
Multifocal Osteomyelitis in a Neonate, an Overview of Diagnosis and Treatment
*Corresponding Author(s):
Somford MPDepartment Of Orthopedic Surgery, Medisch Spectrum Twente, Enschede, Netherlands
Tel:+31 624881380,
Email:Mp_Somford@hotmail.com
Abstract
We present a case of multifocal osteomyelitis and septic arthritis in a 26 weeks premature neonate. A female newborn child presented with sepsis-like illness systemically as well as multiple swelling of the bones and joints. After clinical suspicion of osteomyelitis, the diagnosis was made with the help of blood culture and imaging studies such as ultrasound, plain radiographs and MRI. The child underwent multiple surgeries for drainage of the abscesses and infected joints. Sensitive antibiotics were continued perioperative as well as postoperative for 6 weeks after the last surgery. Inflammatory marker and MRI were used to follow prognosis. The child recovered well without notable short term sequellae at 18 months follow up.
Keywords
INTRODUCTION
CASE REPORT
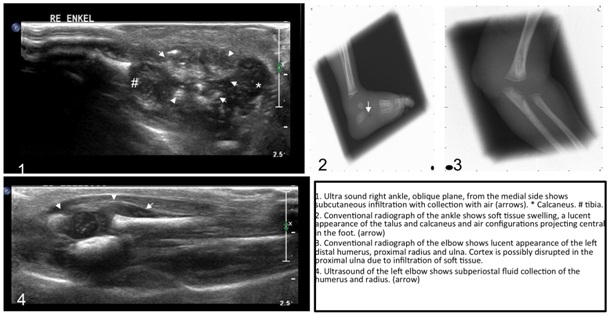
Figure 1: Ultra sound right ankle, oblique plane, from the medial side shows subcutaneous infiltration with collection with air (arrows) * - calcaneus, # - tibia.
2 - Conventional radiograph of the ankle shows soft tissue swelling, a lucent aspect of the talus and calcaneus and air configurations projecting central in the foot (arrow).
3 - Conventional radiograph of the elbow shows lucent aspect of the left humerus, proximal radius and ulna. Cortex is possibly disrupted in the proximal ulna due to infiltration of soft tissue.
4 - Ultrasound of the left elbow shows subperiostal fluid collection of the humerus and radius (arrow).
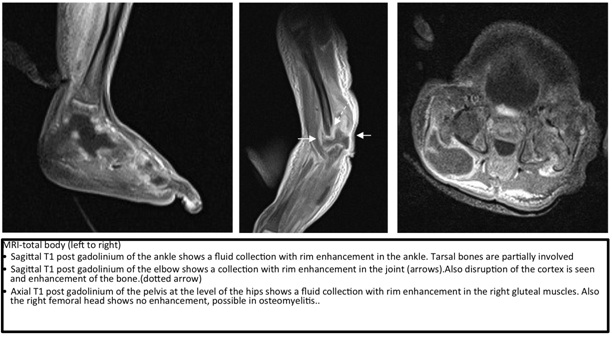
Sagittal T1 post gadolinium of the elbow shows a collection with rim enhancement in the joint (arrows). Also disruption of the cortex is seen and enhancement of the bone (dotted arrow).
Axial T1 post gadolinium of the pelvis at the level of the hips shows a fluid collection with rim enhancement in the right gluteal muscles. Also the right femoral head shows no enhancement, possible in osteomyelitis.
DISCUSSION
CLINICAL SIGNS AND PATHOGENESIS
Staphylococcus aureus is a prominent pathogen in neonatal septicemia and carries a high risk of developing deep-seated infections such as OM [4]. Other commonly found pathogens are Streptococcus agalactiae, Escheria coli, Klebsiella and Enterobacter [1].
Multifocal OM is more frequently seen in neonates compared to older children during childhood and has been reported in 20-50% of all neonates with OM foci [2]. Lower extremities are significantly more often involved [5]. Localization of OM in neonates differs from older children due to a different blood supply to the bone of the neonate. The metaphysical vessels communicate with the epiphysial vessels of the cartilaginous precursor of the ossific nucleus. This facilitates a rapid spread of infections from the metaphysis to the epiphysis, which is often destroyed in the infection. This explains why in neonates arthritis and osteomyelitis co-exist [6]. Premature babies have an underdeveloped haemato-lymphoreticular system, which is required for fighting bacteremia. That might be the reason why bacteremia leads subsequently relatively easy to septic arthritis and osteomyelitis. The incidence in newborns is low (0.5% of all neonatal admissions), especially among preterms [7]. Cases are described in term and late preterm newborns with presentation of symptoms from 2-53 days. Prematurity herein is not clearly defined. As far as we know, the case presented is the youngest patient in literature presenting with a multifocal OM [8].
A noteworthy in the presenting case is the relapse multifocal osteomyelitis and arthritides without positive pus cultures for the original pathogen, Staphylococcus aureus, of infection. Furthermore no pathogen was found. A clear notification for this phenomenon is not found. The diagnosis Chronic Recurrent Multifocal Osteomyelitis (CRMO) could be considered. CRMO is a chronic recurrent multifocal osteomyelitis of unknown noninfectious etiology [9]. Differs microorganisms including Staphylococci, Streptococci, Mycoplasma as well autoimmune process has been suggested but not yet confirmed. CRMO affects metaphysis of the long bones, pelvis, clavicle and mandible. Radiology X-ray and MRI can show similarities to a bacterial osteomyelitis [9]. Bone pains are usually the man symptoms; however this was difficult to report in our case of the premature neonate [10]. Increase of inflammatory markers can be seen in 66% of the case [11]. Though this phenomena is rare and mainly effects children in the age of 4-14 years [9].
DIAGNOSIS
Radiology plays an important role in the early detection and treatment of OM. Usually conventional imaging is the first modality of choice. Conventional imaging may show early signs of osteomyelitis, but early signs of bone destruction may not be evident on X-ray until about 10 days after onset of symptoms. Thus, a normal x-ray cannot be used to exclude OM in the first 10 days after onset of symptoms. In young children, ultrasound is a useful modality to combine physical exam with radiologic findings. Ultrasound has a high sensitivity in detection of infiltration of soft tissue, (subperiosteal) abscess formation, fistulas or fluid in a joint early in the process. Disruption of the bone cortex can be seen. The main drawback of ultrasound is that bone marrow cannot be imaged reliably. MR has an important role in the detection of acute osteomyelitis. It has a high sensitivity for detection and allows imaging of bone marrow, soft tissue, subperiosteal and articular collections. Additionally, complications of osteomyelitis like abscess formation or arthritis can be seen on MR. The main drawback of MR is the long time of scanning, requiring immobilization of the patient. However, children of this age group can be fixated without requiring anesthesia per se. Swaddling after feeding often is enough. CT plays a limited role in the detection of OM. CT can be used to detect complications of osteomyelitis, such as sequester. The main drawback of CT is the high radiation dose and soft tissues are not well analyzed [13].
TREATMENT
Sequential parenteral-oral therapy may be used with close follow up. Shorter duration of parenteral therapy follow by oral therapy based on good clinical response was not associated with recurrence of infection [15]. If the clinical response to therapy is satisfactory, antibiotics can be continued orally. However no specific evidence based recommendations can be made and no specific time markers are described in the literature [1,16]. Peltola et al., propose a shorter treatment in patients older than 3 months [15]. Shorter duration of parenteral therapy followed by oral therapy based on good clinical response was not associated with recurrence of infection [12]. Since few reports of OM in newborns and premature newborns have been published no specific guidelines are available for premature babies suffering from multifocal osteomyelitis [15,16]. In the presented case, the antibiotic regime was continued for 6 weeks after the last increase of swelling and infection parameters in blood.
Surgical decompression and debridement was conducted in the presented case because of the presence of abscesses and multifocal septic arthritis and osteomyelitis. MR showed to be of significant value for pre-operative planning. Pre-operative localization of intra osseous abscesses was seen in advance and resulted in adequate drainage and shorter surgery time. Deshpande et al., reviewed 15 causes of neonatal septic arthritis and advised immediate arthrotomy to drain pus from the joint in case of strong clinical suspicion, instead of waiting 72 h. This resulted in a better long-term outcome with less functional sequellae [7].
LONG TERM FOLLOW-UP
CONCLUSION
REFERENCES
- Goldmann DA, Durbin WA Jr, Freeman J (1981) Nosocomial infections in a neonatal intensive care unit. J Infect Dis 144: 449-459.
- Frederiksen B, Christiansen P, Knudsen FU (1993) Acute osteomyelitis and septic arthritis in the neonate, risk factors and outcome. Eur J Pediatr 152: 577-580.
- Yagupsky P, Bar-Ziv Y, Howard CB, Dagan R (1995) Epidemiology, etiology, and clinical features of septic arthritis in children younger than 24 months. Arch Pediatr Adolesc Med 149: 537-540.
- Ross AC, Toltzis P, O’Riordan MA, Millstein L, Sands T, et al. (2008) Frequency and risk factors for deep focus of infection in children with Staphylococcus aureus bacteremia. Pediatr Infect Dis J 27: 396-399.
- Al Saadi MM, Al Zamil FA, Bokhary NA, Al Shamsan LA, Al Alola SA, et al. (2009) Acute septic arthritis in children. Pediatr Int 51: 377-380.
- Ogden JA (1979) Pediatric osteomyelitis and septic arthritis: the pathology of neonatal disease. Yale J Biol Med 52: 423-448.
- Deshpande SS, Taral N, Modi N, Singrakhia M (2004) Changing epidemiology of neonatal septic arthritis. J Orthop Surg (Hong Kong) 12: 10-13.
- Berberian G, Firpo V, Soto A, Lopez Mañan J, Torroija C, et al. (2010) Osteoarthritis in the neonate: risk factors and outcome. Braz J Infect Dis 14: 413-418.
- Aygun D, Barut K, Camcioglu Y, Kasapcopur O (2015) Chronic recurrent multifocal osteomyelitis: a rare skeletal disorder. BMJ Case Reports.
- Catalano-Pons C, Comte A, Wipff J, Quartier P, Faye A, et al. (2008) Clinical outcome in children with chronic recurrent multifocal osteomyelitis. Rheumatology (Oxford) 47: 1397-1399.
- Brown T, Wilkinson RH (1988) Chronic recurrent multifocal osteomyelitis. Radiology 166: 493-496.
- McPherson DM (2002) Osteomyelitis in the neonate. Neonatal Netw 21: 9-22.
- van Schuppen J, van Doorn MM, van Rijn RR (2012) Childhood osteomyelitis: imaging characteristics. Insights Imaging 3: 519-533.
- Korakaki E, Aligizakis A, Manoura A, Hatzidaki E, Saitakis E, et al. (2007) Methicillin-resistant Staphylococcus aureus osteomyelitis and septic arthritis in neonates: diagnosis and management. Jpn J Infect Dis 60: 129-131.
- Peltola H, Pääkkönen M, Kallio P, Kallio MJ, Osteomyelitis-Septic Arthritis (OM-SA) Study Group (2009) Prospective, randomized trial of 10 days versus 30 days of antimicrobial treatment, including a short-term course of parenteral therapy, for childhood septic arthritis. Clin Infect Dis 48: 1201-1210.
- Caramia G, Ruffini E, Zaffanaello M, Fanos V (2007) Acute bone and joint infections in children and therapeutic options. J Pediatr Infect Dis 2: 193-203.
- Vazquez M (2002) Osteomyelitis in children. Curr Opin Pediatr 14: 112-115.
Citation: Somford MP, Huibers MHW, Schuppen J, Struijs PAA, van Lee R (2015) Multifocal Osteomyelitis in a Neonate, an Overview of Diagnosis and Treatment. J Orthop Res Physiother 2: 015.
Copyright: © 2015 Somford MP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

