |
|
N/A |
At first, the turning it on was a bit of a learning curve. I had to figure out how to turn it on and get it started. |
Supplementary Table 1: Qualitative responses from patients.
|
What parts of TST VR seem helpful? Why? [free response] |
What do you see as the biggest challenges/barriers in using TST VR? How could this challenge (or these challenges) be overcome? [free response] |
What do you think needs to happen to make TST VR successfully adopted at the VA? [free response] |
What other resources/support would be helpful/needed for TST VR implementation? [free response] |
What improvements could be made to TST VR? [free response] |
How would you like to incorporate TST VR into treatment with your patients? [free response] |
What other feedback do you have? [free response] |
|
Additional perspective, memory retention. |
Financial - buying headsets. |
Promoting widely. |
N/A |
N/A |
N/A |
Great program! |
|
Meditation rock. |
Those who afraid or unsure about technology, older generation. |
Have a crowd for scenario, scavenger hunt through a store. |
Add crowd noise. |
None at this time. |
Working with a patient towards goals. |
None at this time. |
|
Voice, very thoughtful observations. |
Eye diseases. |
Advertising. |
Education. |
Strap around chin if possible. |
N/A |
Great work! |
|
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
N/A |
|
Setting the patient in a natural, relaxing environment from the beginning is ideal. |
Eyestrain or headaches? Headsets that can be adjusted to eye width? |
N/A |
N/A |
N/A |
A session and a debrief to answer questions, etc. |
It’s really cool! |
|
Interactive message will help veterans learn and adopt strategies. |
None |
It will be a great addition to the program and ways to get to them in effective manner. |
N/A |
N/A |
Allow outpatients to visit the TST-VR lab and have content in a library for them to choose what they need. |
N/A |
|
It removes distractions, controls the environment and provides comfort. |
Technology, headset comfort and resolution, cost, expanding development. |
Show the benefit, get testimonials, set up VR centers. |
IT support - integrate events/findings into the ER/Med record. |
Graphics, headset resolution. |
N/A |
Amazing tool - very innovative and exciting! |
|
I enjoyed the meditation rock feature and that it can be used regardless of the level the "player" is. |
Maintenance of the equipment, storage space and for those with eyeglasses using the headset. |
Leadership support of obtaining and approving its usage of TST VR. |
Having important resources/supports listed as an option to be connected to them. |
I'd like to have a VR experience where there's more movement (walking, reaching, etc). |
N/A |
Please continue exploring alternative features like this for the veteran populations. |
|
Peaceful scenes calm veterans with PTSD. |
Veterans who are uncomfortable with tech. |
N/A |
Explanation and focus groups, free demo. |
Cartoon portion more realistic. |
Individual sessions. |
Grove - waterfalls; palm trees, stone benches, stone walkway. |
|
Visualization, being in an environment that promotes recovery. |
User knowledge and electronics. |
Pilot with veterans. |
N/A |
Appreciate the early phases of the imagery. Look forward to seeing the enhancements. |
N/A |
N/A |
|
Reinforces paper materials/ in class instruction/ seeing therapist/ real people/ included talking to you. |
Some veterans are elderly or have cognitive delays that may make using technology difficult. |
The number of units available - follow up with a real-life therapist. |
N/A |
The real-life scenes/beaches are more enjoyable than the cartoon/video game type scenes. |
N/A |
N/A |
|
The idea of engaging patients so they spend more time in the therapy. |
Adoption and continual use of the technology. |
Clinic support and funding. |
Tech support. |
Not sure. |
Useful for PTSD patients. |
Reduce the wobble on canoe for those with motion sickness. |
|
Being able to choose where you want to go and make your own schedule. |
Some people may feel claustrophobic at first |
More sessions where providers and patients try it out. |
N/A |
Make some improvements to the graphics - add places to sit. More visual aesthetics. |
N/A |
N/A |
|
All! Personal choice in where patient wants to go and freedom to choose. |
Biggest challenge would be if a person presents multiple times for treatment. |
Jarrod is doing it! |
Full service/ facility support. |
More than a retreat. Offering different retreats for different levels? |
If available, I would like access to TST VR for my patients. |
You guys did a great job! |
|
I liked the area (water, cabin, rocks, etc.). It was peaceful and provided a therapeutic environment. |
It might hurt the dead or eyes to wear the headset too long. Some pts may still prefer in person treatment. Offering both options would be helpful. |
Leadership support and lots of grant money. |
Space for the equipment. |
The words were sometimes blurry or a bit hard to read. |
I think it could be helpful for some of my patients with substance use issues. |
Dr. Reisweber& the female voice guided very well and looked great. |
|
The freedom to schedule and engage as you would like. |
Clients feeling disorientation / not willing to invest. |
Provide space for patients to use the system free of outside noise. |
Soundproof areas. |
When moving, have a 'slider' instead of 'jumping' to next spot. |
Virtual sessions. |
Include fishing and a trophy wall. |
|
Consistency in providing therapy and novelty for patients. |
Access for patients. |
Making it widely available. |
N/A |
N/A |
Being able to refer patients on an outpatient basis. |
Great job! |
|
Meditation exercise, explanation of TST by Dr. Reisweber. |
Technical difficulties. Some maybe hesitant to try technology. Having a tech assistant that is easily available. |
Financial support. |
Full support from executive leadership and all disciplines. |
Ensure appropriate fit for clarity and full immersion. |
Helps to increase engagement, which improves patient's response to treatment, outpatient settings, other areas of facility, possible areas to encourage participation. |
Could be adopted for numerous applications, including assisting staff with decreasing anxiety. |
|
Ability to engage patients in a different way - hopeful immersion and interaction can increase engagement. |
Time, logistics, some patient hospitalizations. |
Clear process for accessibility and references. |
Having a contact that veterans can reach out to if they have questions. |
Less blurry. Headset is heavy. |
Yes please - if and when possible! |
N/A |
|
The use of nature/natural scenes; the novelty of using VR as a new approach; including visual experiences vs. just speaking. |
Learning curve for vets who have limited experience with technology; maybe brief training sessions & introductions like today could help. |
Make it adaptable to multiple programs. |
N/A |
The weight of the device is a bit heavy on your face. |
To support the development of mindfulness techniques like deep breathing. |
N/A |
Supplementary Table 2: Qualitative responses from providers.
Citation: Zaur AJ, Reisweber J, Lambert M, Bjork JM (2023) Feasibility of Virtual Reality-Delivered Transcending Self Therapy in Veterans Undergoing Residential Substance Use Treatment. J Addict Addictv Disord 10: 131.
Copyright: © 2023 Zaur AJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

