Mucoepidermoid Carcinoma of the Eyelid: A Rare Presentation
*Corresponding Author(s):
Kafil AkhtarDepartment Of Pathology, Aligarh Muslim University, Jawaharlal Nehru Medical College, Aligarh, India
Tel:+91 05712721191,
Email:drkafilakhtar@gmail.com
Abstract
Purpose: Mucoepidermoid Carcinoma (MEC) of the skin is an exceedingly rare neoplasm. It is similar to MEC of the salivary gland, a neoplasm whose prognosis is correlated with the pathologic grade. Some confusion exists as to whether MEC is synonymous with adenosquamous carcinoma of the skin. The latter tumor type is a squamous and gland-forming neoplasm with intermediate- to high-grade features rather than a tumor with mucigenic cells intermingled among intermediate and squamous cells.
Methods: We report a case of MEC of the eyelid skin in a 79-year-old woman who presented with a soft to cystic mass on the left upper eyelid.
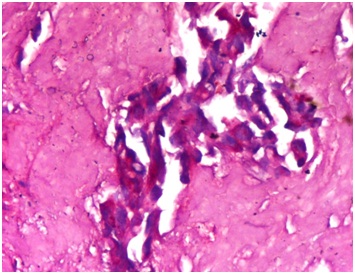
Results: Microscopically it was characterized by a circumscribed, cystic neoplasm, with vague lobules of low-grade-appearing squamous cells accompanied by mucigenic and clear cells. A mucin stain highlighted the PAS positive mucigenic cells. Immunohistochemistry revealed pan-cytokeratin, cytokeratin 7, polyclonal carcinoembryonic antigen and epithelial membrane antigen positivity. The cytokeratin 20 and gross cystic disease fluid protein were nonreactive.
Conclusion: Since the primary cutaneous mucoepidermoid carcinoma is an aggressive neoplasm that frequently develops metastases, it is important to distinguish it from primary MEC originating from the salivary glands for better management and suitable therapeutic decisions.
Keywords
Eyelid; Histopathology; Immunohistochemistry; Mucoepidermoid carcinoma; Mucin
INTRODUCTION
Mucoepidermoid Carcinoma (MEC) is a common tumor of the salivary gland. It also occurs in other sites such as the paranasal sinuses, lung, axilla, finger, scalp and eyelid. Both primary MEC and metastasis from the salivary glands may also be found in the conjunctiva and the lacrimal sac. But it is exceedingly rare in the skin, with few reported cases arising within a nevus sebaceus of Jadassohn [1,2].
MEC is common in the major and minor salivary glands, accounting for approximately 30% of all malignant tumors arising from these glands [3]. Cutaneous involvement should be carefully assessed to exclude the possibility of metastases from distant sites. It has to be differentiated from adenosquamous carcinoma, which is a high-grade neoplasm with poorer outcome and metastasis from a primary MEC arising elsewhere in the body [2,3].
Treatment of MEC is complete surgical excision, using Mohs technique if necessary [4]. Local recurrences may occur after incomplete removal. We report a case of a primary cutaneous mucoepidermoid carcinoma, who presented with left upper eyelid mass.
CASE SUMMARY
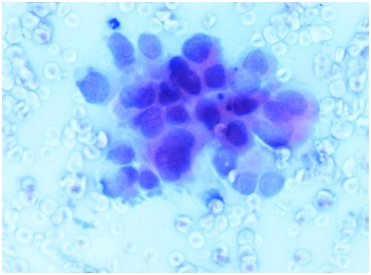
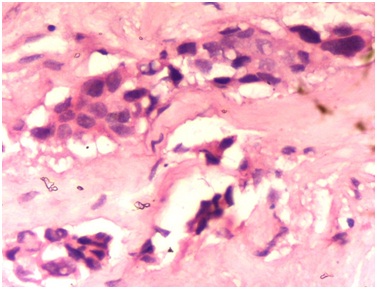
A 79 year-old woman presented to the Ophthalmology clinics with a progressively growing mass on the left upper eyelid with ulcerated skin for the last 2 months. Physical examination showed an erythematous, well defined, ulcerated nodule on his left upper eyelid of size 2 x 2 cm (Figure 1). No systemic symptoms were found but only cervical lymphadenopathy was present. Fine needle aspiration cytology revealed a necrotic and mucinous background with few dispersed atypical cells, suggestive of malignancy (Figure 2). The mass was excised and grossly, showed a well encapsulated, grey, soft to cystic and mucoid tissue of 2.5 × 2.0 cm in size (Figure 3).
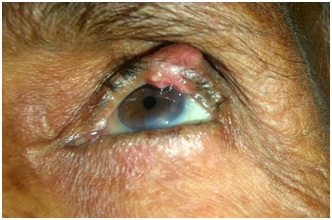
Figure 1: Physical examination showed an erythematous, well defined and ulcerated nodule on his left upper eyelid of size 2 x 2 cm.
Figure 2: The excised mass grossly showed a well encapsulated, grey, soft to cystic and mucoid tissue of 2.5 × 2.0 cm in size.
DISCUSSION
Mucoepidermoid Carcinoma (MEC) is a relatively common neoplasm. Primary MEC accounts for approximately 30% of all malignant tumors arising in major and minor salivary glands [1,2]. MEC was established as a unique salivary gland tumor in 1945 by Stewart et al., [4,5]. It most commonly affects the salivary glands, especially the parotid but also submandibular and minor salivary glands. MEC is also found in the lacrimal gland, with an incidence of approximately 1.5- 4% [3,4]. It may rarely be reported in the esophagus, lung, bronchi, trachea, breast, thymus, thyroid, pancreas and female genital tract [3,5-7]. Cutaneous involvement as a primary origin is extremely rare, with only 11 cases reported in the medical literature [4,5].
The lesion is often well circumscribed and partly cystic. It is deep in location and not attached to the epidermis [5]. The tumor is composed of three cell types: mucinous, squamous and clear. The squamous cells are in lobules and the mucigenic and clear cells are admixed [4]. Periodic Acid-Schiff stain highlights the mucigenic cells. Histologically MEC can be divided into low-grade (well-differentiated) and high-grade (poorly differentiated) subtypes, although an intermediate grade has also been proposed. Also three groups have been described based on the proportion of mucin-secreting, squamous, intermediate and clear cells and the degree of maturation of these cells [3,7].
MEC is often used synonymously with Adenosquamous Carcinoma (ASC). But ASC and its clinical behavior is quite different from MEC, especially in the case of a low-grade MEC, whether in the salivary gland or the skin [8,9]. MEC is usually a low-grade neoplasm with limited metastatic potential, whereas Adenosquamous Carcinoma (ASC) is a high grade neoplasm prone to local recurrence and metastatic dissemination [9,10].
Quintas et al., performed two local excisions with adjuvant cryotherapy and mitomycin C application in their case of mucoepidermoid carcinoma of the bulbar conjunctiva over a period of 6 months [11]. Siuw et al., performed adjuvant radiotherapy in a case of secondary mucoepidermoid carcinoma of the orbit [12].
Immunohistochemically, mucoepidermoid carcinomas are positive for CK7, Pan CK, EMA and CEA and negative for CK20 and anti-human gross cystic disease fluid protein [13,14]. Primary mucoepidermoid carcinoma of the orbit is rare and typically arises from the lacrimal gland or sac. Those tumors not arising from lacrimal apparatus should be presumed metastatic in origin and the thorough systemic survey should be undertaken in the search for the primary tumor [12]. Rare cases of cutaneous metastasis of MEC originating from different sites, like the bronchi should be taken into account [3]. Yadav et al., reported a case of an exophytic lesion of the left bulbar conjunctiva following treatment for high grade mucoepidermoid cancer of ipsilateral parotid gland, 9 months back [15]. For this reason a careful evaluation of the patients to look for occult neoplasms in distant sites needs to be done. It is recommended to perform blood chemistry profile, complete blood count together with diagnostic imaging like total body Positron Emission Tomography and Computed Tomography Scan and p63 immunostaining to differentiate cutaneous metastasis from primary MEC [10,15,16].
CONCLUSION
Primary MEC of the skin is usually a slow-growing neoplasm that should be differentiated from adenosquamous carcinoma and immunohistochemical staining for p63 is helpful to differentiate primary and metastatic MEC in the skin.
REFERENCES
- Azorín D, López-Ríos F, Ballestín C, Barrientos N, Rodríguez-Peralto JL (2001) Primary cutaneous adenosquamous carcinoma: a case report and review of the literature. J Cutan Pathol 28: 542-545.
- Suárez-Peñaranda JM, Vieites B, Valeiras E, Varela-Duran J (2010) Primary mucoepidermoid carcinoma of the skin expressing p63. Am J Dermatopathol 32: 61-64.
- Riedlinger WF, Hurley MY, Dehner LP, Lind AC (2005) Mucoepidermoid carcinoma of the skin: a distinct entity from adenosquamous carcinoma: a case study with a review of the literature. Am J Surg Pathol 29: 131-135.
- Nouri K, Trent JT, Lowell B, Vaitla R, Jimenez GP (2003) Mucoepidermoid carcinoma (adenosquamous carcinoma) treated with Mohs micrographic surgery. Int J Dermatol 42: 957-959.
- Pia-Foschini M, Reis-Filho JS, Eusebi V, Lakhani SR (2003) Salivary gland-like tumours of the breast: surgical and molecular pathology. J Clin Pathol 56: 497-506.
- Hattori H (2003) Goblet cell predominant high-grade mucoepidermoid carcinoma of the index finger. Br J Dermatol 149: 1091-1092.
- Berk DR, Lennerz JK, Bayliss SJ, Lind A, White FV, et al. (2007) Mucoepidermoid carcinoma on the scalp of a child. Pediatr Dermatol 24: 452-453.
- Diwan AH, Smith KJ, Brown R, Skelton HG (2003) Mucoepidermoid carcinoma arising within nevus sebaceus of Jadassohn. J Cutan Pathol 30: 652-655.
- Moloney TP, Trinh T, Farrah JJ (2014) A case of conjunctival mucoepidermoid carcinoma in Australia. Clin Ophthalmol 8: 11-14.
- Farley JH, Hickey KW, Carlson JW, Rose GS, Kost ER, et al. (2003) Adenosquamous histology predicts a poor outcome for patients with advanced-stage, but not early-stage, cervical carcinoma. Cancer 97: 2196-2202.
- Quintas AM, Fonseca AC, Crujo C, Almeida L, Monteiro-Grillo M (2011) Mucoepidermoid carcinoma of the bulbar conjunctiva – an interventional case report. GMS Ophthalmol Cases 1: Doc06.
- Siuw CP, Tan SW, Abdul Wahid AB, Vasudevan S (2016) Secondary mucoepidermoid carcinoma of the orbit. Indian J Ophthalmol 64: 238-241.
- Ivan D, Hafeez Diwan A, Prieto VG (2005) Expression of p63 in primary cutaneous adnexal neoplasms and 12. adenocarcinoma metastatic to the skin. Mod Pathol 18: 137-142.
- Ivan D, Nash JW, Prieto VG, Calonje E, Lyle S, et al. (2007) Use of p63 expression in distinguishing primary and metastatic cutaneous adnexal neoplasms from metastatic adenocarcinoma to skin. J Cutan Pathol 34: 474-480.
- Yadav R, Battoo AJ, Mir AW, Haji AG (2017) Bulbar conjunctival metastasis from mucoepidermoid carcinoma of parotid-a case report and review of literature.World J Surg Oncol 15: 10.
- López V, Rubio M, Santonja N, Jordá E (2010) Primary cutaneous mucoepidermoid carcinoma. Am J Dermatopathol 32: 618-620.
Citation: Akhtar K, Waris A, Rizvi SAR (2017) Mucoepidermoid Carcinoma of the Eyelid: A Rare Presentation. J Infect Non Infect Dis 3: 020.
Copyright: © 2017 Kafil Akhtar, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.