
Legg-Calvé-Perthes Disease and Its Physiotherapy - “If the Hip Melts Away”
*Corresponding Author(s):
Krieg AHDepartment Of Orthopedics, University Children’s Hospital Basel (UKBB), Basel, Switzerland
Tel:+41 617041212,
Email:andreas.krieg@ukbb.ch
Abstract
Legg-Calvé-Perthes disease (or Perthes disease) is a disorder of the hip, which is caused by a vascular disorder ischemia of the femoral head and passes through four stages. It affects mostly infants and children of caucasian population. The cause of the ischemia is not yet known and therefore cannot be prevented norreversed. Limping, restriction of the movement and pain can lead to the diagnosis. X-rays as well as Magnetic Resonance Imaging (MRI) confirms it. The classification of Herring (A-C) is helpful to make a clinical prognosis and further treatment. The main aim of therapy is to improve joint the mobility and the joint’s congruence (“containment”), build up muscle strength and reduce pain. Physiotherapy is an undisputed method, lasts over years involving an extensive movement therapy of the affected hip, the torso and the non-affected limb. Short-term drug-related analgesia, botulinum injection into the adductors and a weight relief can accompany therapy. An indication for operative treatment is given by subluxation within stadium B or B/C of Herring. Containment (hip centering/ joint’s congruence) can be achieved by femoral varization osteotomy or pelvic osteotomy. Only one quarter of all patients is treated with surgery and physiotherapy remains the most relevant therapy on Perthes disease.
Keywords
INTRODUCTION
An unclear cause one reason behind the lack of control and influence over the disease is due to the inability to find its cause (s). However, research has found that various factors play a role in its development. Next to genetic factors [1,2] and a possible coagulation disorder [3,4], LCPD is caused by a local circulatory disorder [5] on the basis of a skeletal disorder, with delayed growth occurring between the ages of 4-6 years [6-9].
Incidence
Clinics and diagnostics young patients can be identified through their limping or through the pain within their hip joints. Sometimes these symptoms are directly associated with limited hip joint mobility. Often the hip pain occurs approximately 6-8 weeks before the radiology’s findings. As a result of a possible collection of liquid within the joint, LCPD can be confounded by a coxitis fugax.
Changes in the scintigram or MRI can already be found at the initial stage. However, given the current state of research, early diagnosis does not alter the subsequent treatment. In any case, the initial stage of LCPD would not be treated, unless a restricted mobility of the hip is present. If this persists for more than two weeks, physiotherapy is prescribed, independent of whether it is a LCPD or a coxits fugax. Six weeks later LCPD can be easily diagnosed, if found to be present on a conventional X-ray image (method of choice) [12]. It is therefore possible to spare the child the MRI examination, which is expensive and invasive due to the anesthesia at this age [13].
Currently it is being tested in various centers, whether an early MRI-diagnosis and early surgical indication have clinical advantages instead of X-rays. A special perfusion-MRI therein specifies the extent of the necrosis of the femoral head (MRI-classifications) [14].
Classifications
• Condensation stage (Ø 7 months)
• Fragmentation stage (Ø 8.5 months)
• Reossification stage (Ø 18 months)
• End stage [15]

Figure 1: Four stages of how the disease progresses (left to right): a) 3-year old boy, head of femur within condensation stage. b) Fragmentation stage at the age of 5 (see arrow for fragmentation line). c) Reparation stage at the age of 7. d) End stage at the age of 9, good relation between the height of the femoral head and the trochanter major (see double arrow).
The older the child at the beginning of the disease, the longer the individual phases last. All classifications are based on a morphological classification according to an X-ray image [16-18]. However, classifications are only useful if they had also contributed to the prognosis and thus to a decision as to therapy. The Herring classification has proven to be the best method in the last years. In addition to the radiological risk factors, table 1 also shows the clinical factors and their relevance to a poor prognosis. Many long-term studies have verified this [19-22].
|
Factors of Clinical and Radiological Prognosis |
Relevance |
|
Condition of the lateral hip pillar 1 |
+++ |
|
Lateral calcification 2 |
++ |
|
Subluxation (“containment”) 2 |
++ |
|
Age (>6 years) |
+++ |
|
Agility |
++ |
|
Sex (female) |
++ |
|
Extent of necrosis 3 |
+ |
|
Metaphysical participation 2 |
+ |
|
Horizontalization of the growth gap 2 |
- |
|
1. Risk factor according to Herring classification 2. Risk factor according to Catteral/“head at risk-sign” 3. Classification according to Catteral/Salter & Thompson |
|
METHODS
Therapy
According to the duration of the disease, an accompanying therapy has to take place over years with different frequencies. In acute painful phases, short-term drug-related analgesia, botulinum injection into the adductors and a discharge can treat as an adjuvant therapy. With the reduction of pain, better mobility can be quickly achieved as an improvement of the hip congruence, as well as the important adaptation of the head in the conversion to its joint partner, the acetabulum. All long-lasting relief methods (bed rest, relief abduction orthoses and crutches) are psychologically quite stressful. Since therapeutic effect has never been established, we never apply them [13].
Operative treatment
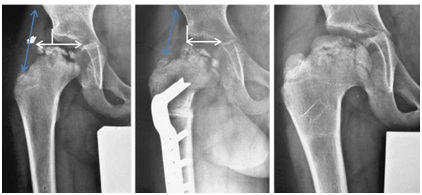
Figure 2: Patient with Perthes disease (Herring type C). a) Typical risk signs on the femoral head with lateral calcification and subluxation (white double arrow). b) Postoperatively following an intertrochanteric varising osteotomy, the abduction lever is shortened (blue double arrow). c) Healing in the end stage, good congruence (=containment) of the femoral head but with leg length discrepancy of 2cm and shorten abductors.
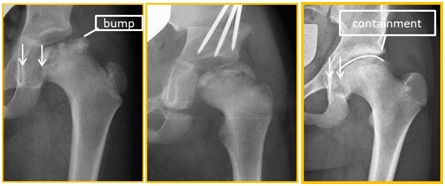
Figure 3: Improvement of the congruence (containment) by triple osteotomy in a nearly 7-year-old girl. a) Preoperative with lateralization and bump development b) Postoperatively, c) 5 years postoperatively. Immediately postoperatively the containment is not ideal, but improves rapidly by further growth and continuous movement. This is a typical development after triple osteotomy in Perthes disease.
Conservative Treatment for LCPD: Physiotherapy for patients with LCPD can last several years and places high demands on patients and their families. A major challenge for the physiotherapist is the compliance of the patient. Patients with LCPD usually has a more or less reduced mobility of the hip joint. Initially the restriction is of functional origin, later of structural origin [28] and affects above all the abduction, extension and internal rotation of the hip [28]. In addition the patients suffer a lack of power in their lower extremities and the trunk. Also a leg length discrepancy of the patient’s legs exists. The main points of the treatments are discussed below.
Objective and indication of physiotherapy the outcome of therapy is related to hip joint mobility. For that reason the restoration of the mobility is most important. Physiotherapy is indicated from initial diagnosis.
Medical prescription includes a report and a current X-ray image. Additional relevant diagnostic data needs to be put in writing (e.g., Attention Deficit Disorder, treated with medication, see table 2 for examples). If hip mobility worsens lasting more than 2-3 sessions, the treating physician should be contacted [29].
|
Prescription of long-term therapy with a clear diagnosis |
|
Example: LCPD right leg, stage 3 Length length discrepancy of 2cm Hyperlordosis of the lumbar spine Attention Deficit Disorder/Specific Learning Disability (SLD) |
Physiotherapeutic assessment an exact documentation including the joint status must be made (see table 3 for components).
|
Medical Assessment of LCPD |
|
Anamnesis/Medical report Pain (with the visual analogue scale) Passive and active ROM of the lower extremities as well as the lumbar spine (with a goniometer) Strength of the entire lower extremity (usually with a hand-held dynamometer) Statics, including indirect leg length testing (with small boards put underneath) Walking (walking analysis or video recording) Balance (standardized assessment) |
Possible differential diagnosis should be known by the physiotherapist (e.g., coxitisfugax, epiphyseal dysplasia, chondroblastoma). A status check should be repeated twice a year. This also applies to any extended therapy pauses. The Swiss quality circle "Children’s Orthopedic and its physiotherapy" has created an appropriate medical report.
Frequency of physiotherapy treatment involves an extensive movement therapy, which not only treats the affected hip but also the trunk and the non-affected limb. The frequency of treatment is adapted to each individual patient and must be reevaluated by the physiotherapist. If mobility decreases, the number of sessions should be increased to four times a week. Where hip mobility improves, therapy can be reduced to one or two times per month.
Joint mobility the Range Of Motion (ROM) should be improved passively by manual treatment. At the same time it should be improved by active and passive stretching of the affected muscle. Therefore the bone structures must allow abduction movement. An X-ray image is very important for the therapist. Ideally, after mobilization and stretching the new attained ROM can be exercised with strength-training e.g., squat-lunges or abduction-squats (Figure 4).
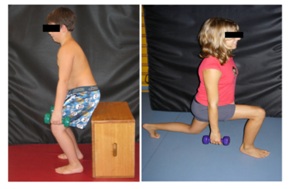
Figure 4: The newly gained degree of movement is exercised in its function: a) Squat b)Squat lung.
Balance and coordination training balance and coordination training as well as “core stability” (Figure 5) are important elements of every therapy session. To avoid more stress on the hip joint we don’t do any kind of jumps.

Medical advice on LCPD
Home exercises must be written down. They are adapted to age and to the individual patient. They must be regularly reviewed.
Therapy consensus for Switzerland currently every physiotherapist uses their own exercise program and treatments, depending on experience. Questionnaires concerning the quality of life are still used to rarely. Such questionnaires, especially for “non-curable” diseases, are very important. Various guidelines exist for the treatment of patients with LCPD [31]. We should bring this information and our know-how together, and adapt it accordingly to our environment. Our goal should be to achieve consensus on a treatment in Switzerland to implement it in practice.
CONCLUSION
Physiotherapy plays the most important role in the treatment of the LCPD. Although the cause of the disease cannot be prevented or cured, physiotherapy maintainship joint mobility which is highly important. It is indicated from the initial diagnosis and can last several years. It includes an extensive movement therapy for the affected hip but also the torso and the non-affected limb as well as balance, coordination training and home exercises. The frequency depends on the improvement or deterioration of the hip mobility and the pain. It is not advisable to have an orthotic support or to have a longer-lasting weight relief during the entire period of illness. In particular cases of the decentering of the hip, it is necessary to initiate an operative treatment.
REFERENCES
- Livesey JP, Hay SM, Bell MJ (1998) Perthes disease affecting three female first-degree relatives. J Pediatr Orthop B 7: 230-231.
- Miyamoto Y, Matsuda T, Kitoh H, Haga N, Ohashi H, et al. (2007) A recurrent mutation in type II collagen gene causes Legg-Calve-Perthes disease in a Japanese family. Hum Genet 121: 625-629.
- Vosmaer A, Pereira RR, Koenderman JS, Rosendaal FR, Cannegieter SC (2010) Coagulation abnormalities in Legg-Calvé-Perthes disease. J Bone Joint Surg Am 92: 121-128.
- Kim HK (2011) Legg-Calve-Perthes disease: Etiology, pathogenesis, and biology. J Pediatr Orthop 31: 141-146.
- Perry DC, Green DJ, Bruce CE, Pope D, Dangerfield P, et al. (2012) Abnormalities of vascular structure and function in children with Perthes disease. Pediatrics 130: 126-131.
- Cannon SR, Pozo JL, Catterall A (1989) Elevated growth velocity in children with Perthes' J Pediatr Orthop 9: 285-292.
- Kealey WD, Lappin KJ, Leslie H, Sheridan B, Cosgrove AP (2004) Endocrine profile and physical stature of children with Perthes disease. J Pediatr Orthop 24: 161-166.
- Kim HK, Skelton DN, Quigley EJ (2004) Pathogenesis of metaphyseal radiolucent changes following ischemic necrosis of the capital femoral epiphysis in immature pigs. A preliminary report. J Bone Joint Surg Am 86: 129-135.
- Vila-Verde VM, da Silva KC (2001) Bone age delay in Perthes disease and transient synovitis of the hip. Clin Orthop Relat Res 385:118-123.
- Perry DC, Bruce CE, Pope D, Dangerfield P, Platt MJ, et al. (2012) Perthes’ disease of the hip: Socioeconomic inequalities and the urban environment. Arch Dis Child 97: 1053-1057.
- Wiig O, Terjesen T, Svenningsen S, Lie SA (2006) The epidemiology and aetiology of Perthes’ disease in Norway. A nationwide study of 425 patients. J Bone Joint Surg Br 88: 1217-1223.
- Rampal V, Clément JL, Solla F (2017) Legg-Calvé-Perthes disease: Classifications and prognostic factors. Clin Cases Miner Bone Metab 14: 74-82.
- Hefti F (2015) Pediatric Orthopedics in Practice, (2nd edn). Springer, Berlin, Germany.
- Sankar WN, Thomas S, Castañeda P, Hong T, Shore BJ, et al. (2014) Feasibility and safety of perfusion MRI for Legg-Calvé-Perthes disease. J Pediatr Orthop 34: 679-682.
- Joseph B, Varghese G, Mulpuri K, Rao NK, Nair NS (2003) Natural evolution of perthes disease: A study of 610 children under 12 years of age at disease onset. J Pediatr Orthop 23: 590-600.
- Herring JA, Neustadt JB, Williams JJ, Early JS, Browne RH (1992) The lateral pillar classification of Legg-Calve-Perthes disease. J Pediatr Orthop 12: 143-150.
- Salter RB, Thompson GH (1984) Legg-Calve-Perthes disease. The prognostic significance of the subchondral fracture and a two-group classification of the femoral head involvement. J Bone Joint Surg Am 66: 479-489.
- Catterall A (1971) The natural history of perthe’s disease. JBJS 53: 37-53.
- Wiig O, Terjesen T, Svenningsen S (2008) Prognostic factors and outcome of treatment in perthes’ disease: A prospective study of 368 patients with five-year follow-up. J Bone Joint Surg Br 90: 1364-1371.
- Froberg L, Christensen F, Pedersen NW, Overgaard S (2011) Long-term follow-up of a patient cohort with Legg-Calvé-Perthes disease. J Pediatr Orthop B 20: 273-277.
- Herring JA, Kim HT, Browne R (2004) Legg-Calve-Perthes disease. Part I: Classification of radiographs with use of the modified lateral pillar and Stulberg classifications. J Bone Joint Surg Am 86: 2103-2120.
- Lee DS, Jung ST, Kim KH, Lee JJ (2009) Prognostic value of modified lateral pillar classification in Legg-Calvé-Perthes disease. Clin Orthop Surg 1: 222-229.
- Brech GC, Guarnieiro R (2006) Evaluation of physiotherapy in the treatment of Legg-Calvé-Perthes disease. Clinics (Sao Paulo) 61: 521-528.
- Westhoff B, Martiny F, Krauspe R (2013) [Current treatment strategies in Legg-Calvé-Perthes disease]. Orthopade 42: 1008-1017.
- Hefti F, Clarke NM (2007) The management of Legg-Calvé-Perthes’ disease: Is there a consensus? : A study of clinical practice preferred by the members of the European Paediatric Orthopaedic Society. J Child Orthop 1: 19-25.
- Pailhé R, Cavaignac E, Murgier J, Cahuzac JP, de Gauzy JS, Accadbled F (2016) Triple osteotomy of the pelvis for Legg-Calve-Perthes disease: A mean fifteen year follow-up. Int Orthop 40: 115-122.
- Rosello O, Solla F, Oborocianu I, Chau E, ElHayek T, et al. (2017) Advanced containment methods for Legg-Calvé-Perthes disease: Triple pelvic osteotomy versus Chiari osteotomy. Hip Int.
- Hefti F (2015) Kinderorthopädie in der Praxis. Springer Verlag, Berlin, Germany.
- Lee J, Allen M, Hugentobler K, Kovacs C, Monfreda J, et al. (2011) Conservative management of Legg- Calve-Perthes disease in children aged 3 to 12 years. Health Policy & Clinical Effectiveness Program, Guideline 39: 1-16.
- Manig M (2013) [Legg-Calvé-Perthes Disease (LCPD). Principles of diagnosis and treatment]. Orthopade 42: 891-902.
- http://www.leitliniensekretariat.de/files/MyLayout/pdf/Morbus_Perthes.pdf
Citation: Krieg AH, Schell RE, Neuhaus C (2018) Legg-Calvé-Perthes Disease and Its Physiotherapy - “If the Hip Melts Away”. J Orthop Res Physiother 4: 037.
Copyright: © 2018 Krieg AH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

