Multimorbidity and Polypharmacy do not influence the Self-Perception of Health among the very Elderly: A Cross-Sectional Study
*Corresponding Author(s):
Vicente Paulo AlvesResearcher And Professor In The Stricto Sensu Graduate Program In Gerontology Of The Catholic Univer, Federal District, 71966-700, Brazil
Email:vicerap@gmail.com
Abstract
The manuscript intends to investigate if multimorbidity (≥2 chronic diseases) and polypharmacy (≥5 drugs) influence the health self-perception in oldest-old people (≥80 years). A sample of 190 outpatients was submitted to a medical consult and application of questionnaires, to assess clinical and sociodemographic characteristics, self-reported diseases and medication use. We also measured the self-perception of current health (good/very good, regular, or poor/very poor), the relative self-perception of health compared to the previous year and to age-matched individuals (better, equal or worse). Chi-square test was used for comparison, p-value of ≤0.05 was considered significant. Self-perception of health was reported as positive by 42%, regular by 51% and poor/very poor by 7% of the participants. When compared to others of the same age, 66% considered their health to be better. A decreased positive self-perception of health was observed when own health was compared to the prior year. The presence of multimorbidity or polypharmacy did not influence the self-perception of health. The use of health self-perception metrics and should be considered in the elaboration of strategies for a more positive self-rated of aging, even in the presence of multimorbidity and polypharmacy.
Introduction
The increase in life expectancy is a global challenge. The number of Brazilians aged ≥60 years surpassed 30 million in 2017, with a 19% increase in the last 5 years [1]. The number ofvery elderly people aged >80 years has been growing at a rate higher than the growth rate of the total Brazilian very elderly population [2].
Population longevity has contributed to an increase in the incidence of chronic diseases, either in isolation or combined, which are a serious public health problem [3]. Consequently, the concept of multimorbidity was created, which is defined by the European General Practice Research Network [4] as any combination of a chronic disease with at least one other disease (either acute or chronic), biopsychosocial factors (either associated or not), or somatic risk factors.
Because very elderly people have one or more chronic diseases, the majority of them are prone to polypharmacy, which is defined as the concurrent use of five or more drugs [5].
Are multimorbidity and polypharmacy independent variables in the self-perception of health among the very elderly?
Self-perception of health and aging is a measure of the subjective judgment that each individual makes about his/her physical and mental health on the basis of his/her own criteria and beliefs [6] and in which the individual himself/herself has a decisive role [7]. Health perceived through subjective rating can be used as a predictor of morbidity [8], disability [9], and mortality [10].
Research conducted with people of very advanced age, including centenarians, has shown that a positive self-rating, even when multimorbidity and functional dependence are present, is associated with the perception of successful aging [11-13]. The objective of the present study was to investigate whether multimorbidity and polypharmacy influence the self-perception of health among very elderly Brazilian individuals.
Materials and Methods
This was an analytical, observational, descriptive, qualitative cross-sectional study. This research was part of the multicenter project National Program of Academic Cooperation, funded by the Coordination of Superior Level Staff Improvement (CAPES), aimed at studying the morphological and physiological changes related to longevity in very elderly people aged ≥80 years using an interdisciplinary approach. It was submitted to and approved by the Research Ethics Committee (CEP) of the Catholic University of Brasília (CAAE no. 50075215.2.0000.0029) under opinion no. 1.290.368. The participants were informed about the objective of the study and the voluntary nature of their participation. They, or their authorized representatives, signed a Term of Free and Informed Consent.
Very elderly patients were assessed in the outpatient facilities of the Hospital of the Catholic University of Brasília, administrated by the Taguatinga Unit of the Federal District Institute of Cardiology. The participants underwent medical evaluation to obtain the most relevant information about their health status, namely through tests and questionnaires.
The study included 190 very elderly individuals (70 men and 120 women) recruited from a group of very elderly patients (n = 223) receiving geriatric medical care at the institution. Those who were aged ≥80 years and were able to understand and answer the survey instruments were invited to participate in the study, which was conducted between March 2016 and May 2018. Individuals were excluded from the study if they were unable to answer the questionnaires after cognitive function screening using the Mini-Mental State Examination [14] appropriate for their schooling level, if they died during the study period, if they refused to participate in subsequent stages of the study, and if they had no means of transportation to the sites where they would be assessed by a multiprofessional team.
Data collection was performed within 1 h during each encounter to avoid long fasting periods or changes in medication intake times.
An outpatient assessment was performed by a multidisciplinary team to collect information on: I. Morbidities: heart diseases, hypertension, stroke, diabetes mellitus, cancer, arthritis/rheumatism, lung diseases, depression, and osteoporosis (Annex A); II. Use of medications/polypharmacy (Annex A); III. Sociodemographic variables (Annex B); IV. Self-perception of health assessed using three questions: 1. How the very elderly person rates his/her health at the present moment (very good/good, fair, or poor/very poor); 2. How the very elderly person compares his/her health with that of other individuals of the same age (better, same, or worse); and 3. How the very elderly person compares his/her current health status with that in the previous year (better, same, or worse) (Annex C).
Statistical Analysis
Data analysis was performed through the calculation of the proportions of categorical variables. The sample was divided into three groups according to health self-perception: 1. Positive for those who perceived their health as very good/good (n = 79); 2. Fair for those who perceived it as fair (n = 97); 3. Negative for those who perceived it as very poor/poor (n = 14).
The comparison of the self-ratings according to the demographic and clinical variables (sex, age group, schooling, family income, polypharmacy, and multimorbidity) was performed using Fisher’s exact chi-square test. Significance level was set at p ≤ 0.05. All analyses were performed using IBM Statistical Package for the Social Sciences software, version 22.0.
Results
In the present study, 190 very elderly patients with a mean age of 84.62 ± 4.29 years (range, 80–101 years) were assessed; the majority of them were women (63.2%), as shown in table 1.
|
Variables |
Number |
% |
|
Total |
190 |
100.0 |
|
Sex |
|
|
|
Male |
70 |
36.8 |
|
Female |
120 |
63.2 |
|
Age group (years) |
|
|
|
80 to 84 |
109 |
57.4 |
|
≥85 |
81 |
42.6 |
|
Schooling (years)† |
|
|
|
Never went to school |
49 |
25.8 |
|
1 to 4 |
79 |
41.6 |
|
≥5 |
58 |
30.5 |
|
Family income |
|
|
|
Up to 1.0 m.w. |
23 |
12.1 |
|
1.1 to 3.0 m.w. |
76 |
40.0 |
|
≥3.0 m.w. |
91 |
47.9 |
|
Polypharmacy‡ |
|
|
|
Yes |
77 |
40.5 |
|
No |
83 |
43.7 |
|
Multimorbidity§ |
|
|
|
Yes |
84 |
44.2 |
|
No |
80 |
42.1 |
Table 1: Study of aging patterns among elderly outpatients living in different contexts Notes: M.W. = minimum wages(s); †4 patients had no data on schooling; ‡30 patients had no data on polypharmacy; §26 patients had no data on multimorbidity.
The individuals who reported using more than five medications accounted for 40.5% of the sample. The reported number of prescribed medications varied from 1 to 17, with a median of 4 and an interquartile range of 5 (Q3 = 7 and Q1 = 2).
Regarding multimorbidity, 44.2% of the individuals had two or more diseases (Table 1), with the most prevalent being hypertension (80.9%), followed by osteoporosis (41.8%), diabetes (31.2%), arthritis/rheumatism (29.2%), depression (29%), heart diseases (22.8%), cancer (18.3%), lung diseases (14.8%), and stroke (13.2%). The number of chronic diseases ranged from 0 to 9, with a median of 2.0 and an interquartile range of 1.75 (Q3 = 3.00 and Q1 = 1.25).
According to the subjective self-rating of the current health status, the majority of the assessed individuals (51%) self-rated their health as fair, 42% rated it as positive, and a mere 7% rated it as negative (Figure 1).
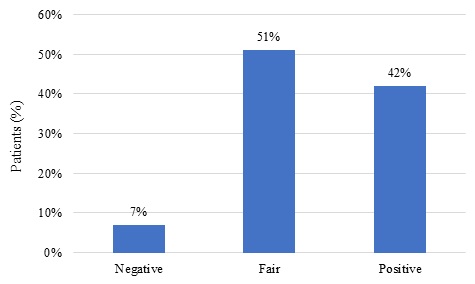 Figure 1: Distribution of subjective self-rating of the current health status. Brasília, 2016/2018.
Figure 1: Distribution of subjective self-rating of the current health status. Brasília, 2016/2018.
A comparison of the subjective self-rating of the current health status according to the sociodemographic and clinical variables showed that there were no significant differences in the proportions according to sex (p = 0.087), age group (p = 0.728), schooling (p = 0.087), family income (p = 0.251), polypharmacy (p = 0.061), and multimorbidity (p = 0.318), as shown in table 2.
|
Variables |
Negative |
Fair |
Positive |
p-value* |
|||
|
nº |
% |
nº |
% |
nº |
% |
||
|
Total |
14 |
100.0 |
97 |
100.0 |
79 |
100.0 |
- |
|
Sex |
|
|
|
|
|
|
|
|
Male |
3 |
21.4 |
31 |
32.0 |
36 |
45.6 |
0.087 |
|
Female |
11 |
78.6 |
66 |
68.0 |
43 |
54.4 |
|
|
Age group (years) |
|
|
|
|
|
|
|
|
80 to 84 |
7 |
50.0 |
58 |
59.8 |
44 |
55.7 |
0.728 |
|
≥85 |
7 |
50.0 |
39 |
40.2 |
35 |
44.3 |
|
|
Schooling (years) |
|
|
|
|
|
|
|
|
Never went to school |
5 |
35.7 |
27 |
27.8 |
17 |
21.5 |
0.087 |
|
1 to 4 |
5 |
35.7 |
47 |
48.5 |
27 |
34.2 |
|
|
≥5 |
4 |
28.6 |
22 |
22.7 |
32 |
40.5 |
|
|
Family income |
|
|
|
|
|
|
|
|
Up to 1.0 m.w. |
1 |
7.1 |
15 |
15.5 |
7 |
8.9 |
0.251 |
|
1.1 to 3.0 m.w. |
9 |
64.3 |
37 |
38.1 |
30 |
38.0 |
|
|
≥3.0 m.w. |
4 |
28.6 |
45 |
46.4 |
42 |
53.2 |
|
|
Polypharmacy |
|
|
|
|
|
|
|
|
Yes |
8 |
57.1 |
43 |
44.3 |
26 |
32.9 |
0.061 |
|
No |
3 |
21.4 |
39 |
40.2 |
41 |
51.9 |
|
|
Multimorbidity |
|
|
|
|
|
|
|
|
Yes |
5 |
35.7 |
39 |
40.2 |
40 |
50.6 |
0.318 |
|
No |
7 |
50.0 |
44 |
45.4 |
29 |
36.7 |
|
Table 2: Study of aging patterns among elderly outpatients living in different contexts
Note: *p-value calculated using the chi-square test, excluding patients without data
A comparison of the participants’ self-rating of health with rating the health of other people of same age showed that the majority (65.6%) self-rated their health as better and 6.5% rated it as worse than that of the others (Figure 2).
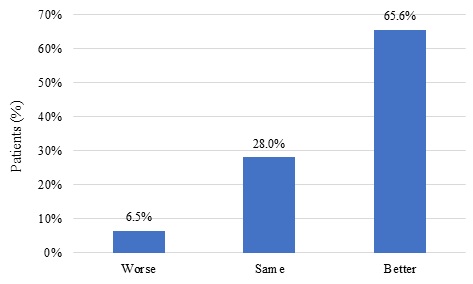 Figure 2: Distribution of subjective self-rating of health when compared with the health of other people of the same age, Brasília, 2016/2018.
Figure 2: Distribution of subjective self-rating of health when compared with the health of other people of the same age, Brasília, 2016/2018.
The distribution of subjective self-rating of health compared with rating the health of other people of same age according to the sociodemographic and clinical variables. The subjective self-rating of health comparing the current health status with that in the previous year indicated that the majority of the 189 participants (39.7%) reported being currently worse, 34.4% reported being same as that in the previous year, and 25.9% reported being better than that in the previous year.
Regarding the subjective self-rating of health compared with that in the previous year, according to the sociodemographic and clinical variables, a significant difference (p = 0.012) was obtained only for the variable schooling, i.e., most of those who self-reported being worse or better relative to the previous year had between 1 and 4 years of schooling (41.3% and 46.9%, respectively), whereas most of those who reported being the same as in the previous year had at least 5 years of schooling (46.2%), as shown in table 3.
|
Variables |
Worse |
Same |
Better |
p-value* |
|||
|
nº |
% |
nº |
% |
nº |
% |
||
|
Total |
75 |
100.0 |
65 |
100.0 |
49 |
100.0 |
- |
|
Sex |
|
|
|
|
|
|
|
|
Male |
24 |
32.0 |
29 |
44.6 |
16 |
32.7 |
0.245 |
|
Female |
51 |
68.0 |
36 |
55.4 |
33 |
67.3 |
|
|
Age group (years) |
|
|
|
|
|
|
|
|
80 to 84 |
40 |
53.3 |
41 |
63.1 |
28 |
57.1 |
0.506 |
|
≥85 |
35 |
46.7 |
24 |
36.9 |
21 |
42.9 |
|
|
Schooling (years) |
|
|
|
|
|
|
|
|
Never went to school |
24 |
32.0 |
10 |
15.4 |
15 |
30.6 |
0.012 |
|
1 to 4 |
31 |
41.3 |
24 |
36.9 |
23 |
46.9 |
|
|
≥5 |
18 |
24.0 |
30 |
46.2 |
10 |
20.4 |
|
|
No data |
1 |
1.3 |
1 |
1.5 |
1 |
2.0 |
|
|
Family income |
|
|
|
|
|
|
|
|
Up to 1.0 m.w. |
8 |
10.7 |
7 |
10.8 |
8 |
16.3 |
0.065 |
|
1.1 to 3.0 m.w. |
32 |
42.7 |
19 |
29.2 |
25 |
51.0 |
|
|
≥3.0 m.w. |
35 |
46.7 |
39 |
60.0 |
16 |
32.7 |
|
|
Polypharmacy |
|
|
|
|
|
|
|
|
Yes |
31 |
41.3 |
27 |
41.5 |
19 |
38.8 |
0.614 |
|
No |
27 |
36.0 |
31 |
47.7 |
24 |
49.0 |
|
|
No data |
17 |
22.7 |
7 |
10.8 |
6 |
12.2 |
|
|
Multimorbidity |
|
|
|
|
|
|
|
|
Yes |
32 |
42.7 |
27 |
41.5 |
24 |
49.0 |
|
|
No |
29 |
38.7 |
32 |
49.2 |
19 |
38.8 |
0.578 |
|
No data |
14 |
18.7 |
6 |
9.2 |
6 |
12.2 |
|
Table 3: Study of aging patterns among elderly outpatients living in different contexts.
Note: *p-value calculated using the chi-square test, disregarding patients without data.
An analysis of the individuals’ self-rating of their current health status compared with that in the previous year showed a significant difference in the distribution of proportions (p=0.003). An individual’s positive perception of the current health status changed to “worse” on comparing it with the health in the previous year, i.e., 32% of those who self-rated their current health status as worse than that in the previous year had self-rated their current status as positive, whereas 49.2% and 44.9% rated their health as the same and better than that in the previous year, respectively. In addition, self-rating of the current health status was negative in 16.0%, 4.1% and 0% of those individuals who had self-rated their health as worse, better, and the same as that in the previous year, respectively.
Discussion
The most relevant finding of the present study was that multimorbidity and polypharmacy did not influence the self-perception of health among very elderly individuals recruited from an outpatient geriatric care clinic of a university hospital.
Some authors have reported that multimorbidity and polypharmacy increase with advanced age. The prevalence of multimorbidity and polypharmacy demonstrated in the present study is in line with that reported in the literature [15,16]. However, according to the self-report instruments, these variables did not influence the self-perception of health.
In the present study, there were no significant differences in the subjective self-rating of the current health status according to the sociodemographic variables (sex, age group, schooling, and family income).
Some studies indicate an association of a negative self-rating of health among very elderly individuals with the development of chronic non-communicable diseases and their complications and with the concurrent use of multiple drugs [17,18]. The literature suggests that precarious economic conditions and limited material and mental resources to cope with problems lead to a more negative subjective self-perception of health [7,19], especially among very elderly people with low levels of schooling, low income, poor health, and high rates of comorbidities and disability [17,20]. However, the divergence is probably due to the fact that those studies included wider age groups (young adults and young old adults) than those assessed in the present study [7,18,19].
Moreover, research has shown that there are other factors associated with successful aging with positive self-rating by the very elderly, including centenarians, even in the presence of multimorbidity and functional dependence [11-13]. This positive self-rating may be associated with the psychological resilience of an individual and with factors such as psychosocial well-being, social comparison with other people of the same age, and life satisfaction. This feature may have accounted for the result of the present study that only 7% of the participants reported a negative self-perception of their health, rating it as very poor/poor.
The differences between the demographic variables and socioeconomic background according to which an very elderly person lives (community, geriatric, and internal medicine outpatient care or long-term care institutions) may influence the self-rating of health.
Health assessment in thevery elderly requires a multidimensional perspective of health and satisfaction that interact in old age, influencing patterns of activity and social engagement [21]. Researchers state that octogenarian or older individuals tend to underestimate the decline of their health and maintain a positive self-perception using different mechanisms, including comparing their health status with that of others [11,13].
The very elderly people in the present study perceived their health status to be better than that of their peers.
Compared with the health status in the previous year, the majority reported their current health status to be worse, followed by those who reported no changes, a finding that is in line with the literature [22]. These data suggest that very elderly individuals are confronted with anatomic and physiological changes that are inherent to the aging process. No significant differences were observed with regard to the variables polypharmacy and multimorbidity; however, a significant difference was observed regarding schooling.
Jylhä pointed out that the rating of perceived health increases with the level of schooling, probably because of the correlation between higher income and education level [23]. Alvarado demonstrated that a low level of schooling is a risk factor for cognitive decline, which increases the likelihood of lower quality of life and reflects on self-perception [24].
Regarding the self-rating of the current health status compared with that in the previous year, there was a significant difference in the distribution of proportions. The individuals’ positive perception of health changed to “worse” when they compared their current health status with that in the previous year. Those who self-rated their current health status as negative comprised those reporting a worsening of their health status, but even those who self-rated their current health status as positive reported it to be worse than that in the previous year. This may be associated with low levels of control over their health and with depressive symptoms. French, Sargent-Cox, and Luszcz reported the influence of depression on the self-rating of health with age advancement; the worsening of the self-rated health status is more associated with psychological symptoms, and it is therefore necessary to deepen the understanding regarding these mental health aspects and to further intervene in this area [25].
Successful aging may coexist with illnesses and functional limitations if compensatory psychological and/or social mechanisms are used, such as a positive feeling of well-being [15,26,27] and a positive self-perception of health and aging, as was observed in the present study. This coincidence of findings complies with one of the tenets of scientific research: reproducibility. This attestation indicates the possibility of a universal truth, i.e., the Popperian logic: it does not require a system to be susceptible of being considered as valid once and for all, in a positive sense; but it requires its logical form to be such that it is possible to validate it using empirical tests, in a negative sense; it must be possible to refute an empirical scientific system by experience”, until the opposite is proven (making the results falsifiable), these conclusions can be deemed reliable and valuable for the development of policies that aim to improve the care provided to this population age group.
In an attempt to define indicators that confirm that successful aging is possible, the WHO (2015) has proposed a shift from an epidemiological focus based on multimorbidity to a framework built around the functional ability of very elderly people [28]. Several studies have shown that strategies such as staying physically and mentally active, a balanced diet, and being socially engaged promote the functional ability of very elderly people and have a positive impact on their self-perception of health [13,15,29].
Conclusion
A positive self-perception of the aging process, including psychological and behavioral factors, mediated by a will to live, may influence longevity and increase life expectancy, regardless of sex, socioeconomic status, loneliness, and functional ability of the individuals [30]. These findings were obtained in a sample of individuals from other countries, i.e., from cultures and social structures different from those in Brazil. Nevertheless, the results are coincident, thus reinforcing the validity of the findings presented herein.
The heterogeneity of aging and health should be considered both with regard to the individual and the context in which he/she lives.
The sample of the present study comprised very elderly individuals recruited from a geriatric outpatient clinic of a university hospital. Therefore, a selection bias may exist, as the participants were all outpatients, and their self-perception of health may differ from that of very elderly people receiving institutionalized or home-based care.
The data obtained herein indicates trends that are in line with those reported in other studies with very elderly individuals: a positive self-perception of their own health despite multimorbidity, polypharmacy, and/or limitations in this stage of life, with a paradoxical relationship between these factors. This finding is confirmed by studies conducted in other countries with different cultural and socioeconomic contexts, thereby demonstrating that it is necessary to foster studies that assess the psychological and social mechanisms used by this population age group to live longer, thereby attaining great longevity.
The use of instruments to measure health self-perception should be included in the development of strategies for a more positive self-perception of the aging process, even in the presence of multimorbidity and polypharmacy, with the aim of ensuring healthy aging.
Data Availability
The data supporting the current study can be made available from the corresponding author upon reasonable request.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with ethical standards of the institution and/or national research committee (Ethics Committee on Research, Catholic University of Brasília) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflicts of Interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Funding Statement
This study was funded by the government agencies: Research Support Foundation of the Federal District (FAP-DF) and Coordination of Superior Level Staff Improvement (CAPES).
Acknowledgment
We thank the participants for sharing their lives, their knowledge, and their stories and for being always forthcoming and considerate in reporting how they are experiencing the aging process.
References
- Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional por Amostra de Domicílios Continuada [monographon Internet]. Rio de Janeiro: IBGE; 2017 [Cited 23 Feb 2019].
- Inouye K, Pedrazzani ES, Pavarini SCI (2008) Octogenários e Cuidadores: Perfil Sócio- Demográfico e Correlação da Variável Qualidade de Vida. Texto Contexto Enferm 17: 350-
- Veras RP (2011) Estratégias Para o Enfrentamento das Doenças Crônicas: Um Modelo em que Todos Ganham. Rev Bras Geriatr Gerontol 14: 779-
- Le Reste JY, Nabbe P, Rivet C, Lygidakis C, Doerr C, et al. (2015) The European general practice research network presents the translations of its comprehensive definition of multimorbidity in family medicine in ten European languages. PLoS One 10: 0115796.
- Elmståhl S, Linder H (2013) Polypharmacy and inappropriate drug use among older people: a systematic review. Healthy Aging Clin Care Elder 5: 1-8.
- Kleinspehn-Ammerlahn A, Kotter-Grühn D, Smith J (2008) Self-perceptions of aging: do subjective age and satisfaction with aging change during old age? J Gerontol 63: 377-385.
- Borim FSA, Barros MBA, Neri AL (2012) Autoavaliação da Saúde em Idosos: Pesquisa de Base Populacional no Município de Campinas, São Paulo, Brasil. Cadernos de Saúde Pública 28: 769-
- Martin LG, Schoeni RF, Freedman VA, Andreski P (2007) Feeling better? Trends in general health status. J Gerontol 62: 11-21.
- Shulamit BL, Jean KE, Thomas KR, Thomas AA, Donna RJ, et al. (1997) Predicting mortality from community surveys of older adults: the importance of self-rated functional ability. J Gerontol B Psychol Sci Soc Sci52: 155-163.
- Sargent-Cox KA, Anstey KJ, Luszcz MA (2014) Longitudinal change of self-perceptions of aging and mortality. J Gerontol 69: 168-173.
- Henchoz K, Cavalli S, Girardin M (2008) Health perception and health status in advanced old age: a paradox of association. J Aging Stud 22: 282-290.
- Carstensen LL, Turan B, Scheibe S, Ram N, Ersner-Hershfield H, et al. (2011) Emotional experience improves with age: evidence based on over 10 years of experience sampling. Psychol Aging26: 21-33.
- Araújo L, Teixeira L, Ribeiro O, Paúl C (2018) Objective vs. subjective health in very advanced ages: looking for discordance in centenarians. Front Med (Lausanne) 5: 189.
- Brucki SMD, Nitrini R, Caramelli P, Bertolucci PHF, Okamoto IH (2003) Sugestões Para o Uso do Mini-Exame do Estado Mental no Brasil. Arq Neuro-Psiquiatr 61: 777-
- Curcio CM, Pineda A, Quintero P, Rojas A, Muñoz S, et al. (2018) Successful aging in Colombia: the role of disease. Gerontol Geriatr Med 4: 1-11.
- Kostev K, Jacob L (2018) Multimorbidity and polypharmacy among elderly people followed in general practices in Germany. Eur J Intern Med55: 66-68.
- Carvalho AT, Malta DC, Barros MBA, Oliveira PNFP, Mendonça DMMV, et al. (2015) Desigualdades na Autoavaliação de Saúde: Uma Análise Para Populações do Brasil e de Portugal. Cad Saúde Pública 31: 2449-
- Confortin SC, Giehl MWC, Antes DL, Schneider IJC, d’Orsi E (2015) Autopercepção Positiva de Saúde em Idosos: Estudo Populacional no Sul do Brasil. Cad Saúde Pública31: 1049-1060.
- Robert AS, Cherepanov D, Palta M, Dunham NC, Feeny D, et al. (2009) Socioeconomic status and age variations in health-related quality of life: results from the national health measurement study. J Gerontol 64: 378-389.
- Medeiros SM, Silva LSR, Carneiro JA, Ramos GCF, Barbosa ATF, et al. (2016) Fatores Associados à Autopercepção Negativa da Saúde entre Idosos Não Institucionalizados de Montes Claros, Brasil. Ciênc Saúde Coletiva 21: 3377-
- Pinto JM, Neri AL (2013) Doenças Crônicas, Capacidade Funcional, Envolvimento Social e Satisfação em Idosos Comunitários: Estudo Fibra. Ciênc Saúde Coletiva 18: 3449-3460.
- Antunes JLF, Filho ADPC, Duarte YAO, Lebrão ML (2019) Desigualdades Sociais na Autoavaliação de Saúde de Idosos da Cidade de São Paulo. Rev Bras Epidemio l 21: 180010.
- Jylhä M (2009) What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med 69: 307-316.
- Alvarado BE, Zunzunegui MV, Del Ser T, Béland F (2002) Cognitive decline is related to education and occupation in a Spanish elderly cohort. Aging Clin Exp Res14: 132-142.
- French DJ, Sargent-Cox K, Luszcz MA (2012) Correlates of subjective health across the aging lifespan: understanding self-rated health in the oldest old. J Aging Health 24: 1449-1469.
- Smith J, Borchelt, M, Maier H, Jopp D (2002) Health and well-being in the young old and oldest old. J Soc Issues 58: 715-732.
- Young Y, Frick KD, Phelan EA (2009) Can successful aging and chronic illness coexist in the same individual? A multidimensional concept of successful aging. J Am Med Dir Assoc 10: 87-92.
- World Health Organization (2015) World Report on Aging and Health. World Health Organization, Genève, Switzerland.
- Orb A (2004) Aspectos de Salud en Adultos Mayores de 80 Anos de Edad que Viven Independientemente en la Comunidad: Una Perspectiva Australiana. Latino-Am Enfermagem 12: 589-596.
- Levy BR, Slade MD, Kunkel SR, Kasl SV (2002) Longevity increased by positive self-perceptions of aging. J Pers SocPsychol 83: 261-270.
Citation: Alves VP, de Souza Barbosa MP, de Melo GF (2021) Multimorbidity and Polypharmacy do not influence the Self-Perception of Health among the very Elderly: A Cross-Sectional Study. J Pract Prof Nurs 5: 028.
Copyright: © 2021 Vicente Paulo Alves, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.