Outcome Measures for Post-Shoulder Injury Surgical Intervention Therapeutic Rehabilitation
*Corresponding Author(s):
Unruh SADepartment Of Kinesiology And Sport Sciences, University Of Nebraska, Kearney, NE, United States
Tel:+1 3084404390,
Email:unruhsa@unk.edu
Abstract
A commonality among all surgical procedures correcting shoulder injuries is the requirement of post-surgical therapeutic rehabilitation. The purpose of this cross-sectional study was to examine post-surgery shoulder rehabilitation outcomes from archival data of subjects who underwent rotator cuff repairs, biceps tendonesis, and/or Superior Labrum Tear from Anterior to Posterior (SLAP) repair surgery. Specific interest was paid to therapeutic outcomes from orthopedic physical therapy at a semi-rural Midwestern outpatient clinic with an interest in identifying common therapeutic intervention strategies. Rehabilitation outcomes measures included: total length of rehabilitation, maximal shoulder range-of-motion achieved, number of scheduled therapy sessions missed, and exercises performed. Thirty-two subjects significantly increased passive flexion, external rotation, and active flexion Range of Motion (ROM) during therapy (p<.001). There was no significant effect on rehabilitation outcomes between physicians performing the surgery or physical therapists overseeing rehabilitation (p>.219 and p>.096 respectively). The largest external determinant for subject’s length and quality of recovery in the rehabilitation is the severity of injury and subsequent surgery. Additionally, standard timelines for common shoulder exercises and progressions were found. We can potentially use these data for optimizing current post-surgical shoulder rehabilitation.
Key Points
- Length of rehabilitation may be solely dependent upon severity of injury
- Number of rehabilitation sessions do not impact patient outcomes
- Patient reliability of attendance to therapy sessions significantly correlates with length of rehabilitation
Keywords
Athletic training; Physical therapy; Range-of-motion
INTRODUCTION
Shoulder injuries are one of the most common and debilitating musculoskeletal injuries suffered by the middle-aged adult workforce in America [1-3]. It is estimated 4.5 million doctor visits a year can be attributed to shoulder pain across the America [2]. Of these visits, approximately 250,000 patients are referred for further repair surgery, costing each patient an average of $19,000 or $4.8 billion in total [1]. Of the remaining patients not referred to surgery, non-operative shoulder pain treatments can end up costing about $40,000 per patient per year [1]. Shoulder injuries can result in pain, fatigue, limited motion in the arm, and even weakness lasting 6-12 weeks or longer [3].
Although the prevalence of shoulder injury or pain increases with age, shoulder injuries can occur to individuals of any age for a variety of reasons associated with activities of daily living or extracurricular activities [1-9]. Rotator cuff tears in younger adults (under 40 years old) are typically attributed to acute traumatic injuries [7]. Prevalence rates for younger adults (under 40years old) fluctuate due to their specific etiology, but one review found a range of ages for rotator cuff tears among different studies to be 16-40 years old (the average ages between studies ranged from 22 to 33 years old) [7]. Rotator cuff tears in elderly adults are typically attributed to chronic overuse increasing with age [9]. Prevalence of rotator cuff tears in elderly adults (65+ years old) with shoulder pain is about 22% [5]. Prevalence of rotator cuff tears in adult’s age 70-79 years old was 31%, and adults age 80+ years old saw prevalence rates as high as 51% [8].
One of the most prominent debates in the physical therapy field currently is whether surgery is the best management option for rotator cuff injuries, or if non-operative measures are more effective [2-9]. me studies suggest that younger patients benefit more from surgery than do older patients, possibly due to the nature of an acute injury versus chronic injuries [4-9]. Middle age patients seem to fall on a continuum between the two age groups with more gravitating towards surgery than non-operative rehabilitation [9]. Conversely, older patients (>65 years old) sometimes seem to benefit more from non-operative rehabilitation for their shoulder injuries than do younger patients, due to a lower healing potential from natural aging processes [4-9]. Patients who choose surgical options may undergo one of three major surgical options: biceps tenodesis, rotator cuff repair, or a Superior Labrum Tear from Anterior to Posterior (SLAP) repair [6-9]. Biceps tenodesis is a surgical procedure where the biceps tendon attachment to the labrum is torn or inflamed so the surgeon reattaches the tendon directly to the humerus bone [6]. A rotator cuff repair requires surgical repairing of any or all of the tendons (subscapularis, supraspinatus, infraspinatus, and teres minor muscles) and can incorporate attaching tendons to bone or stitching of tendons back together [6]. A SLAP repair is required for any other injury to the labrum not including the biceps tendon and can incorporate suturing or stitching any part of the labrum back together [6]. Among the various surgical procedures includes required post-surgery rehabilitation [4-6]. Clinicians directly control the modalities and therapeutic exercises used in physical therapy to affect the progress of and optimize shoulder rehabilitation. However, current data supporting the optimal therapeutic intervention strategies (duration, frequency, intensity) is needed to ensure that the most efficient therapeutic practices are being used [4-9].
The purpose of this cross-sectional study was to examine post-surgery shoulder rehabilitation outcomes (subject length of rehabilitation, final shoulder range-of-motion, and number of therapy sessions missed) from subjects who underwent rotator cuff repairs, biceps tenodonesis, and/or SLAP repair surgery and orthopedic physical therapy at a semi-rural outpatient clinic in the Midwest United State. A secondary purpose was to identify common88 therapeutic intervention strategies that might positively affect post-surgery shoulder rehabilitation patient outcomes and optimize them.
METHOD
Subjects
Therapeutic records for thirty-two subjects from a rural Midwestern community (18 males and 14 females aged 54.7±8.2 years) were included for use in this study. Inclusion criteria included subjects who had reported to the sports medicine rehabilitation clinic between 2011 and 2016 for shoulder pain and had undergone surgical corrections from one of three affiliated physicians for their shoulder injury. Additionally, all subjects had received the majority of their physical therapy instruction from one of eight affiliated physical therapists. All gender, age, and ethnicities were included in this study. Exclusion criteria include records of subjects who only received physical therapy for shoulder pain (non-operative subjects) and subjects who did not complete their therapy at the same rural sports medicine clinic. All subject identifying markers were removed from archival data sets per HIPPA guidelines.
Therapeutic interventions
After the initial injury evaluation and surgical correction by the physician, each subject underwent an initial post-surgical assessment with a licensed physical therapist to determine the level of shoulder disability from surgery. Therapeutic interventions began and included a Range of Motion (ROM) phase and a strengthening phase per an established protocol of the clinic. The ROM phase focused on increasing both passive and active shoulder ROM. The strengthening phase focused on increasing strength and endurance of the shoulder and supportive musculature. The weekly progression of ROM, therapeutic exercise, and modality prescription (type, intensity, frequency) were recorded on each subject’s chart per visit in addition to subject subjective shoulder activity and assessment. Although each specific treatment prognosis varied in response to patient needs, the general protocol for each patient remained consistent and can be found in table 1 below:
|
Phase |
Example Modalities |
Frequency |
Duration |
Intensity |
|
|
Evaluation |
Assessment |
1st Visit |
1 Day |
N/A |
|
|
Education |
|||||
|
ROM |
Passive |
|
2-3x/Week |
6-8 Weeks |
Low |
|
|
PROM |
||||
|
|
Codman’s |
||||
|
|
Pulleys |
||||
|
Active |
|
||||
|
|
Active Assistive |
||||
|
|
AROM |
||||
|
Strengthening |
Thera-Band |
|
2-3x/Week |
Week 8+ |
Moderate |
|
|
IR |
||||
|
|
ER |
||||
|
|
Rows |
||||
|
|
Triceps Extension |
||||
|
Dumbbell |
|
||||
|
|
Side-lying ER |
||||
|
|
Prone Row |
||||
|
|
Horizontal Abduction |
||||
|
|
Bicep Curl |
||||
|
Cable Machine |
|
||||
|
|
Row |
||||
|
|
Triceps Extension |
||||
Table 1: Generalized Treatment Protocol.
Procedures
After this study was approved by the primary investigator’s Institutional Review Board (IRB) and permission was obtained from the director of the sports medicine rehabilitation clinic, a systematic review of the archival data obtained from subject records was performed. Qualifying subjects were screened via billing coding and hard-copy treatment records were examined. The detailed treatment records included each primary variable including: active and passive ROM measurements, exercises performed, length of rehabilitation, number of therapy sessions missed, and a brief description of the therapy session for all subjects.
Statistical analysis
Data from subject’s treatment records were converted from paper charts to a digital spreadsheet via statistical software [IBM SPSS Statistics v 25 (IBM, Armonk, NY)] and coded. Subject files were grouped according to the type of surgery and criteria included subjects who received: biceps tenodonesis repair (Group 1), rotator cuff repair (Group 2), SLAP and rotator cuff repair (Group 3), biceps tenodonesis and rotator cuff repair (Group 4), biceps tenodonesis, SLAP, and rotator cuff repair (Group 5), and minor surgical debridement (Group 6). Each of the measured outcome variables were compared.
Descriptive characteristics including age, gender, and injured side for each group is reported in table 2. A one-way ANOVA was performed on each group, physician, and physical therapist for each outcome variable (length of rehabilitation, range of motion, number of rehabilitation sessions) via IBM SPSS Statistics. A regression analysis was performed between number of therapy visits, total number of days spent recovering, and number of therapy visits missed. Additionally, an effects-coded regression analysis was performed between injury group and length of rehabilitation. Data was analyzed for statistical significance at the p<.05 level of significance.
|
|
All |
Group 1 |
Group 2 |
Group 3 |
Group 4 |
Group 5 |
Group 6 |
|
n |
32 |
4 |
5 |
4 |
14 |
3 |
2 |
|
Age (years)* |
54.56±8.20 |
47.50±6.45 |
59.40±8.79 |
56.00±5.29 |
55.43±7.14 |
57.67±3.79 |
43.00±15.56 |
|
Gender (M - F) |
18 - 14 |
3 - 1 |
3 - 2 |
0 - 4 |
8 - 6 |
3 - 0 |
1 - 1 |
|
Injured Side (R - L) |
21 - 11 |
3 - 1 |
3 - 2 |
3 - 1 |
10 - 4 |
1 - 2 |
1 - 1 |
* = Data reported as means ± standard deviation
No significant (p>0.05) difference for any of the parameters
Table 2: Descriptive Characteristics.
RESULTS
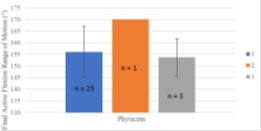
Groups 1 through 6 included four (3 male and 1 female), five (3 male and 2 female), four(4 female), fourteen (8 male and 6 female), three (3 male), and two (1 male and 1 female)patients respectively (Table 1). There was no significant (p>.05) difference between subjects’ ages of any of the shoulder procedure groups (Table 1).Additionally, there was no significant(p>.219) difference between physicians who performed the surgical procedure on length of recovery or final AROM, and there was no significant (p>.096) difference between physical therapist in charge of rehabilitation and length of recovery or final AROM (Figures 1-4).There was a significant (p<.001) difference between initial and final PROM during flexion and external rotation and between initial and final AROM during flexion for all subjects(Figure 5).
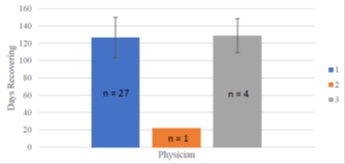
No significant (p>0.05) difference between Physicians 1 and 2
Figure 1: Average number of day’s patient spent recovering by physician.
No significant (p>0.05) difference between Physicians 1 and 2
Figure 2: Average final active flexion range of motion in injured arm of patient by physician.
No significant (p>0.05) difference between Physical Therapists 1, 2, or 3
Figure 3: Average number of days patient spent recovering by physical therapist.

No significant (p>0.05) difference between Physical Therapists 1, 2, or 3
Figure 4: Average final active flexion range of motion in injured arm of patient by physical therapist.
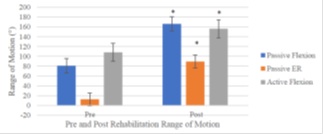
* = Significant (p<0.05) difference from pre-measurement
Figure 5: Average pre and post physical therapy rehabilitation range of motion for passive flexion, external rotation and active flexion.
No significant differences were found for any of the outcome variables (final PROM, AROM, length of rehabilitation (Figure 6), and number of rehabilitation sessions (Figure 7) between any of the groups (all p>.089 [.089-.815] and all η2p<.001, R2=0.524) between number of therapy visits and total number of days recovering (Figure 8). There was no significant correlation between number of therapy visits missed and total number of days recovering or total number of physical therapy visits respectively (Figure 9). Additionally, there was a significant correlation (r=0.684, p=.04, R2=0.468) between total number of days spent in rehabilitation and injury group.
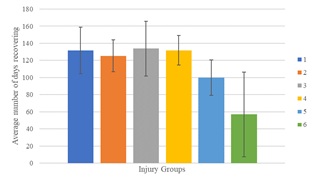
No significant (p>0.05) difference between any group
Figure 6: Average number of days recovering for each injury group.
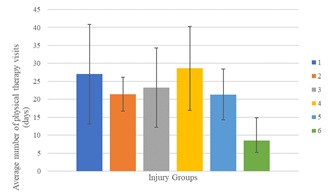
No significant (p>0.05) difference between any group
Figure 7: Average number of rehabilitation sessions for each injury group.
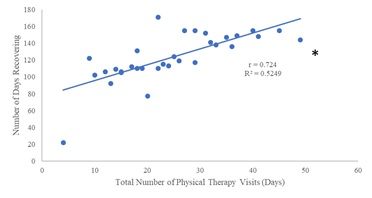
* = Significant (p<0.05) correlation present
Figure 8: Number of days recovering vs number of rehabilitation sessions.
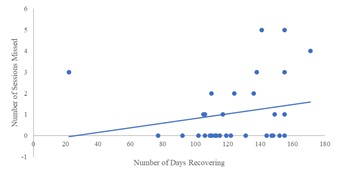
No significant (p>0.05) correlation present
Figure 9: Number of rehabilitation sessions missed vs number of days recovering.
DISCUSSION
All physicians and physical therapists included in this study provided universally consistent treatment to shoulder injury subjects, and did not seem to significantly alter subject outcomes. Number of physical therapy visits significantly correlated with length of rehabilitation, which indicates that the length of rehabilitation is strongly tied with time spent under direct physical therapist supervision. Number of physical therapy visits is generally based on severity of shoulder injury, yet severity of shoulder injury was not found to be a significant determining factor in any of the rehabilitation outcomes in this study. There are very few published articles on identifying factors that affect post-surgical shoulder rehabilitation outcomes to date [10]. However, factors affecting shoulder replacement recovery outcomes have been investigated and report similar findings [10-12]. One study conducted on 98 subjects who received total shoulder arthroplasty for primary and secondary osteoarthritis in the glenohumeral joint found significant positive gains in pain, activity, movement, and power with 93.9% of subjects feeling good or very good about their shoulder in a 6 year post-surgery follow-up [11]. Another study conducted on 27 subjects who received total shoulder arthroplasty for proximal nonunion humeral fractures saw marked decreases in function with a much lower patient satisfaction rate of 48% [12]. As Wolff and Rosenzweig(2017) noted, two major differences between these two studies were underlying pathology and severity of tissue injury, which is confirmed in our analysis as well [10]. Although the allostatic loads differ due to variations in biomechanics, factors affecting knee rehabilitation outcomes present similar general results. One study investigating the effect of weight on the rehabilitation outcomes of 354 total knee replacement subjects found that obese subjects’ rehabilitation progress was significantly delayed and total motion and function was significantly reduced when compared to normal and overweight individuals [13]. Similarly, a non-surgical intervention rehabilitation study found that the presence of osteoarthritis in the knee significantly impaired stroke victims’ functionality improvements compared to stroke victims without the condition [14]. In both these studies, pre-existing conditions or pathologies were found to cause the biggest influence on rehabilitation outcomes which correspond to our findings.
Timing is known to play a very large factor in returning the patient back to pre-injury abilities [15-19]. Specifically, the longer it takes for a patient to begin exercising/strength training in the injured area, the longer it will take for them to return [15]. One study estimated that nearly 4%of a patient’s muscular strength is lost per day of inactivity during post-injury immobilization [16]. Unfortunately, many studies indicate that the rate of recovery is significantly longer than the rate of atrophy [16-19]. Indeed, it may take up to 3-5 times longer to regain strength then it does to lose it [15].
Patient adherence to home-based programs assigned and monitored by professionals has also been shown to be a major factor in long term patient success [20]. The World Health Organization has suggested that, due to its vital importance in the rehabilitation process, health professionals must monitor patient adherence with in person and frequent follow-ups to ensure program success [20]. Monitoring patient adherence accurately is difficult and some published studies have had differing opinions regarding the methods. One studied published in 2014 by Silverio and Cheung used a verified patient self-report questionnaire on 45 rotator cuff repair patients at their 6-week follow-up appointment [21]. In this study, the authors found no significant difference in outcomes between high compliant and low compliant patients [21]. An alternate study published in 2004 (Brewer, et al.) created an adherence variable for 108 post-ACL reconstruction surgery patients consisting of two components: 1. A daily self-reporting exercise log cross referenced with the number of times the video exercises were accessed and 2. Patient rehabilitation session attendance with an effort score assigned by the overseeing therapist using a verified adherence scale [22]. In this study, the authors found a significant portion of the rehabilitation outcomes were determined via patient adherence with higher levels of adherence relating to better rehabilitation outcomes [22]. A key difference between these two studies is the reliance on self-reported and un-validated adherence levels being influenced by recollection and social desirability biases [21,22].
CONCLUSION
The rural Midwestern sports medicine orthopedic and rehabilitation outpatient clinic provides consistent shoulder injury rehabilitation services across all physicians and physical therapists. Subject recovery time seems to be more influenced by number of physical therapy sessions (thus the severity of underlying shoulder pathology) than subject demographics (gender and injury side). A limitation to this research was subject compliance to home exercise programs. Future articles should investigate the effects of exercise timing on rehabilitation outcomes and gathering data on larger sample sizes.
REFERENCES
- Mather RC 3rd, Koenig L, Acevedo D, Dall TM, Gallo P, et al. (2013) The societal and economic value of rotator cuff repair. J Bone Joint Surg Am 95: 1993-2000.
- Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG (2007) Indications for rotator cuff repair: a systematic review. Clin Orthop Relat Res 455: 52-63.
- Shanahan EM, Sladek R (2011) Shoulder pain at the workplace. Best Pract Res Clin Rheumatol 25: 59-68.
- Edwards P, Ebert J, Joss B, Bhabra G, Ackland T, et al. (2016) Exercise rehabilitation in the non- operative management of rotator cuff tears: a review of the literature. Int J Sports Phys Ther 11: 279-301.
- Fehringer EV, Sun J, VanOeveren LS, Keller BK, Matsen FA 3rd (2008) Full-thickness rotator cuff tear prevalence and correlation with function and co-morbidities in patients sixty-five years and older. J Shoulder Elbow Surg 17: 881-885.
- Greenspoon JA, Petri M, Warth RJ, Millett PJ (2015) Massive rotator cuff tears: pathomechanics, current treatment options, and clinical outcomes. J Shoulder Elbow Surg. 24: 1493-1505.
- Lazarides AL, Alentorn-Geli E, Choi JJ, Stuart JJ, Lo IK, et al. (2015) Rotator cuff tears in young patients: a different disease than rotator cuff tears in elderly patients. J Shoulder Elbow Surg 24: 1834-1843.
- Tempelhof S, Rupp S, Seil R (1999) Age-related prevalence of rotator cuff tears in asymptomatic shoulders. J Shoulder Elbow Surg 8: 296-299.
- Wolf BR, Dunn WR, Wright RW (2007) Indications for repair of full-thickness rotator cuff tears. Am J Sports Med 35: 1007-1016.
- Wolff AL, Rosenzweig L (2017) Anatomical and biomechanical framework for shoulder arthroplasty rehabilitation. J Hand Ther 30: 167-174.
- Levy O, Copeland SA (2001) Cementless surface replacement arthroplasty of the shoulder: 5-to 10- year results with the Copeland mark-2 prosthesis. J Bone Joint Surg Br. 83: 213- 221.
- Antuña SA, Sperling JW, Sánchez-Sotelo J, Cofield RH(2002) Shoulder arthroplasty for proximal humeral nonunions. J Shoulder Elbow Surg 11: 114-121.
- Liao CD, Huang YC, Chiu YS, Liou TH (2017) Effect of body mass index on knee function outcomes following continuous passive motion in patients with osteoarthritis after total knee replacement: A retrospective study. Physiotherapy 103: 266-275.
- Doruk, P (2013) The impact of knee osteoarthritis on rehabilitation outcomes in hemiparetic stroke patients. J Back Musculoskelet Rehabil. 26: 207-211.
- Houglum PA (2016) Therapeutic Exercise for Musculoskeletal Injuries 4th Edition. Human Kinetics.
- Appell HJ (1990) Muscular atrophy following immobilisation. Sports Med 10: 42-58.
- Staron RS, Leonardi MJ, Karapondo DL, Malicky ES, Falkel JE, et al. (1991) Strength and skeletal muscle adaptations in heavy-resistance-trained women after detraining and retraining. J Appl Physiol 70: 631-640.
- Hortobágyi T, Dempsey L, Fraser D, Zheng D, Hamilton G, et al. (2000) Changes in muscle strength, muscle fibre size and myofibrillar gene expression after immobilization and retraining in humans. J Physiol 524: 293-304.
- MacDougall JD, Elder GCB, Sale DG, Moroz, JR, Sutton JR (1980) Effects of strength training and immobilization on human muscle fibres. Eur J Appl Physiol Occup Physiol 43: 25-34.
- World Health Organization. Adherence to long-term therapies: evidence for action. 2003.
- Silverio LM, Cheung EV (2014) Patient adherence with postoperative restrictions after rotator cuff repair. J Shoulder Elbow Surg 23: 508-513.
- Brewer BW, Cornelius AE, Van Raalte JL, Brickner JC, Sklar JH, et al. (2004) Rehabilitation adherence and anterior cruciate ligament reconstruction outcome. Psychol Health Med 9: 163-175.
Citation: Maupin C, Unruh SA, Akehi K, Bice M, Weed W, et al. (2020) Outcome Measures for Post-Shoulder Injury Surgical Intervention Therapeutic Rehabilitation. Sport Med Inj Care 2: 007.
Copyright: © 2020 Maupin C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.