Ganglion of the Foot and Ankle Imaging and Pathological Findings, Differential Diagnosis, and Operative Management
*Corresponding Author(s):
Emrah SayitDepartment Of Orthopedics And Traumatology, Samsun Education And Research Hospital, Samsun, Turkey
Tel:+90 5056708662,
Email:dremrahsayit@gmail.com
Abstract
Ganglion cysts are the most common benign soft-tissue tumors in the foot and ankle. They are often asymptomatic but can cause discomfort and pain. If they compress the adjacent nerve fascicles, they can cause pain, paresthesias, weakness, muscle denervation, and atrophy. Diagnosis is usually made clinically. Imaging methods such as ultrasound and Magnetic Resonance imaging are also very helpful in making a diagnosis. Treatment is usually conservative. Ganglion cysts can be removed by surgical excision, but surgeons must be careful as these types of cysts are very close to the nerves. The aim in this article is to discuss imaging findings, differential diagnosis, and treatment approaches relating to ganglion cysts in the foot and ankle.
Keywords
INTRODUCTION
There are many ways of classifying ganglion cysts such as using the relation of structure. The cysts those within the bone are called as intraosseous ganglion cysts, those adjacent to bone called as periosteal ganglion cysts, and those away from bone called as soft tissue ganglion cysts. The cysts those within the joint are called as intra-articular ganglion cysts and those adjacent to a joint called as juxta-articular ganglion cysts [6].
Intraosseous ganglion cysts are benign and often multiloculated lesions located in the subchondral bone [4]. They occur in the mature skeletons of patients and are often seen in the femoral head and the tibia [4]. They are mostly seen at the 4 and 5 decade, and rare at children. The exact pathogenesis of ganglion cysts is still unclear, but they are thought to be the result of acute or repetitive trauma. Most researchers [5,7,8] believe ganglion cysts are due to the myxoid degeneration of surrounding connective tissue, such as the joint capsule or tendon sheath.
The aim in this article is to discuss the imaging findings, differential diagnosis, and treatment approaches relating to ganglion cysts in the foot and ankle.
CLINICAL FINDINGS
Physical examination can reveal swelling with tenderness. Upon palpation, a cyst can be soft or firm or movable or fixed. A visible lesion is covered with normal skin, which is not red or warm (Figure 1) [4].

Figure 1: Swelling around the lateral malleolus.
PATHOLOGICAL FINDINGS

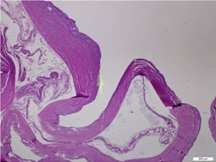
The wall of the ganglion is composed of randomly oriented sheets of collagen arranged in loose layers, one on top of another, and can be shown with electron microscopy. Rare cells are present in the collagen sheets and appear to be fully functional fibroblasts or mesenchymal cells. As no synovial lining exists in these structures, they cannot be classified as true cysts [10]. Although there are focal areas of mucinous degeneration in the cyst wall, significant global degenerative changes, necrosis, or inflammatory changes within the pseudocyst or surrounding tissues have not been demonstrated [10].
IMAGING FINDINGS
Ultrasound (US) and Magnetic Resonance Imaging (MRI) can differentiate a ganglion cyst from other soft-tissue tumors and tumor-like lesions [2]. US reveals an oval, uniloculated or multiloculated anechoic lesion that had an posterior acoustic enhancement. If the cysts are complicated by chronic inflammation, infection or hemorrhage, they may have partial or complete hyperechogenic component [12]. However, US is not as good as MRI in showing deeper tissues. Besides, it cannot clearly shows the relationship of the lesions with joints and tendon sheaths.
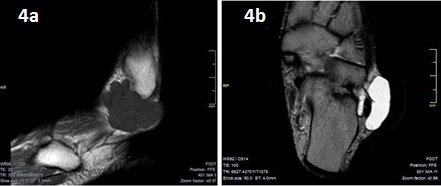
The indications of the MRI are uncertain diagnosis, tarsal tunnel ganglion, planning of the optimal location of the ganglion portal, posterior ankle or plantar ganglion, foot dorsum ganglion that covered the area of the intermetatarsal space and toe pulp ganglion. MRI is also useful in identifying the surrounding neurovascular structures of the lesion, the original site of the tarsal tunnel ganglion, and the relationship between the nerve and the ganglion in order to choose the most appropriate operative management [13]. MRI can also show any deep extension of the foot dorsum ganglion through the intermetatarsal space [14]. Ganglion cysts are shown to be well-defined and hypointense on T1-Weighted (W) images (Figure 4a) and hyperintense on T2-W images (Figure 4b) [9]. Contrast enhancement can reveal septation and cyst walls in post-contrast images [9]. Uncharacteristic signal behavior can be seen when hemorrhages and chronic inflammation develop [11]. Due to chronic inflammation or hemorrhage, the signal intensity increases at T1W images and decreases at T2W images. Besides, thickening and enhancement can be seen at the cyst wall [12].
DIFFERENTIAL DIAGNOSIS
Also, unicameral bone cysts, chondromyxoid fibroma, Brodie’s abscesses, giant cell tumor, fibrous dysplasia, aneurysmal bone cyst, chondroblastoma and Pigmented Villonodular Synovitis (PVNS) should be considered in the differential diagnosis of intraosseous ganglion cysts [4,16]. PVNS is a benign proliferative disorder of synovium. It affects joints, bursae and tendon sheath, and may be diffuse or localized. X-ray may be normal. However, in very advanced cases, the synovial proliferation can be seen as uncalcified radiodense mass. Also, bone erosion due to pressure and subchondral cysts are observed. PVNS is seen inhomogeneous signal intensity in MRI according to fat, collagen and hemosiderin it contains. It is frequently seen at hypointense signal intensity on T1 and T2W images, therefore, can be distinguished from the ganglion cyst by the signal intensity which have been shown in T2W images [1]. Giant Cell Tumor (GCT) of bone is well-defined and shows eccentric placement in bone [17]. It often shows close settlement to the articular surface. The epiphyses of the patients are closed. Fluid-fluid levels may be seen at aggressive lesions [17]. GCT of bone and aneurysmal bone cyst can be differentiated from intraosseous ganglion on X-ray by a lack of marginal osteosclerosis and thinning of the adjacent cortex due to expansion [16]. Chondroblastomas show epiphyseal settlement and differential diagnosis of intraosseous ganglion cyst from chondrosarcoma is difficult. At chondroblastoma, marginal osteosclerosis can be seen in X-ray. The differential diagnosis can only be done by lack of enhancement in intraosseous ganglion cyst with contrast enhanced MRI (Table 1) [16].
OPERATIVE MANAGEMENT
The primary treatment for symptomatic intraosseous ganglion cysts is surgical excision by curettage followed by bone grafting in order to prevent any recurrence and the risk of a collapsing fracture [4].
Arthroscopic removal of ganglion cyst is a less invasive procedure for intraosseous ganglia. Büchler reported no recurrences and excellent results after arthroscopic treatment. Another advantage of this technique is that the possibility of intervention in the chondral lesions [18].
Nerve damage during excision of the cyst causes major problems. Nerve damage during surgery can be prevented by using a bipolar coagulator and by magnification with a loop [2].
Excision of the tarsal tunnel ganglion is very difficult. Three postoperative tibial nerve injury cases have been reported in the literature [19]. Cutaneous nerve branches, such as the sural nerve and superficial peroneal nerve, are attached to the mass in about one third of cases, requiring meticulous dissection. However, sometimes nerve branches cannot be separated from the mass. In such cases, nerve branches have to be sacrificed after giving the necessary information to the patient [2].
CONCLUSION
REFERENCES
- Woertler K (2005) Soft tissue masses in the foot and ankle: characteristics on MR Imaging. Semin Musculoskelet Radiol 9: 227-242.
- Ahn JH, Choy WS, Kim HY (2010) Operative treatment for ganglion cysts of the foot and ankle. J Foot Ankle Surg 49: 442-445.
- Macdonald DJ, Holt G, Vass K, Marsh A, Kumar CS (2007) The differential diagnosis of foot lumps: 101 cases treated surgically in North Glasgow over 4 years. Ann R Coll Surg Engl 89: 272-275.
- Sedeek SM, Choudry Q, Garg S (2015) Intraosseous ganglion of the distal tibia: clinical, radiological, and operative management. Case Rep Orthop 2015: 759257.
- Angelides AC, Wallace PF (1976) The dorsal ganglion of the wrist: its pathogenesis, gross and microscopic anatomy, and surgical treatment. J Hand Surg Am 1: 228-235.
- Beaman FD, Peterson JJ (2007). MR imaging of cysts, ganglia, and bursae about the knee. Radiol Clin North Am 45: 969-982.
- Rozbruch SR, Chang V, Bohne WH, Deland JT (1988) Ganglion cysts of the lower extremity: an analysis of 54 cases and review of the literature. Orthopedics 21: 141-148.
- Wu KK (1993) Ganglions of the foot. J Foot Ankle Surg 32: 343-347.
- Nikolopoulos D, Safos G, Sergides N, Safos P (2015) Deep peroneal nerve palsy caused by an extraneural ganglion cyst: a rare case. Case Rep Orthop 2015: 861697.
- Loder RT, Robinson JH, Jackson WT, Allen DJ (1988). A surface ultrastructure study of ganglia and digital mucous cysts. J Hand Surg AM 13: 758-762.
- Weishaupt D, Treiber K, Kundert HP, Zollinger H, Vienne P, et al (2003) Morton neuroma: MR imaging in prone, supine, and upright weight-bearing body positions. Radiology 226: 849-856.
- Hul EV, Vanhoenacker F, Dyck PV, Schepper AD, Parizel PM (2011) Pseudotumoural soft tissue lesions of the foot and ankle: a pictorial review. Insights Imaging 2: 439-452.
- Lui TH (2014) Arthroscopic ganglionectomy of the foot and ankle. Knee Surg Sports Traumatol Arthrosc 22: 1693-1700.
- McEvedy BV (1962). Simple ganglia. Br J Surg 49: 585-594.
- Patel P, Schucany WG. A rare case of intraneural ganglion cyst involving the tibial nerve (2012). Proc (Bayl Univ Med Cent) 25: 132-135.
- Sakamoto A, Oda Y, Iwamoto Y (2013)Intraosseous Ganglia: A Series of 17 Treated Cases. Biomed Res Int 2013: 462730.
- Chakarun CJ, Forrester DM, Gottsegen CJ, Patel DB, White EA, et al. (2013). Giant cell tumor of bone: review, mimics, and new developments in treatment. Radiographics 33: 197-211.
- Büchler L, Hosalkar H, Weber M (2009) Arthroscopically Assisted Removal of Intraosseous Ganglion Cysts of the Distal Tibia. Clin Orthop Relat Res 467: 2925-2931.
- Rosson GD, Spinner RJ, Dellon AL (2005) Tarsal tunnel surgery for treatment of tarsal ganglion: a rewarding operation with devastating potential complications. J Am Podiatr Med Assoc 95: 459-463.
Citation: Sayit E, Sayit AT, Bakirtas M (2015) Ganglion of the Foot and Ankle: Imaging and Pathological Findings, Differential Diagnosis, and Operative Management. J Orthop Res Physiother 1: 005.
Copyright: © 2015 Emrah sayit, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

