
Metastatic Fracture Femur in Subtrochanteric Region Misdiagnosed as Bisphosphonate Fracture - A Case Report of a Very Unusual Presentation of Metastatic Fracture Femur
*Corresponding Author(s):
Ashish Vinodkumar BatraDepartment Of Orthopedics, Pacific Medical College And Hospital, Udaipur, India
Email:drashishbatra.ortho@gmail.com
Abstract
There is a gradual increase in atypical subtrochanteric femur fractures which are related to bisphosphonate administration. Atypical femoral fractures are difficult to manage and need a great deal of care. AFF cases needed extra time for bone union than typical ones and persistent bisphosphonate administration led to a prolonged period of time required for bone union. We report a case of subtrochanteric femur fracture in a female patient that had been diagnosed with bisphosphonates related subtrochanteric fracture femur and later diagnosed with lung carcinoma with multiple metastatic lesions.
Keywords
Metastatic fracture; Subtrochanteric; Bisphosphonate fracture; Lung carcinoma; Misdiagnosed
Introductiion
Fractures in subtrochanteric region of femur are not so common (10-30% of all hip fractures) and majority of these are due to high velocity road traffic accidents. Subtrochanteric fractures reports to around 4% of all femoral fractures but the morbidity and mortality associated with these fractures are similar to other hip fractures [1,2].
Bisphosphonate (BP) is commonly used in the management of osteoporosis [1]. Whilst bisphosphonates have proved effective in this role, there is growing concern over their long-term use, with much evidence linking bisphosphonate-related suppression of bone remodeling to an increased risk of Atypical subtrochanteric Fractures of the Femur (AFFs).
Fractures of the subtrochanteric region are rare fractures and can happen without any high velocity trauma. Bones that are abnormal in elasticity and mineralization are prone to develop such fractures. The main mechanism of action of BPs is the hinderance in the natural remodeling and repair process of bone, and these insufficiency fractures are a consequence of build-up of these micro damages [2,3]. Metastatic lesions in the bone could present as pain in the zone of an impending insufficiency fractures.
Rising figure of AFF cases lately has encouraged further research of numerous potential causes of these fractures. Literature shows that AFFs are a known complication in patients taking Bisphosphonates for management of osteoporosis, this relationship has not yet been explored in similar depth as with cases with metastatic lesions in bone [4]. These types of AFFs could occur in both above cases [5].
In this report, we present a case of atypical femoral fractures in female patients that had been diagnosed with bisphosphonates related subtrochanteric fracture femur and later diagnosed with lung carcinoma with multiple metastatic lesions. Therefore, the aim of this case report is to highlight the specific concerns in this setting.
Case Report
A 76 years old lady tripped over a step in the backyard. She got up and managed to walk inside the house. After some time while getting something from the fridge, she turned around and her right hip suddenly gave way and she fell to the floor. She was unable to weight bear on her right leg after injury and had severe pain in hip.
On examination her right leg was shortened and externally rotated and she was not able to straighten leg raise, skin over right lower limb was absolutely normal. She was neurovascular intact in the right foot. X-rays show transverse sub trochanteric fracture femur with thickened cortices at the fracture site indicating it as a bisphosphonate fracture (Figure 1). She sustained an isolated closed injury to the right sub trochanteric region of the femur. She informed that she had pain in this hip for about a month before this injury and she had x-ray at that time, which was normal and didn’t show any bony lesion.
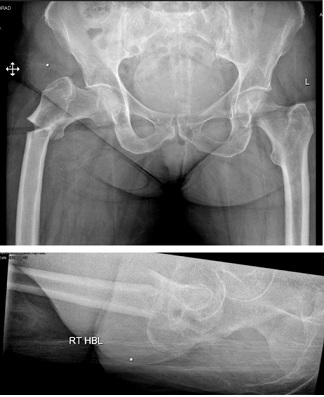 Figure 1: Image showing transverse Subtrochanteric Fracture Right Femur.
Figure 1: Image showing transverse Subtrochanteric Fracture Right Femur.
Her past medical history included osteoporosis, DVT and diverticular disease. She was taking Alendronate for the past 14 years without any holiday. Looking at her previous x-rays, about a month ago, it seems that she was developing an impending fracture over the lateral cortex which was thickened which is classic of bisphosphonate induced fractures (Figure 2).
 Figure 2: X-Ray Pelvis 1 month prior to sustaining the fracture showing thickening and sclerosed cortex.
Figure 2: X-Ray Pelvis 1 month prior to sustaining the fracture showing thickening and sclerosed cortex.
She underwent right femoral nailing, valgus osteotomy, & bone grafting next day. Intraoperatively, there was extremely screotic lateral cortex, very hypovasular bone, very unstable fracture pattern, and very dense cortices. It was decided to do open reduction because fracture was highly displaced. Fracture site was exposed using extended lateral transvastus approach. Even with open reduction, femur was still in unacceptable varus position so proceeded to do valgus proximal femoral osteotomy, and bone cuts & marrow were saved as graft. Reduction was held by applying temporary 6-hole LCP plate laterally (Figure 3), fracture stabilized to good position with 340x10mm 130deg TFNA and 95mm lag screw in neck and 2 bicortical distal locking screws (Figure 4). Fixation augmented with one cable placed just around the lesser trochanter (Figure 4) and bone graft applied. Post-operatively she was doing well and mobilizing comfortably with the help of zimmer frame. She was also referred to rheumatologist for ongoing bone health management given the complexity of her case. She was discharged from hospital around 2 weeks post-surgery.
 Figure 3: Intraoperative image showing use of plate to reduce the fracture and pass intramedullary nail.
Figure 3: Intraoperative image showing use of plate to reduce the fracture and pass intramedullary nail.
 Figure 4: Immediate post-operative image.
Figure 4: Immediate post-operative image.
She was followed up in clinic multiple times after her surgery and she was doing really well and was mobilizing full weight bearing. During her follow up X-rays there were encouraging signs of fracture union (Figure 5 and Figure 6). Dynamization of nail was done by removing the distal static locking screw to aid fracture union. Approximately, two and half months after her surgery, she developed shortness of breath and lethargy while she was at her home. She was seen by the medical team in emergency on that day, her CTPA was done which showed extensive mediastinal and subcarinal lymphadenopathy with hilar lymphadenopathy. Multiple soft tissue nodules throughout pulmonary parenchyma, there was no pulmonary embolism. Also, three discrete lumps were reported in left breast. CT Abdomen was also arranged which showed disseminated metastasis in liver, adrenals, peritoneum, bones, lymph nodes, breasts and likely pancreas. And CT Pelvis depicted multiple sclerotic metastasis within pelvis. It was suspected to be a malignant neoplasm of bronchus or lung. She underwent US guided biopsy of left breast nodule, which showed tiny cores of fibrofatty tissue showing a small cell carcinoma. Cells were positive for TTF1, CK7, Synaptophysin and Chromogranin and negative for GATA3 and ER, supporting the diagnosis. It was discussed in Lung MDT next day and concluded that this is likely metastasis from primary lung origin (Small Cell Lung Cancer TxN3M1c), although other primary sites cannot be excluded completely. Her performance status has failed to improve despite a week of steroids. It was decided in Lung MDT to give patient a best supportive care under palliative care team. Unfortunately, she died a month after diagnosis of metastatic lesions. Her initial imaging of the subtrochanteric fracture was not in keeping with a malignancy and there were no biopsies taken at that time.
 Figure 5: 6 weeks post operative image showing callus formation and signs of union.
Figure 5: 6 weeks post operative image showing callus formation and signs of union.
 Figure 6: 9 weeks post operative CT scan image during CT Abdomen and Pelvis.
Figure 6: 9 weeks post operative CT scan image during CT Abdomen and Pelvis.
Discussion
AFFs are defined as an oblique or transverse fracture pattern in the subtrochanteric region of femur. Most common mechanism of this is either a trivial trauma or it may develop spontaneously and frequently happens bilaterally. There could be some associated features such as prodromal thigh or groin pain, and thickening of femoral cortex [6].
It is recommended that a thorough assessment of patients with new onset of mid-thigh or groin pain and discomfort should be done for patients on bisphosphonates for more than 3 years. Most common diagnostic finding in X-rays is the endosteal and periosteal callus formation along with an oblique or transverse fracture at the lateral cortex in the subtrochanteric zone of the femur [6]. Further imaging by MRI may help in identifying fracture line through the cortex and any concomitant edema in bone and marrow of femur. Lucency or breach in the cortex and accompanying formation of new bone may be the finding on CT scan. Radionuclide bone scan has less specificity than MRI or CT but may detect focal bone and marrow hyperemia. If cortical lucency is found, the lesion could be considered an incomplete AFF but, if no lucency is seen but marrow edema is present, such lesions are described as stress reaction [6].
Regarding the mechanism of AFF formation, the appearance of them on imaging suggests that damage accumulates within the bone cortex over a long period and that AFFs are stress or insufficiency fractures. Long-term therapy with BPs can give rise to severe inhibition not only of osteoclastic activity but also of osteoblastic activity and a severe suppression of bone turnover. This protracted remodelling suppression leads to compromised bone quality [7,8]. At the same time, mineralization of the osteoid tissue continues resulting in increased brittleness of bone that makes it prone to fractures. This accumulation of abnormal bone tissue is thought to be the basis of atypical fracture pathogenesis. To our knowledge it has not been related, so far, to the existence of either lytic or blastic bone metastases but it should be noted that abnormal osteoblastic activity occurs in both types of metastases and may contribute to the AFF pathogenesis. Atypical femoral fractures have previously been reported in patients on high-dose bisphosphonate therapy for malignancy [9].
A study of AFF with high-dose bisphosphonate therapy for malignancy found a median duration of treatment of 6 years [10].
A study by shane et al described the criteria for an AFF according to the American Society of Bone and Mineral Research 2013 Task Force [11] and the fractures observed in our patients met these criteria, in that they were located within the femoral diaphysis and satisfied all 5 major criteria including: low-energy mechanisms, originating from the lateral cortex, involving both cortices, being generally non-comminuted, and showing localized periosteal or endosteal thickening of the lateral cortex.
Pathological fractures of the long bones are a common complication of bone metastases caused by various types of primary malignancies. The reported incidence of bone metastasis is up to 50% of all cancer patients [12]. Approximately 50% of primary malignant tumors may affect the skeleton, which is subsequently the third most frequent site of metastases after the lung and liver [13,14]. The reported incidence of bone metastases in breast, multiple myeloma, lung, prostate, and kidney cancers is up to 25% and 100% [12].
Small cell lung carcinoma can cause sclerotic or blastic metastases [15]. In our case report this patient was diagnosed with small cell lung carcinoma as primary few months after sustaining the subtrochanteric fracture. Taking the biopsy of reaming sample at the time of intramedullary nailing fixation could have helped either to rule out any metastatic lesion or to diagnose any pathological fracture and early diagnosis of primary carcinoma.
Conclusion
In conclusion, proper evaluation of patients to rule out any metastatic lesions related AFF must be done for patients who sustained subtrochanteric fracture femur with query bisphosphonate related. A MDT discussion with radiology and a pre-operative MRI of the entire fractured bone should be considered in all cases of atypical femoral fractures with no associated history of malignancy. Sending the bone marrow reaming material for biopsy at the time of surgery will be a very important initiative to rule out any sclerotic metastasis related subtrochanteric fracture as they sometimes mimic bisphosphonate related AFFs. There are few cancers such as lung Ca, Prostate Ca which can cause sclerotic meatstatic lesions, and they should be kept in mind while evaluating and BPs related AFFs. Metastatic lesion should be considered as a differential diagnosis in all cases of suspected bisphosphonate induced subtrochanteric femur fractures. Therefore, for patients receiving bisphosphonates as treatment for osteoporosis, we should must include awareness to recognize and rule out any metastatic lesion to better avoid any adverse event.
References
- Drake MMT, Clarke BL, Khosla S (2008) Bisphosphonates: Mechanism of action and role in clinical practice. Mayo Clin Proc 83: 1032-1045.
- Giannini S, Chiarello E, Tedesco G, Cadossi M, Luciani D, et al. (2013) Atypical femoral fractures. Clin Cases Miner Bone Metab 10: 30-33.
- Bush LA, Chew FS (2008) Subtrochanteric femoral insufficiency fracture following bisphosphonate therapy for osseous metastases. Radiol Case Rep 3: 232.
- Chang ST, Tenforde AS, Grimsrud CD, O’Ryan FS, Gonzoledronatelez JR, et al. (2012) Atypical femur fractures among breast cancer and multiple myeloma patients receiving intravenous bisphosphonate therapy. Bone 51: 524-527.
- Kharazmi M, Hallberg P, Michaëlsson K (2014) Gender related difference in the risk of bisphosphonate associated atypical femoral fracture and osteonecrosis of the jaw. Ann Rheum Dis 73: 1594.
- Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, et al. (2014) Atypical Subtrochanteric and Diaphyseal Femoral Fractures: Second Report of a Task Force of the American Society for Bone and Mineral Research. J Bone Miner Res 29: 1-23.
- Mashiba T, Hirano T, Turner C, Forwood M, Johnston C, et al. (2000) Suppressed bone turnover by bisphosphonates increases microdamage accumulation and reduces some biomechanical properties in dog rib. J Bone Miner Res 15: 613-620.
- Ettinger B, Burr DB, Ritchie RO (2013) Proposed pathogenesis for atypical femoral fractures: lessons from materials research. Bone 55: 495-500.
- Puhaindran ME, Farooki A, Steensma MR, Hameed M, Healey JH, et al. (2011) Atypical subtrochanteric femoral fractures in patients with skeletal malignant involvement treated with intravenous bisphosphonates. J Bone Joint Surg Am 93: 1235-1242.
- Chang ST, Tenforde AS, Grimsrud CD, O’Ryan FS, Gonzalez JR, et al. (2012) Atypical femur fractures among breast cancer and multiple myeloma patients receiving intravenous bisphosphonate therapy. Bone 51: 524-527.
- Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, et al. (2014) Atypical subtrochanteric and diaphyseal femoral fractures: Second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 29: 1-23.
- Landis SH, Murray T, Bolden S, Wingo PA (1998) Cancer statistics. 1998. CA Cancer J Clin 48: 6-29.
- Hage WD, Aboulafia AJ, Aboulafia DM (2000) Incidence, location, and diagnostic evaluation of metastatic bone disease. Orthop Clin North Am 31: 515-528.
- Coleman RE (1997) Skeletal complications of malignancy. Cancer 80: 1588-1594.
- Macedo F, Ladeira K, Pinho F, Saraiva N, Bonito N, et al. (2017) Bone Metastases: An Overview. Oncol Rev 11: 321
Citation: Batra AV (2022) Metastatic Fracture Femur in Subtrochanteric Region Misdiagnosed as Bisphosphonate Fracture - A Case Report of a Very Unusual Presentation of Metastatic Fracture Femur. J Orthop Res Physiother 8: 058
Copyright: © 2022 Ashish Vinodkumar Batra, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

