Pathophysiology of Delirium in End-of-Life Patient: A Systematic Review
*Corresponding Author(s):
María Nabal VicuñaPalliative Care Supportive Team, Hospital Universitari Arnau De Vilanova, Lleida, Spain
Email:mnabal.lleida.ics@gencat.cat
Abstract
Objectives: Review of current understanding of delirium in terminally ill patients, emphasizing on precipitating factors, etiology and physiopathology.
Methods: Systematic review conducted on PubMed, Cochrane, Scopus, Web of Science and Scielo databases. To identify relevant studies, the search strategy utilized combinations of MeSH terms and keywords including "Delirium," "Palliative Care," and "Pathophysiology," while limiting inclusion criteria to studies written in English, with full-text availability and containing an abstract.
Material and results: From 603 papers found, 18 articles were included, of which 14 were reviews and 4 were studies. Only one double-blind randomized clinical trial was considered to be relevant. The most commonly studied hypotheses were those related to imbalances in neurotransmitter levels and neurotoxicity resulting from organ failure.
Conclusion: Delirium is a common distressing neuropsychiatric syndrome among end-stage patients. Multifactorial pathophysiology includes neurotransmitter and sleep-wake dysregulations, organ dysfunction and prolonged stress and inflammatory states. Precipitating factors such as drugs, infections, electrolyte imbalances, hypoxia, dehydration, pain and social conditions trigger delirium in predisposed patients.
Keywords
Alcohol; Alzheimer; Cognitive impairment; Delirium; End-of-life; Parkinson; Pathophysiology
Introduction
- Delirium
Delirium is a serious neurocognitive syndrome characterized by an acute disruption of attention, awareness and orientation. It is important to highlight the sudden onset of the symptoms and the fluctuation of these during the length of the process. Disorganized thinking, changes on mood and behavior and sleep-wake cycle disturbances are the most common symptoms. This global brain dysfunction usually occurs as a complication of an undelaying pathological process [1].
It is often underdiagnosed, leading to mistaken treatments and high distress in patients, families and caregivers [2-19]. Delirium creates significant communication difficulties [10], hindering patients from expressing their wishes and saying goodbye [20]. Depending on clinical features, delirium can be classified as hypoactive, hyperactive or mixed sub type.
- Palliative care definition
Palliative care is the branch of healthcare that focuses on total care of the patients with life-threatening diseases. This interdisciplinary work emphasizes improvement of quality of life for patients whose illnesses failed to curative measures. It aims to achieve proper pain control while providing relief to patients and their families in the social, psychological, spiritual spheres. “Palliative care affirms life and regards dying as a normal process; it neither hastens nor postpones death. It sets out to preserve the best possible quality of life until death [21].”
- Epidemiology of delirium at the end of life
Delirium is the most common neuropsychiatric complication in terminally ill patients and it is seen in 88-90% of patients during the last week of life or at the moment of death [11,14,18,19]. According to epidemiological measures, prevalence of delirium in Palliative Care oscillates around 13-88%. In parallel, incidence increases to a range of 3-45% [8,22]. Not only frequency shows importance of this diagnosis. Delirium highly increases risk of dying during admission or soon after it. Several studies have showed mortality rate ascends to 10-65% [16]. Most frequently found patient’s demographics include male gender, advanced age, sensorial impairments, neurocognitive/dementia diagnosis, previous psychiatric disorders (as depression), polypharmacy, metabolic disturbances, severe organic illness, dehydration, immobility, functional dependence, stroke antecedents, malnutrition and alcoholism [9,14,16,19,23]. Hypoactive delirium is the predominant subtype among terminally ill patients, likewise, the least diagnosed [10].
- Importance of pathophysiology
Understanding pathophysiology facilitates research towards discovering therapy targets. Wide knowledge helps to stablish preventive measures and to guide correct management. By being aware of how delirium develops, progression of this syndrome may be blocked. This decreases complications incidence and improves patient’s quality of life while ensuring efficient use of resources.
Objective
Major objective from this article is to review delirium’s literature in context of end-of-life or Palliative Care subsidiary patient, focusing closely on precipitating factors and physiopathology of this syndrome.
Proposed specific objectives are:
- To stablish etiological and precipitating factors that favor appearance of delirium in terminally ill patients.
- To review delirium’s pathophysiology in advanced diseases/end-of-life situation.
Materials And Methods
- Review design
Biographic research has been explored in the following Databases: PubMed, Cochrane, Web of Science, Scopus and Scielo. Applied keywords, inclusion and exclusion criteria and search strategy are detailed below in pursuit of finding related literature to this review.
- Keywords
These Me SH terms and keywords were used for conducting the search among the different databases: “Palliative Care”, “Delirium”, “Pathophysiology”, “End-of-life" and "Cognitive impairment” combined with terms as “Parkinson”, “Alzheimer” and “Alcohol”, to exclude irrelevant papers.
- Inclusion and exclusion criteria
Inclusion criteria that have been taken into consideration are:
• Articles in English language.
• Terminally ill or receiving Palliative Care patients, diagnosed of delirium.
• Full text article.
• Presence of abstract.
Applied exclusion criteria are:
• Articles not exposed in English.
• Patients diagnosed of delirium due to alcohol withdrawal, after surgery, dementia or other cognitive illnesses, etc.
• Unavailable “Full text article”.
• Absence of abstract.
- Search strategy
Initial research has been guided by PICO question strategy, so it is possible to find objective answers to this article’s aims and elevate the quality of evidence. In this review, the following research question was formulated: "What are the etiological and pathophysiological factors that favor the presence of delirium in patients with advanced disease or end-of-life situation? (Annex 1) ".Successive phase was executed according to PRISMA 2020, which helps to expand a correct systematic review announcing evidence-based items. Additional papers were included by reviewing the bibliographies of the selected articles. Detailed flow diagram is presented hereafter (Figure 1).
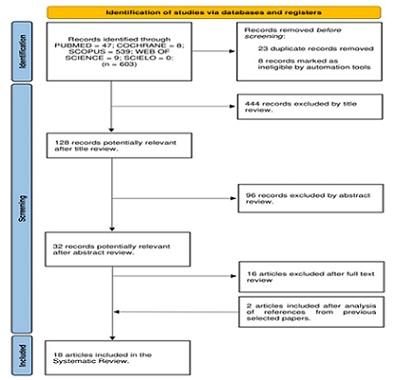 Figure 1: Flow diagram for literature searching and screening.
Figure 1: Flow diagram for literature searching and screening.
Results
Keywords combinations were used in Database search engines to obtain initial quantitative paper selection (Annex 2) (Tables 1&2).
Table of contents: Reviews
|
Author/Country/Year
|
Article design/Population |
Results and conclusions |
|
Bruera et al./Canada/1998 [3] |
[Review]
Patients receiving palliative care |
Main causes of delirium in advanced cancer patients: 1. Increased calcium levels and reduced sodium levels. 2. Renal failure. 3. Drug toxicity (mainly due to opioids).
|
|
Ross et al./U.S./2001 [2] |
[Review]
Terminally ill patients |
Main causes of delirium at the end of life: 1. Medication (opioid and benzodiazepine withdrawal) 2. Dehydration. 3. Infections. 4. Hypoxia. Major pathophysiologic mechanism in end-of-life patients is deterioration in renal and hepatic function, which multiply risk of drug toxicity. This situation leads easily to delirium.
|
|
Lawlor at al./Canada/2002 [11] |
[Review]
Advanced cancer patients |
Etiology and pathophysiology of delirium is multifactorial. The common molecular pathway is related to neurotransmitters imbalance. Implicated factors are: - High dopamine levels and acetylcholine deficiency. - Serotonin, GABA, cytokines and cortisol. - Dehydration leads to hypoperfusion, which consequently reduces renal elimination of metabolites and drugs as opioids (causing toxicity): 1. Meperidine produces neurotoxic metabolite normeperidine (anticholinergic effect). 2. Fentanyl and methadone result in neurotoxicity without known metabolites. - Hyponatremia: secondary to ascites, obstructions, chronic nausea and diarrhea. - Hypoalbuminemia, - Diuretics and SIADH, causing dehydration-like situation.
|
|
Friedlander at al./U.S./2004 [18] |
[Review]
Patients receiving palliative care |
Multifactorial etiology: dehydration, medication, hypoxia, infections, systemic cancer involvement, renal and hepatic failure (discovered in < 50% of terminally ill patients). Precipitating factors: 1. Infection. 2. Electrolyte imbalance. 3. Vascular complications. 4. Adverse medication effects (corticoids as dexamethasone or prednisone). 5. Others: hypercalcemia, hypoxia, paraneoplastic syndromes or disseminated intravascular coagulation.
|
|
Yennurajalingam at al./U.S./2005 [19] |
[Review]
Terminally ill elderly patients |
Delirium is a potential emergency in palliative care. Poor pain control increases risk and creates a vicious circle, cause pain’s expression requires cognition. Pathophysiology: cholinergic deficiency and excessive dopaminergic activity.
|
|
Lagman at al./U.S./2005 [14] |
[Review]
Advanced cancer patients |
Terminal delirium is irreversible and has no identifying features. Most common etiologies: medications, infection and central nervous system malignancies. Diagnosis: complete bool count, renal and hepatic function and oximetry. CT scans and MRI may be needed. Pathophysiology is related to neurotransmitter dysfunction: Acetylcholine deficiency and dopamine and serotonin excess.
|
|
White at al./United Kingdom/2007 [16] |
[Review]
Patients in end-of-life situation |
Precipitant factors: infection, metabolic disturbances, hypoxia, anemia, urine retention, fecal impaction, alcohol withdrawal, surgery, psychosocial factors and drugs. - Drug toxicity in Palliative Care: 1. Opioids: dose-related toxicity because some of them decrease acetylcholine release in cerebral cortex (oxycodone) or bind to muscarinic receptors (fentanyl). 2. Ant secretory medication: hyoscine hydrobromide and glycopyrronium are anticholinergic drugs. 3. Anxiolytics: benzodiazepines, which reduce cholinergic function. 4. Polypharmacy: lithium, anticholinergic and antipsychotics due to medication interaction. - Electrolytes: hyper and hyponatremia and hypercalcemia - Thyroid function. Pathophysiology remains unclear: 1. Reduced oxidative metabolism. 2. Neurotransmitters imbalance (reduced acetylcholine, dopamine, serotonin, GABA and noradrenaline). Dysfunction in central cholinergic transmission causes changes in arousal, attention and memory. Cerebrospinal fluid acetylcholinesterase levels correlate to life expectancy after delirium episodes. Neuroanatomical structed affected during delirium: 1. Frontal cortex. 2. Anteromedial thalamus. 3. Right basal ganglia 4. Right posterior parietal cortex. 5. Mesial-basal temporooccipital cortex.
|
|
Leonard at al./Ireland/2008 [5] |
[Review]
Patients receiving palliative care |
Pathophysiology of delirium in Palliative Care patients has not been studied properly. 1. Genetic predisposition to delirium (related to Apo lipoprotein E). 2. Opioid and psychoactive medication side effects. 3. Elevated inflammatory markers and immunological changes related to cancer: high cytokine levels, elevated C-reactive protein and neuronal apoptosis markers. 4. Low acetylcholine levels
|
|
Caraceni at al./Italy/2009 [17] |
[Review]
Hospitalized oncological patients |
Physiopathology: toxic effect of medication and neurotransmitters dysfunction (mainly acetylcholine) affecting: 1. Reticular formation of the brainstem. 2. Hypothalamus. 3. Thalamus 4. Cortex
|
|
Moyer at al./U.S./2011 [6] |
[Review]
Geriatric patients in end-of-life situation |
Delirium’s pathophysiological routes: 1. Neurotransmitter imbalance: acetylcholine deficiency and dopamine excess. Dopamine agonists and anticholinergic medication can lead to delirium. 2. Deregulation of the limbic-hypothalamic-pituitary-adrenal axis, meaning high cortisol levels. 3. Oxygen and glucose metabolism dysregulation affecting central nervous system. Others: - Space-occupying lesions in brain and cerebral edema. - Metabolic encephalopathy. - Sepsis. - Oxygen and fluid deprivation. - Electrolyte imbalance (hyponatremia, dehydration or hypercalcemia) and hypoglycemia. - Hepatic failure. - Sleep deprivation. - Poor pain management. - Fecal impaction and urinary retention. - Drug side effects (many times secondarily to dehydration). At the end of life, decreased renal and hepatic function can interfere with medication metabolism and excretion, potentially leading to harmful levels of medication in the body. Main reversible causes of delirium are medication toxicity and dehydration.
|
|
LeGrand at al./U.S./2012 [13] |
[Review]
Patients receiving palliative care |
Pathophysiology theories of delirium: 1. Decrease oxidative metabolism. 2. Neurotransmitter dysfunction (decreased acetylcholine levels, excess of dopamine and dysregulation in norepinephrine, GABA, glutamate and serotonin levels). This theory is validated by the fact that anticholinergic medication produces delirium-like symptoms (effects on memory, arousal, rapid eye moment, behavior, mood, orientation and perception) and slows electroencephalogram activity. Parallelly, serum acetylcholinesterase levels inform about severity of delirium and decrease when symptoms improve). Regarding to dopamine, this neurotransmitter decreases cholinergic activity (side effects of L-dopa and bupropion, which are dopaminergic drugs). 3. Age-related neurotransmitter levels changes (increased risk of delirium in elderly people due to lower acetylcholine levels). 4. Increased inflammatory cytokines. 5. Stress-induced blood-brain barrier reaction, meaning high hypothalamic-pituitary-adrenal axes activity. 6. Changes in intracellular transduction signals, translating into neurotransmitter synthesis and release.
|
|
Kang at al./U.S.-Republic of Korea/2013 [12] |
[Review]
Advanced cancer patients |
Delirium is caused by a global cerebral dysfunction, secondarily to: 1. Neurotransmitter imbalance (acetylcholine deficiency). Dopamine, serotonin and GABA. Activation of dopamine receptors D2-D4 decreases acetylcholine release. Serotonin interfere with dopamine and acetylcholine. Hypoxemia, infection, dehydration and electrolyte imbalance, decrease acetylcholine and increase dopamine. 2. Over reactive inflammatory response. Interleukin-6 and tumor-necrosis-factor-alpha by microglia activation and neurotoxicity (acetylcholine controls microglia) after transferring blood-brain barrier, produce 3. High cortisol levels with negative effects on hippocampal activity. Chronic stress produces pituitary-adrenal axis activation. Opioids, corticosteroids, benzodiazepines and serotonin agonists are most common drugs causing delirium when medication is found to be reason.
|
|
Grassi at al./Italy/2015 [8] |
[Review]
Patients receiving palliative care |
Pathophysiologic: - Underlying condition affecting on metabolism - Treatments, substance intoxication and drug withdrawal. - Neurotransmitter theory as pathophysiologic pathway of delirium (acetylcholine deficiency and dopamine excess). Antipsychotics action mechanism endorses this theory by inhibitory action on dopamine (D2 receptors) and neuroprotective effect on delta-1 receptor antagonism, reduction of oxidative stress and immunomodulation with indirect antagonism of interleukyne-1.
|
|
Bramati at al./U.S./2021 [10] |
[Review]
Patients receiving palliative care |
Main factors producing delirium: polypharmacy (opioids, corticosteroids, benzodiazepines, neuroleptics), hypercalcemia, hypoxemia, uremia, hyperammonemia, pneumonia, brain metastasis, leptomeningeal carcinomatosis and dehydration. Pathophysiology is based on: 1. “The systems integration failure hypothesis”, which explains neurotransmitter synthesis and availability disruption, leading to failure in different central nervous system functions (integration and processing) because of neuroinflammation, brain vascular dysfunction, altered brain metabolism and neurotransmitter imbalance (low acetylcholine levels, dopamine excess, glutamate and GABA alteration). 2. “Neuroinflammatory hypothesis”, related to inflammatory dysregulation with higher cytokines levels in Palliative Care. This results on neurotoxicity. 3. “Oxidative stress hypothesis”, increased oxidative stress products in Palliative Care patients with negative effect on central nervous system.
|
Table 1: Description of main aspects of reviews included during the research process.
Table of contents: Studies
|
Author/Country/Year
|
Article design/Population |
Objectives |
Intervention |
Results and conclusions |
|
Mortita at al./Japan/2003 [4] |
[Retrospective Cohort Study]
Terminally ill cancer patients (n=284) |
1. To assess communication capacity levels of terminally ill cancer patients at the end of life. 2. To identify factors contributing to communication capacity impairment and agitated delirium. |
To study daily hydration volume, doses of opioids, steroids and sedative medications during final week of life. |
Pathophysiology of delirium depends on underlying etiology. - Hepatic encephalopathy and advanced liver disease, (increase nitrogen levels, causing neurotoxicity) delirium. - Fentanyl and high serotonin levels have been observed to cause hepatic encephalopathy. - Hyperactive delirium associated with icterus and male gender.
|
|
Leonard at al./Ireland/2013 [7] |
[Longitudinal observational study]
Patients with diagnosed delirium (DSM-IV) receiving palliative care (n=100) |
1. To analyze most frequent and severe symptoms of delirium in palliative care. 2. To study symptom fluctuation pattern during delirium. 3. To estimate delirium’s rate change and evolution of cognition, composed inattention and cognitive deficits in delirium. |
Twice-weekly assessments using Delirium Rating Scale Revised-98 (DRS-98) and Cognitive Test for Delirium (CTD). |
Anatomical structures affected in delirium: thalamus, cortex and diencephalon. This disruptive functioning affects attention, cognition, circadian cycle and thinking. During delirium, neuronal processing for all higher cerebral cortical and subcortical functions is deteriorated. Main etiologies in PC: - Metabolic and endocrine disturbances, - Systemic infection - Drug intoxication. Neuroimaging studies and research show neurochemistry and neuroinflammation, induvial genetics and previous neuronal or physical susceptibilities, underlying delirium’s pathophysiology.
|
|
?enel at al./Turkey/2017 [9] |
[Prospective cohort study]
Terminal cancer patients admitted in palliative care (n=213) |
Better understanding of etiological, precipitating and risk factor for developing delirium in cancer patients admitted in palliative care. |
Diagnoses of delirium using Delirium Rating Scale (DRS) and Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV). |
- Temporary thalamic dysfunction by acetylcholine deficiency and dopamine excess. Serotonin, glutamate, cortisol, endogenous opioids and cytokines (IL-1, IL-6, IL-8, interferon and tumor necrosis factor) are also implicated in pathophysiology. - Organ failure conditions - Poor pain control - Drugs: benzodiazepines, opioids, steroids and anticholinergics.
|
|
Lawlor at al./Canada/2020 [15] |
[Double-blind, parallel, randomized, controlled, feasibility study]
Advanced cancer patients receiving palliative care (n=60)
|
Assessment of exogenous melatonin administration to prevent delirium in advance cancer patients. |
Daily melatonin 3mg or placebo orally at 21:00 over 28 days or less (in case of developing delirium, death, discharge or withdrawal antecedents. |
Delirium can be the clinical result of sleep-wake cycle disturbances and melatonin imbalance. |
Table 2: Description of main aspects of studies included during the research process.
Discussion
This systematic review aimed to investigate pathophysiology of delirium in terminally ill patients. In order to respond to proposed objectives, 18 papers were selected. Most studies highlight lack of investigation with high prevalence of this syndrome in this group of patients [2-19]. Regarding pathophysiologic theories, 12 articles state neurotransmitter dysfunction is involved in delirium’s development in these patients. There is evidence to suggest that low acetylcholine levels and excessive dopamine activity contribute to delirium. These chemicals pay key role in cognitive processes such as attention, arousal and memory [5,6,8-14,16,17,19]. Sustaining this theory, anticholinergic drugs are known to augment risk of delirium. Additionally, anticholinesterase drugs and antipsychotics, which respectively increase acetylcholine availability and block D2 dopamine receptors, have been found to be effective in treating delirium in some cases [6,8,9,13,16,17]. Furthermore, cerebrospinal fluid acetylcholinesterase levels during episodes have prognostic value (16). Oher involved neurotransmitters are serotonin, GABA, noradrenaline and glutamate
[4,9-14,16]. Different hypotheses accentuate terminal patients may be at increased risk of organ dysfunction. Renal and hepatic dysfunction impair drug metabolism and elimination, leading to drug toxicity. Neurotoxicity happens when noxious metabolites transfer blood-brain barrier and obstruct normal functioning of brain tissue. It is exacerbated by malnutrition and dehydration, conditions that are commonly seen in end-stage patients. This last situation creates a vicious circle: it entails to hypo perfusion which contributes to organ dysfunction and reinforce ineffective excretion of metabolites and neurotoxicity [2-4,6,9,11,14,18,19].
Polypharmacy and drugs as opioids, benzodiazepines, corticosteroids and anticholinergics happen to be a clear risk and precipitating factor for delirium [4,5,9-12,16]. Hyper metabolic states in advance cancer patients are also related. When this stress is severe or prolonged leads to excessive oxygen consumption. Oxidative stress damages cells and interfere physiological homeostasis (brain is the most sensible tissue towards oxidative stress) [10,13,16]. In response, pineal gland releases cortisol which has an inverse relationship with melatonin. Chronic stress can disrupt sleep-wake cycle causing terminal restlessness. Sleep dysregulation is a known precipitating factor for developing delirium [6,9,11,12,15]. Hypo/hypernatremia, hypercalcemia, increased cytokines and hypoxia provide hints to underlying delirium episode [6,10-12,16,18,19]. Another known pathophysiological pathway is genetic predisposition to this condition [5,7]. Affected anatomical structures are frontal, parietal and temporo-occipital cortex, thalamus, brain-stem reticular formation, right basal ganglia and hypothalamus [6,7,9,13,16,17].
This review has several limitations. There is lack of published studies regarding the main subject. Funding in palliative care can be limited due to several reasons: there is little economic incentive for investing in research when it is aimed to improve quality of life rather than developing new curative treatments. Secondly, research is difficulted as a result of ethics; patients’ autonomy and limitation of medical effort should not be forgotten. Furthermore, it can be challenging to find a correct population according to inclusion criteria and sufficient sample sizes to draw meaningful conclusions because of low life expectancy. End-stage illness involves complex interventions in conformity with every patient’s will and needs, making difficult to standardized outcome measures (it is not always possible to compare studies and draw conclusions) [20-23]. Most of the papers included were reviews from previous studies without delirium’s pathophysiology as main subject. Among the four selected studies, only one is a double-blind randomized controlled trial, which is the most reliable method thanks to control group presence, transparency and replicability. In contrast, the other three studies are observational, which means their methodology is susceptible to missing data, inherently increasing risk of bias. Specifically speaking about delirium, is a condition that is often underdiagnosed or misdiagnosed, especially in critically ill patients. Variety of symptoms makes it difficult to be diagnosed. Other reasons are lack of awareness and training among healthcare providers about this condition, interpretation of delirium as a natural part of aging process and that terminally ill patients may be more likely to be underdiagnosed due to complex medical conditions and multiple comorbidities [24,25]. Selection, sampling and measurement bias may be introduced.
Conclusion
Pathophysiology of delirium is complex and multifactorial. Most influential theories talk about neurotransmitter imbalance (acetylcholine deficiency and dopamine excess), organ dysfunction, sleep-wake cycle dysregulation and prolonged stress and inflammatory state which damages tissue functioning.
Drugs, polypharmacy, infections, electrolyte imbalances, hypoxia, dehydration, pain or social conditions may precipitate delirium in predisposed patients. Scientific knowledge found in literature is mostly based on retrospective studies. More research is needed to fully comprehend pathophysiology of delirium in terminally ill patients to develop effective prevention and management strategies, ensuring patient's care goals at all times.
References
- World Health Organization (2023) ICD-11 for Mortality and Morbidity Statistics [Internet].
- Ross DD, Alexander CS (2001) Management of common symptoms in terminally ill patients: Part II. Constipation, delirium and dyspnea. Am Fam Physician 64: 1019-26.
- Bruera E, Neumann CM (1998) Management of specific symptom complexes in patients receiving palliative care. CMAJ Canadian Medical Association Journal 158: 1717-26.
- Morita T, Tei Y, Inoue S (2003) Impaired communication capacity and agitated delirium in the final week of terminally ill cancer patients: Prevalence and identification of research focus. J Pain Symptom Manage 26: 827-34.
- Leonard M, Agar M, Mason C, Lawlor P (2008) Delirium issues in palliative care settings. J Psychosom Res 65: 289-98.
- Moyer DD (2011) Terminal delirium in geriatric patients with cancer at end of life. American Journal of Hospice and Palliative Medicine 28: 44-51.
- Leonard M, Adamis D, Saunders J, Trzepacz P, Meagher D (2013) A longitudinal study of delirium phenomenology indicates widespread neural dysfunction. Palliat Support Care 13: 187-96.
- Grassi L, Caraceni A, Mitchell AJ, Nanni MG, Berardi MA, et al. (2015) Management of Delirium in Palliative Care: a Review. Curr Psychiatry Rep 7: 550.
- Senel G, Uysal N, Oguz G, Kaya M, Kadioullari N, et al. (2017) Delirium Frequency and Risk Factors Among Patients With Cancer in Palliative Care Unit. American Journal of Hospice and Palliative Medicine 34: 282–6.
- Bramati P, Bruera E (2021) Delirium in palliative care. Cancers (Basel) 13: 5893.
- Lawlor PG (2002) Delirium and dehydration: Some fluid for thought? Support Care Cancer 10: 445-454.
- Kang JH, Shin SH, Bruera E (2013) Comprehensive approaches to managing delirium in patients with advanced cancer. Cancer Treat Rev 39: 105-112.
- LeGrand SB (2012) Delirium in palliative medicine: A review. J Pain Symptom Manage 44: 583-94.
- Lagman RL, Davis MP, LeGrand SB, Walsh D (2005) Common symptoms in advanced cancer. Surgical Clinics of North America 85: 237-255.
- Lawlor PG, McNamara-Kilian MT, MacDonald AR, Momoli F, Tierney S, et al. (2020) Melatonin to prevent delirium in patients with advanced cancer: a double blind, parallel, randomized, controlled, feasibility trial. BMC Palliat Care 19: 1.
- White C, McCann MA, Jackson N (2007) First do no harm... terminal restlessness or drug-induced delirium. J Palliat Med 10: 345-351.
- Caraceni A, Simonetti F (2009) Palliating delirium in patients with cancer. Lancet Oncol 10:164-72.
- Friedlander MM, Yanina B, Breitbart WS (2004) Delirium in palliative care. Oncology 18: 1541-1550.
- Yennurajalingam S, Braiteh F, Bruera E (2005) Pain and terminal delirium research in the elderly. Clin Geriatr Med 21: 93-119.
- O’Malley G, Leonard M, Meagher D, O’Keeffe ST (2008) The delirium experience: A review. J Psychosom Res 65: 223-228.
- EAPC [Internet] (2023) European Association for Palliative Care.
- de la Cruz M, Fan J, Yennu S, Tanco K, Shin SH, et al. (2015) The frequency of missed delirium in patients referred to palliative care in a comprehensive cancer center. Supportive Care in Cancer [Internet]. 23: 2427-33.
- Noble S, Noble M (2015) Emergencies in palliative care. Medicine 43: 722-5.
- Cleeland CS (2000) Cancer-related symptoms. Semin Radiat Oncol 10: 175-90.
- Bush SH, Bruera E, Bush S (2023) The Assessment and Management of Delirium in Cancer Patients; The Assessment and Management of Delirium in Cancer Patients.
Citation: Nabal Vicuña M and Moreno Giroud C (2023) Pathophysiology of Delirium in End-of-Life Patient: A Systematic Review. J Hosp Palliat Med Care 5: 021.
Copyright: © 2023 María Nabal Vicuña, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.