
Hip Dislocation in Cerebral Palsy: Treatment Options
*Corresponding Author(s):
Eldessouky ASpr Trauma And Orthopaedics, Alexandra Hospital, Redditch, United Kingdom
Tel:+44 1215741676; +44 7462223365,
Email:amr_rbcs@yahoo.com
Abstract
Hip displacement in cerebral palsy is a common problem. The muscle imbalance and spasticity can lead to abnormal deforming forces which act on the hip joint resulting in acetabular dysplasia and femoral head migration. The patients suffer painful seating, abnormal gait and difficulty in personal hygiene.
There are various treatment options to address this problem depending on the patient’s age, GMFCS level and the degree of hip subluxation. Careful individual assessment is paramount in choosing the suitable treatment. The aim of this paper is to review the most common treatments of hip problems in cerebral palsy patients.
Keywords
INTRODUCTION
Hip instability and gait abnormalities are common hip problems in Cerebral palsy patients. Hip subluxation and dislocation develops in response to muscle imbalance and spasticity [2]. The patient’s problems vary from abnormal gait to painful seating and difficulty in personal hygiene. The goal of treatment in those patients is to provide a painless hip that allows stable sitting and positioning.
INCIDENCE
The reported incidence of hip displacement in children with cerebral palsy has ranged from 1% to 75% and has been linked with the severity of involvement and the ambulatory status. Incidence of hip displacement is low in patients with mild involvement and who can walk independently, whereas those with more severe involvement and who are unable to walk have the greatest risk of hip displacement [4]. The lowest incidence of hip displacement was found in the children with GMFCS level-I and the highest incidence, in those with level-V [5]. Per Larnet and colleagues analysed the risk of hip displacement in relation to age and gross motor function in a total population of children with CP at GMFCS levels III-V. The data was collected from the Swedish CP registry and follow-up Program (CPUP) and included annual radiographic examinations of 353 children. They found that Children at GMFCS V have a significantly higher risk of hip displacement compared with children at GMFCS III–IV. The risk thought to be highest at 2-3 years of age [6].
CLASSIFICATION
Cerebral palsy can be classified according to the motor type which includes spastic, dystonic, mixed, ataxic, or hypotonic. Another classification depends on the topographical distribution which could be either spastic hemiplegia, spastic diplegia or spastic quadriplegia [7].
The creation of the Gross Motor Function Classification System (GMFCS) has made a huge impact on the way cerebral palsy is classified. The GMFCS is a grading system that describes the gross motor function of children and youth with cerebral palsy. Distinctions between levels are based on functional limitations, the need for walking aids or assistive equipment and the quality of movement [8].
ETIOLOGY AND PATHOLOGY
The resulting hip subluxation causes erosion of the lateral lip of the acetabulum and as acetabular changes continue, an increase in the acetabular angle is noted.
Finally, deformity of the femoral head occurs as a result of pressure from the capsule, the rim of the acetabulum, the abductors, and the ligamentum teres [12]. Also, the position of the hip in adduction may contribute to the development of pelvic obliquity and subsequent scoliosis.
DIAGNOSTIC EVALUATION
Physical examination is then followed by radiological assessment. The earliest signs of hip instability include subtle break in shenton’s line and uncovering of the most lateral aspect of the femoral head by a shallow acetabulum. The amount of femoral head protruding past the lateral border of the acetabulum can be qualified by Reimers’ migration percentage, or the percentage of transverse diameter of the femoral head that lies lateral to Perkins’ line, which is drawn at the edge of the acetabulum [14] (Figure 1). The acetabular index will be increased because of acetabular dysplasia. Coxa valga and increased femoral anteversion is demonstrated by increased neck shaft angle.In Bagg et al., series, he showed that hips with Migration Index (MI) < 50% may reduce spontaneously or at least remain subluxated. Hips with MI > 50% remained subluxated or progressed to dislocation [15].
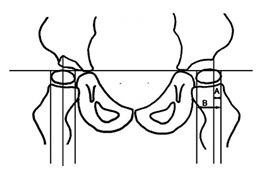
Figure 1: Measurement of Migration Percentage (MP).
A study of 39 patients by Foroohar and colleagues demonstrated that Head Shaft angle is greater in children with CP than in typically developing children and this is more pronounced in patients who are at risk for eventual subluxation [16].
MANAGEMENT
Miller and Bagg studied the prevalence of progression of subluxation based on the age of the patients. Their study involved 143 untreated hips in patients with cerebral palsy. 75% of the hips with Reimer’s migration indices of less than 30% did not progressively subluxate and those that did progress were individuals younger than 18 years. All hips with migration indices of greater than 60% eventually dislocated [17].
PREVENTION
Non-operative treatments for hip displacement are preventive in nature. Various braces and postural alignment systems have been used aiming to maintain adequate hip abduction and to prevent progressive contractures of the muscles and consequent hip dislocation. However, several studies have shown that fixed abduction braces are not well tolerated in children with cerebral palsy [20].
BOTULINUM TOXIN
Other treatment measures used is Intrathecal Baclofen Pump (ITBP) and Selective Dorsal Rhizotomy (SDR). Silva and colleagues found no significant difference in the rate of secondary hip reconstructive surgery or dislocation between non-ambulatory cerebral palsy patients who underwent SDR versus ITBP. Reconstruction was still required for 25% to 32% of the hips [22].
CATEGORIES OF SURGICAL TREATMENT
• Soft tissue release.
• Hip reconstruction surgery which include femoral and pelvic osteotomies.
• Salvage surgery for long-standing painful hip dislocations [1].
Soft tissue release
A hip at risk is defined as a hip with significant amount of muscle contractures but minimal subluxation and a migration index of less than 30% [23]. Soft tissue release is indicated in a child who is preferably not older than 5 years with hip abduction less than 30 degrees, flexion contracture more than 45 degrees and a migration index which is greater than 25% to 30% [4].
In the treatment of a spastic hip a variety of soft tissue procedures is recommended, including partial or total tenotomy of the adductors and iliopsoas. The goal of these procedures is to achieve the optimum muscular balance. Tenotomies of the hip adductor muscle in patients with spastic cerebral palsy are the most common soft tissue procedures in the treatment of hip contractures [24].
Presedo and colleagues reviewed the results of adductor and iliopsoas release for patients with mild hip subluxation. With 10 years follow up their study concluded that soft-tissue release was effective for long-term prevention of hip dislocation in 67% (forty-three of sixty five) of children with spastic hip subluxation. Two preoperative factors were related to a favourable outcome: spastic diplegic pattern of involvement and the ability to walk. The hip migration percentage at one year postoperatively was a good predictor of final outcome [25]. On the other hand Turker and colleagues found that 58% of patients who had adductor myotomy and were followed for 8 years required further surgery for hip subluxation or dislocation after soft tissue release [26].
Anterior branch obturator neurectomy is performed if children have greater than 60% migration and are not expected to have ambulatory ability in the future.
Reconstruction surgery for subluxated or dislocated hips
Femoral osteotomy
The aim is to achieve a neck-shaft angle of 90 to 100 degrees. Various methods of internal fixation have been used but the most common ones are a hip screw with a side plate and a 90-degree blade plate [28].
The osteotomy is usually accompanied with release of soft tissue contractures in order to balance the forces across the hip. Patient is then immobilized in a spica cast [29].
Several studies have compared the outcomes of hips treated with Varus Derotational Osteotomy (VDRO) only and hips treated with VDRO and pelvic osteotomy. Al Ghadir and colleagues found superior results with addition of pelvic osteotomy, and the authors recommended against VDRO alone [30]. Song and Carroll advocated pelvic osteotomy if the preoperative migration index is greater than 70% [31].
Pelvic osteotomies
Dega’s osteotomy
A study done by Mubarak and colleagues reported the outcomes following Dega osteotomy combined with adductor, iliopsoas and proximal hamstring release as well as a shortening femoral VDRO. Results showed that 95% of the 104 hips remained stable after 7 years follow-up, although AVN occurred in 8% of hips. The study concluded that with Dega’s osteotomy excellent correction of the superior and lateral deficiency was achievable [33].
Chiari’s osteotomy
In a study reported by Pope and associates, 3 different types of pelvic osteotomies were performed on 21 patients with cerebral palsy. Five of seven hips treated with VDRO and a Chiari osteotomy remained stable. They advocated the use of Chiari osteotomy in the presence of severe subluxation or if there is moderate incongruity on arthrography after the femoral osteotomy [35].
Shelf acetabular augmentation
The operation is not recommended if dysplastic hip is suitable for redirectional osteotomy or if there is a need for supplementary stability following open reduction. Also patients who are not suitable for spica cast immobilisation are not candidates for this procedure [37].
Bernese peri-acetabular osteotomy
Although bernese periacetabular osteotomy was more common in the treatment of adolescent hip dysplasia, modifications of this osteotomy have been used in patients with cerebral palsy. More studies have shown that better coverage can be obtained because of the ability to redirect the acetabulum with great ease [39].
Pemberton osteotomy
Salvage surgery for dislocated hips
Proximal femoral resection-interposition arthroplasty
It is essential to perform the femoral resection at a level no more proximal than the level of the inferior aspect of the ipsilateral ischial ramus, or 3 cm distal to the lesser trochanter [41]. A more proximal resection can lead to increased pain after surgery due to the proximal migration of the femoral shaft as a result of spasticity [42].
Another problem reported following proximal femoral resection is heterotopic bone formation with substantial stiffness of the resected hip. Egermann and colleagues published their results following the use of femoral head to cap the proximal femur and showed a decreased rate of heterotopic ossification [43].
Although several studies have reported good outcomes after the surgery, it can take up to 6 to 9 months before obtaining proper pain relief [44].
Total hip arthroplasty
Few technical aspects need to be considered while performing the procedure for cerebral palsy patients: first, flexing the acetabular component will provide more posterior stability in sitting position. Second, bone grafting may be required to compensate for the bone loss in the superolateral aspect of the acetabulum [1]. Root and colleagues recommended the use of spica for 4 weeks after surgery [45].
Raphael and colleagues reported on 59 hips who underwent total hip arthroplasty. Complete pain relief was obtained by 48 of 59 patients (81%), and reduction of preoperative pain was achieved by all patients. The 2-year survival was 95% (56 of 59). Revision rate was 15% (9 of 59). There were 8 dislocations (14%) [46].
Hip resurfacing with femoral osteotomy for painful, subluxated or dislocated hips in patients with cerebral palsy has been reported, Prosser and colleagues showed a series of 19 patients (20 hips) treated with hip resurfacing and proximal femoral osteotomy. The mean follow-up was 8 years. Pain was relieved in 16 of the 18 surviving hips (89%) at the last follow-up, and the GMFCS level had improved in seven (37%) patients [47].
Valgus osteotomy of the proximal end of the femur
However, pain relief following the osteotomy may not be predictably achieved and patients may continue to have problems with sitting because of the abduction position of the leg post-operatively. The femoral head may also be prominent causing pressure problems [1].
Another option is combining the valgus osteotomy with a femoral head resection as described by McHale and associates [49]. Leet and colleagues compared the outcomes of McHale procedure (valgus osteotomy and femoral head resection) and femoral head resection and traction. They found that with valgus osteotomy and proximal femoral resection, the superior migration of the femoral head was less pronounced although there was no significant difference in the long-term caregiver satisfaction [50].
Hip arthrodesis
Root and colleagues reported on the outcomes of hip arthrodesis for CP patients. They used a combined intra-articular and extra-articular technique with subtrochanteric osteotomy of the femur to promote fusion. Two of the eight patients developed pseudoarthrosis and underwent revision. Their recommendation for hip arthrodesis is a young adult with normal contralateral hip and no lumbo-sacral spine deformity [45].
A study by De Moraes Barros Fucs and associates found that hip arthrodesis had good results in ambulatory patients especially those with unilateral hip involvement. The mean position of fusion was 40 degrees of flexion, 15 degrees of abduction, and neutral rotation. Among the seven bedridden patients, five were able to remain seated and two were able to walk [52].
CONCLUSION
REFERENCES
- Herring John A (2008) The neuromuscular system. Tachdjian’s Pediatric orthopedics. Saunders Elsevier Inc, Philadelphia, USA.
- Brunner R, Baumann JU (1997) Long-term effects of intertrochanteric varus-derotation osteotomy on femur and acetabulum in spastic cerebral palsy: an 11- to 18-year follow-up study. J Pediatr Orthop 17: 585-591.
- Boyle CA, Yeargin-Allsopp M, Doernberg NS, Holmgreen P, Murphy CC, et al. (1996) Prevalence of selected developmental disabilities in children 3-10 years of age: the Metropolitan Atlanta developmental disabilities surveillance program, 1991. MMWR Surveillance Summaries, Centers for Disease Control and Prevention, Atlanta, Georgia, USA. 45: 1-14.
- Flynn JM, Miller F (2002) Management of hip disorders in patients with cerebral palsy. J Am Acad Orthop Surg 10: 198-209.
- Soo B, Howard JJ, Boyd RN, Reid SM, Lanigan A, et al. (2006) Hip displacement in cerebral palsy. J Bone Joint Surg Am 88: 121-129.
- Larnert P, Risto O, Hägglund G, Wagner P (2014) Hip displacement in relation to age and gross motor function in children with cerebral palsy. J Child Orthop 8: 129-134.
- Sanger TD, Delgado MR, Gaebler-Spira D, Hallett M, Mink JW (2003) Classification and definition of disorders causing hypertonia in childhood. Pediatrics 111: 89-97.
- Wood E, Rosenbaum P (2000) The gross motor function classification system for cerebral palsy: a study of reliability and stability over time. Dev Med Child Neurol 42: 292-296.
- Graham HK (2002) Painful hip dislocation in cerebral palsy. Lancet 359: 907-908.
- Long C (1995) Handbook of Pediatric Physical Therapy. Williams & Wilkins, Baltimore, USA. Pg no: 198-200.
- Miller F, Slomczykowski M, Cope R, Lipton GE (1999) Computer modeling of the pathomechanics of spastic hip dislocation in children. J Pediatr Orthop 19: 486-492.
- Lundy DW, Ganey TM, Ogden JA, Guidera KJ (1998) Pathologic morphology of the dislocated proximal femur in children with cerebral palsy. J Pediatr Orthop 18: 528-534.
- Bozinovski Z, Poposka A, Serafimoski V (2008) Hip reduction in cerebral palsy with soft tissue operative procedures. Prilozi 29: 211-219.
- Reimers J (1980) The stability of the hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand Suppl 184: 1-100.
- Bagg MR, Farber J, Miller F (1993) Long-term follow-up of hip subluxation in cerebral palsy patients. J Pediatr Orthop 13: 32-36.
- Foroohar A, McCarthy JJ, Yucha D, Clarke S, Brey J (2009) Head-shaft angle measurement in children with cerebral palsy. J Pediatr Orthop 29: 248-250.
- Miller F, Bagg MR (1995) Age and migration percentage as risk factors for progression in spastic hip disease. Dev Med Child Neurol 37: 449-455.
- Miller F, Dabney KW, Rang M (1995) Complications in cerebral palsy treatment. In: Epps CH Jr, Bowen JR (eds.). Complications in pediatric orthopaedic surgery. JB Lippincott, Philadelphia, Pennsylvania, USA. Pg no: 477-544.
- Dobson F, Boyd RN, Parrott J, Nattrass GR, Graham HK (2002) Hip surveillance in children with cerebral palsy. Impact on the surgical management of spastic hip disease. J Bone Joint Surg Br 84: 720-726.
- Bleck EE (1987) Orthopaedic management in cerebral palsy. Mac Keith Press, Philadelphia, Pennsylvania, USA.
- Willoughby K, Ang SG, Thomason P, Graham HK (2012) The impact of botulinum toxin A and abduction bracing on long-term hip development in children with cerebral palsy. Dev Med Child Neurol 54: 743-747.
- Silva S, Nowicki P, Caird MS, Hurvitz EA, Ayyangar RN, et al. (2012) A comparison of hip dislocation rates and hip containment procedures after selective dorsal rhizotomy versus intrathecal baclofen pump insertion in nonambulatory cerebral palsy patients. J Pediatr Orthop 32: 853-856.
- Kalen V, Bleck EE (1985) Prevention of spastic paralytic dislocation of the hip. Dev Med Child Neurol 27: 17-24.
- Bozinovski Z, Zairoski G, Karevski Lj, Poposka A, Gavrilovski A (2008) Soft tissue surgical procedures in the prevention of hip dislocation in patients with spastic cerebral palsy. Georgian Med News.
- Presedo A, Oh CW, Dabney KW, Miller F (2005) Soft-tissue releases to treat spastic hip subluxation in children with cerebral palsy. J Bone Joint Surg Am 87: 832-841.
- Turker RJ, Lee R (2000) Adductor tenotomies in children with quadriplegic cerebral palsy: longer term follow-up. J Pediatr Orthop 20: 370-374.
- Miller F (2005) Cerebral palsy. Springer, New York, USA.
- Hau R, Dickens DR, Nattrass GR, O’Sullivan M, Torode IP, et al. (2000) Which implant for proximal femoral osteotomy in children? A comparison of the AO (ASIF) 90 degree fixed-angle blade plate and the Richards intermediate hip screw. J Pediatr Orthop 20: 336-343.
- Hoffer MM, Stein GA, Koffman M, Prietto M (1985) Femoral varus-derotation osteotomy in spastic cerebral palsy. J Bone Joint Surg Am 67: 1229-1235.
- Al-Ghadir M, Masquijo JJ, Guerra LA, Willis B (2009) Combined femoral and pelvic osteotomies versus femoral osteotomy alone in the treatment of hip dysplasia in children with cerebral palsy. J Pediatr Orthop 29: 779-783.
- Song HR, Carroll NC (1998) Femoral varus derotation osteotomy with or without acetabuloplasty for unstable hips in cerebral palsy. J Pediatr Orthop 18: 62-68.
- Grudziak JS, Ward WT (2001) Dega osteotomy for the treatment of congenital dysplasia of the hip. J Bone Joint Surg Am 83A: 845-54.
- McNerney NP, Mubarak SJ, Wenger DR (2000) One-stage correction of the dysplastic hip in cerebral palsy with the San Diego acetabuloplasty: results and complications in 104 hips. J Pediatr Orthop 20: 93-103.
- Chiari K (1974) Medial displacement osteotomy of the pelvis. Clin Orthop Relat Res.
- Pope DF, Bueff HU, DeLuca PA (1994) Pelvic osteotomies for subluxation of the hip in cerebral palsy. J Pediatr Orthop 14: 724-730.
- Turgeon TR, Phillips W, Kantor SR, Santore RF (2005) The role of acetabular and femoral osteotomies in reconstructive surgery of the hip: 2005 and beyond. Clin Orthop Relat Res 441: 188-199.
- Staheli LT, Chew DE (1992) Slotted acetabular augmentation in childhood and adolescence. J Pediatr Orthop 12: 569-580.
- Ganz R, Klaue K, Vinh TS, Mast JW (1988) A new periacetabular Osteotomy for the treatment of hip dysplasia: Technique and Preliminary results. Clin Orthop Relat Res 232: 26-36.
- Roposch A, Wedge JH (2005) An incomplete periacetabular osteotomy for treatment of neuromuscular hip dysplasia. Clin Orthop Relat Res Pg no: 166-175.
- Kelly DM (2013) Congenital and Developmental Anomalies of the Hip and Pelvis. Campb Oper Orthop Mosby, Elsevier, Missori, USA.
- McCarthy RE, Simon S, Douglas B, Zawacki R, Reese N (1988) Proximal femoral resection to allow adults who have severe cerebral palsy to sit. J Bone Joint Surg Am 70: 1011-1016.
- Perlmutter MN, Synder M, Miller F, Bisbal R (1993) Proximal femoral resection for older children with spastic hip disease. Dev Med Child Neurol 35: 525-531.
- Egermann M, Döderlein L, Schläger E, Müller S, Braatz F (2009) Autologous capping during resection arthroplasty of the hip in patients with cerebral palsy. J Bone Joint Surg Br 91: 1007-1012.
- Widmann RF, Do TT, Doyle SM, Burke SW, Root L (1999) Resection arthroplasty of the hip for patients with cerebral palsy: an outcome study. J Pediatr Orthop 19: 805-810.
- Root L, Goss JR, Mendes J (1986) The treatment of the painful hip in cerebral palsy by total hip replacement or hip arthrodesis. J Bone Joint Surg Am 68: 590-598.
- Raphael BS, Dines JS, Akerman M, Root L (2010) Long-term followup of total hip arthroplasty in patients with cerebral palsy. Clin Orthop Relat Res 468: 1845-1854.
- Prosser GH, Shears E, O’Hara JN (2012) Hip resurfacing with femoral osteotomy for painful subluxed or dislocated hips in patients with cerebral palsy. J Bone Joint Surg Br 94: 483-487.
- Hogan KA, Blake M, Gross RH (2007) Subtrochanteric valgus osteotomy for chronically dislocated, painful spastic hips. Surgical technique. J Bone Joint Surg Am 89: 226-231.
- McHale KA, Bagg M, Nason SS (1990) Treatment of the chronically dislocated hip in adolescents with cerebral palsy with femoral head resection and subtrochanteric valgus osteotomy. J Pediatr Orthop 10: 504-509.
- Leet AI, Chhor K, Launay F, Kier-York J, Sponseller PD (2005) Femoral head resection for painful hip subluxation in cerebral palsy: Is valgus osteotomy in conjunction with femoral head resection preferable to proximal femoral head resection and traction? J Pediatr Orthop 25: 70-73.
- Renshaw TS, Green NE, Griffin PP, Root L (1996) Cerebral palsy: orthopaedic management. Instr Course Lect 45: 475-490.
- 52. de Moraes Barros Fucs PM, Svartman C, de Assumpção RM, Kertzman PF (2003) Treatment of the painful chronically dislocated and subluxated hip in cerebral palsy with hip arthrodesis. J Pediatr Orthop 23: 529-534.
Citation: Eldessouky A, Smeda G (2016) Hip Dislocation in Cerebral Palsy: Treatment Options. J Orthop Res Physiother 2: 026.
Copyright: © 2016 Eldessouky A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

