Impact of a PharmD Consult to Improve Futile Medication Discontinuation Rates in a Home Hospice Program
*Corresponding Author(s):
Christopher M HerndonSouthern Illinois University Edwardsville School Of Pharmacy, United States
Email:Cherndon12@gmail.com
Abstract
Objectives: The primary objective of this study was to determine if discontinuation rates of related but medically unnecessary medications (RMU) and conversion rates of related but non-formulary medications (RNF) to formulary equivalents were increased when patients or caregivers spoke with a pharmacist versus nurse upon admission to a home hospice program. The secondary objective of this study was to determine average cost savings once these medications were discontinued or converted.
Design: Observational, retrospective chart review.
Setting and Participants: The hospice was a community not for profit home hospice program serving 27 counties in southern Illinois. Inclusion criteria included any patient admitted to hospice between November 1, 2017 and March 19, 2018 that were receiving any medications deemed as RMU or RNF. Exclusion criteria included patients admitted while the hospice pharmacist was on vacation and if the patients died prior to intervention by either nurse or pharmacist.
Outcome Measures: Frequency of RMU and RNF medication discontinuations, estimated cost savings
Results: Of the 57 RMU and RNF medications identified, 29 (51%) were successfully discontinued or switched to formulary alternatives by either the nurse or pharmacist, while 28 attempts were unsuccessful. Cases assigned to the pharmacist resulted in a 66% success rate, compared to a 35% success rate in cases assigned to a nurse (x2 5.1, df 1, p=0.035).
Conclusion: The hospice pharmacist was able to more successfully discontinue RMU medications compared with nurses; however the conversion of RNF medications to formulary equivalents was no different between pharmacist and nurse. The addition of a pharmacist to hospice teams appears to be effective and may result in significant cost savings for both patients and hospice organizations.
Key Points
Background
- • No current literature to support benefit of pharmacists on deprescribing in home hospice programs
- • Pharmacists serve as medication experts and are underutilized in this healthcare setting
Findings
- • Pharmacists should be utilized in hospice programs to assist with cost savings and medication deprescribing
- • Pharmacists can improve patient care and quality of life through deprescribing efforts
Keywords
Healthcare setting; Home hospice programs; PharmD
BACKGROUND
Hospice services provide exceptional patient and family care at end-of-life. While the roles of physicians, nurses, and social workers, among others, are clearly defined, the role of the pharmacist in hospice care is less documented. Pharmacists serve as the drug experts in a variety of circumstances, but pharmacists employed by hospice programs are scarce. Furthermore, the benefits of pharmacist services to hospice organizations are frequently overlooked, despite potentially leading to improved symptom control, significant cost savings for hospice programs and patients, and decreased futile medications.
Existing evidence for pharmacists’ roles within hospice revolves around clinical consultation, dispensing, and administrative services [1]. A pilot study in two Maryland hospice programs evaluated the accuracy of medication reconciliations performed first by nurses and followed five days later by pharmacists. These medication reconciliations were then compared to determine any discrepancies and a total of 504 discrepancies were found between nurses and pharmacists [2].
Before further discussion of de-prescribing at the end-of-life, a brief review of processes that determine futile medications is warranted. Once admitted to a hospice program, a patient’s medications are reviewed by a hospice physician and categorized as a) unrelated to terminal prognosis, b) related to terminal prognosis and medically necessary, c) related to terminal prognosis but medically unnecessary (RMU), or d) related to terminal prognosis but non-formulary (RNF). Futile medications are defined as any medication that is no longer necessary at end-of-life and can be in any of the aforementioned categories. Hospice programs, based on Medicare Conditions of Participation, are required to pay for any medications considered related to the terminal prognosis and medically necessary. If a medication is considered unrelated to the terminal prognosis, the patient may continue to receive the medication and may also continue to bill their pre-existing prescription insurance, if applicable [3]. Payment is less clearonce a medication is categorized as related but medically unnecessary or related but non-formulary. If a medication is classified into one of these categories, the cost may become the patient or caregiver’s responsibility and can no longer be submitted to insurance for coverage, which can place a significant cost burden on patients and their families [3]. See figure 1 for a detailed review of payment in these situations.
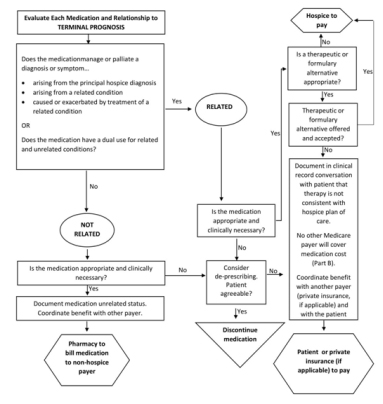 Figure 1: Determining Payment for Medications upon Admission to Home Hospice Services [4]
Figure 1: Determining Payment for Medications upon Admission to Home Hospice Services [4]
While some evidence exists to support the benefits of pharmacist-led deprescribing efforts in long-term care facilities, to date, there are no studies evaluating the effectiveness of pharmacist communication with patients or caregivers regarding discontinuation of RMU and RNF medications in hospice [5].
OBJECTIVES
The primary objective of this study was to determine if discontinuation rates of related but medically unnecessary medications (RMU) and conversion rates of related but non-formulary medications (RNF) to formulary equivalents were increased when patients or caregivers spoke with a pharmacist versus nurse upon admission to a home hospice program. The secondary objective of this study was to determine average cost savings once these medications were discontinued or converted.
METHODS
Setting
The hospice program is community not for profit hospice that employs a full-time physician, nurse practitioner, and pharmacist (post-graduate year 2 pain and palliative resident) in addition to seven associate medical directors, one part-time nurse practitioner, 46 nurses, eight social workers, and four bereavement counselors. This hospice provides services in downstate Illinois covering 27 counties with an average daily census of approximately 200 patients.
Subjects
At the time of patient-admission, both RMU (futile) and RNF medications were identified by the hospice medical director. These cases were then assigned to either a hospice nurse or pharmacist to initiate discussions with patients or caregivers on discontinuation of RMU medications or the switch of RNF medications to formulary equivalents.
After receiving exempt status from the Southern Illinois University Edwardsville Institutional Review Board, a retrospective chart review was performed over a 5 month period to identify all patient admissions to a home hospice program with RMU and RNF medications.
Inclusion criteria included any patient admitted to the hospice between November 1, 2017 and March 19, 2018 that were receiving any medications deemed as RMU or RNF. Exclusion criteria included patients admitted while the hospice pharmacist was on vacation and if the patients died prior to intervention by either nurse or pharmacist.
Data Collection
Data abstracted included RMU / RNF medication indication, primary care provider or hospice provider management of pain and symptoms, site of patient care, age, gender, race, and disposition of the RMU / RNF medication.
Analysis
General descriptive statistics are reported. Categorical data was compared using the Pearson Chi-squared test to determine statistical significance with a two-tailed alpha set at 0.05. All analysis was conducted using SPSS 24.0 (IBM SPSS, Chicago, IL).
RESULTS
Seventy-one medication cases were initially eligible to be included in this study, however only 57 remained eligible after excluding for patient death prior to intervention and omitting admissions taking place during the pharmacist’s vacation time as these patients were not properly assigned to nurse or pharmacist.Baseline characteristics and medication discontinuation rates can be found in table 1.
|
|
All Medications (%) n = 57 |
Discontinued (total = 29) |
P-value |
|
|
Discontinued by Pharmacist (%) n = 19 |
Discontinued by Nurse (%) n = 10 |
|||
|
Demographics Race African-American Caucasian Gender Male Female Age <90 90+ |
3 (5) 54 (95)
24 (42.1) 33 (57.9)
47 (82.5) 10 (17.5) |
2 (6.9) 17 (58.6)
6 (20.7) 13 (44.8)
19 (65.5) 0 |
0 10 (34.8)
5 (17.2) 5 (17.2)
6 (20.7) 4 (13.8) |
0.003
0.331
0.288
|
|
Patient Location^ ALF LTC Home |
4 (7) 28 (49.1) 25 (43.9) |
0 9 (31) 10 (34.8) |
1 (3.4) 9 (31) 0 |
0.11
|
|
Pain and Symptom Management◊ Hospice Other physician |
39 (68.4) 18 (31.6) |
10 (34.8) 9 (31) |
10 (34.8) 0 |
0.009
|
|
Indication of Futile Medication† Dementia COPD Hyperlipidemia DVT/PE AFIB Anemia Other |
7 (12.3) 21 (36.9) 1 (1.8) 7 (12.3) 3 (5.3) 3 (5.3) 15 (26.3) |
2 (6.9) 11 (37.9) 0 1 (3.4) 2 (6.9) 0 3 (10.3) |
0 2 (6.9) 0 3 (10.3) 1 (3.4) 0 4 (13.8) |
0.161
|
Table 1: Baseline Characteristics and Medication Discontinuations.
^ALF = assisted-living facility; LTC = long-term care facility
◊Certifying physician is given option to manage pain and symptoms once patient is admitted to hospice
†COPD = chronic obstructive pulmonary disease; DVT = deep vein thrombosis; PE = pulmonary embolism; AFIB = atrial fibrillation
Figure 2 outlines medication inclusion and exclusion data. Of the 57 RMU and RNF medication cases included, 29 (51%) were successfully discontinued or switched to formulary alternatives by either the nurse or pharmacist, while 28 attempts were unsuccessful. Cases assigned to the pharmacist resulted in a 66% success rate (n=19), compared to a 35% success rate (n=10) in cases assigned to a nurse (x2 5.1, df 1, p=0.035). Moreover, RMU medication discontinuation success was achieved in 68% of cases assigned to the pharmacist versus a nursing success rate of 24% (x2 7.3, df 1, p=0.01). Pharmacist and nurse success rates for RNF conversion to formulary alternatives were similar (60% and 55%, respectively, p = NS).
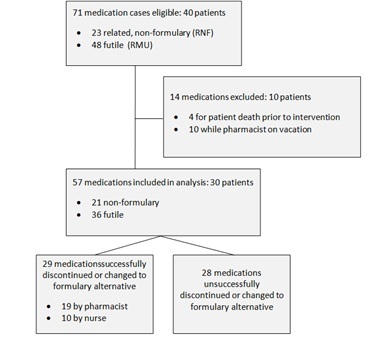 Figure 2: Medication Disposition.
Figure 2: Medication Disposition.
The 29 medications discontinued or switched to formulary alternatives saved patients approximately $4,468.70 in just over five months. These calculations were based on the available cash price (using GoodRx coupons) of each medication that was discontinued or converted multiplied by an estimated duration of therapy, approximately 30 days per our hospice average length of stay. No statistically significant differences were observed in intervention success rates between gender, ethnicity, site of care, or primary pain and symptom management provision.
DISCUSSION
When discussing futile medications with patients and families, many barriers exist that can preclude optimal patient-care, including demands of the family, patient or primary caregiver health literacy, lack of understanding regarding futile medications, and lack of consensus among the healthcare team [6]. Approaching the concept of futility of care with the dying patient and caregiver can be uncomfortable for many providers despite their expertise and experience. For this reason, efforts have been undertaken to develop a practice model that allows for evidence-based and compassionate care in these settings. This model, coined the “BUILD” model, provides a step-by-step process that allows interdisciplinary team members to approach discussions regarding futile medications [7]. This model focuses on building a foundation of trust and respect, understanding what the patient or caregiver knows about the futile medication, informing the patients and caregivers of evidence-based information about the futile medication, listening to the patient’s goals and expectations, and ending with the development of a plan of care [7]. Although this model helps facilitate a difficult discussion, it does not account for individual patient-specific or drug-specific variables. While education regarding futile medications serves as enough information to aid in discontinuation for some patients, it remains insufficient for a number of others [8].
This is in line with what was observed in this study and is perhaps the result of a paucity of hospice deprescribing guidelines or formal supporting educational materials developed for patients and caregivers [9].
As the medication experts, pharmacists are at an advantage when discussing discontinuation of RMU and substitution of RNF medications with hospice patients and their families. Pharmacists’ knowledge of adverse effects, interactions, and risks versus benefits of pharmacotherapy certainly supports effectively relaying these concerns to hospice patients. While both disciplines of nursing and pharmacist were successful in addressing RMU and RNF medication cases in a home hospice program, this study suggests pharmacists may be better positioned to address pharmacotherapy-specific educational needs of patients and caregivers. Furthermore, the cost savings that resulted from these discontinuations and formulary conversions help to better serve the patients and their families.
It is also crucial to mention the burden of polypharmacy on quality of lifewhile enrolled in hospice services. McNeil et al. found that the average number of medications taken per patient was 11.5 during end-of-life care [10]. This was associated with increased pill burden and increased adverse effects, both of which contribute to decreased quality of life measures during end-of-life care [10]. Another study found that increased number of medications was associated with higher symptom burden and decreased quality of life in adults with advanced illness [11]. As evidenced above, discussions surrounding medications during end-of-life care is warranted to address quality of life measures and improve patient satisfaction.
LIMITATIONS
Several limitations of this study exist. One such limitation is the use of soft dollars being analyzed to report cost savings data. The estimated savings are not exact and were calculated based on cash price of the medication for a one month supply, which is a slight underestimation of the average length of stay at 41 days. However, this did not take into account how many days supply of medication the patient may have had when admitted to hospice, possibly resulting in a slight over-estimation of total cost savings. Additionally, a comparative analysis of actual cost to patient for similar or same RMU / RNF drug therapy in those who chose not to discontinue an RMU or transition from an RNF medication would provide a more accurate description of cost data. Furthermore, the emphasis of this study was to focus on RMU / RNF medications, rather than other futile medications that were deemed unrelated, such as antihyperlipidemics. Some other limitations include small sample size, lack of standardized or scripted patient education materials, and retrospective nature of the study. As a quality improvement project, true randomization of RMU / RNF cases was not feasible. Lastly, we did not assess interpatient variability to determine if certain classes of medications were more willing to be discontinuedcompared to others. This could be an insightful future direction for other hospice programs to evaluate to assist with cost savings and quality of life measures.
CONCLUSION
Pharmacists serve as the medication experts in a variety of different clinical settings; however their role in hospice deprescribing and formulary support is not well documented. Although both nurse and pharmacist intervention for RMU and RNF medication was successful, the hospice pharmacist achieved successful discontinuation more frequently. While larger, prospective studies are required, the addition of a pharmacist intervention when attempting to discontinuing futile medications or transition non-formulary, medically necessary medications appears to be effective and may result in significant cost savings for patients and their families.
DECLARATION OF INTEREST
Authors have nothing to disclose.
REFERENCES
- Latuga NM, Wahler RG, Monte SV (2012) A national survey of hospice administrator and pharmacist perspectives on pharmacist services and the impact on medication requirements and cost. Am J Hosp Palliat Med 29: 546-554.
- Kemp LO, Narula P, McPherson ML, Zuckerman I (2009) Medication reconciliation in hospice: a pilot study. Am J Hosp Palliat Care 26: 193-199.
- Centers for Medicare and Medicaid Services. Hospice Regulations and Notices, CMS.govr, USA.
- National Hospice and Palliative Care Organization (2018). Determination of Hospice Mediation Coverage, Version 1.0., NHPCO, USA.
- Pruskowski J, Handler SM (2017) The DE-PHARM Project: A pharmacist-Driven deprescribing initiative in a nursing facility. Consult Pharm 32: 468-478.
- Sibbald R, Downar J, Hawryluck L (2007) Perceptions of “futile care” among caregivers in intensive care units. CMAJ 177: 1201-1208.
- Collier KS, Kimbrel JM, Protus BM (2013) Medication appropriateness at end of life: a new tool for balancing medicine and communication for optimal outcomes-the BUILD model. Home Healthc Nurse 31: 518-524.
- Martin P, Tannenbaum C (2017) A realist evaluation of patients’ decisions to deprescribe in the EMPOWER trial. BMJ Open7:
- Narayan SW, Nishtala PS (2017) Discontinuation of preventive medicines in older people with limited life expectancy: A Systematic Review. Drugs Aging 34: 767-776.
- McNeil MJ, Kamal AH, Kutner JS, Ritchie CS, Abernethy AP (2016) The Burden of Polypharmacy in Patients Near the End of Life. J Pain Symptom Manage 51: 178-83.
- Schenker Y, Park SY, Jeong K, Pruskowski J, Kavalieratos D, et al. (2019) Associations Between Polypharmacy, Symptom Burden, and Quality of Life in Patients with Advanced, Life-Limiting Illness. J Gen Intern Med 34: 559-566.
Citation: Mullins AM, Herndon CM (2020) Impact of a PharmD Consult to Improve Futile Medication Discontinuation Rates in a Home Hospice Program. J Hosp Palliat Med Care 3: 011.
Copyright: © 2020 Amanda M Mullins, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.