
Patterns of Alcohol Consumption Data Over 21 Years Following Hospitalization for Alcohol Use Disorder
*Corresponding Author(s):
Collins E LewisWashington University School Of Medicine, Department Of Psychiatry, United States
Tel:+1 3142862234,
Email:lewisco@psychiatry.wusl.edu
Abstract
Background
Alcohol use disorder is a chronic disease, and the consumption of alcohol after treatment is an integral part of the disease process. However, drinking alcohol itself is not a disorder; persistent problematic drinking is. This paper assesses the stability of the yearly drinking patterns of individuals with alcohol use disorder after discharge from psychiatric hospitalization for Alcohol Use Disorder (AUD).
Methods
A sample of 259 men and women hospitalized in 1967-68 with a diagnosis of probable or definite alcohol use disorder by Feighner Criteria was followed over 21 years. Of the survivors, 96 (82.1%) completed follow-up interviews and 76 (65.0%) had yearly drinking pattern data available for the entire 21 years. Yearly drinking patterns were analyzed for the proportions maintaining them for >5 years and for the mean maximum number of consecutive years for each pattern.
Results
This follow-up cohort represented a less severely affected group of problem drinkers than had been admitted to the study. Abstinence, occasional-social, regular-heavy, and very-heavy or binge drinking were the most stable patterns of consumption in that between 19.7% to 44.7% of the patients maintained these patterns for >5 consecutive years and the mean maximum durations were between from 2.7 and 7.3 years. Frequent-social and regular-light drinking were the least stable (0% to 6.6% and 0.0 to 0.9 years respectively). Approximately 89% of the patients consuming alcohol at a regular-heavy or higher level did so within a year after hospital discharge.
Conclusion
Occasional-social drinking was the most stable and least pathological, non-abstinent, drinking pattern. Frequent-social and regular-light drinking were the least stable patterns and had a high likelihood of leading to more serious, pathological consumption. The marked instability of regular-light drinking suggests that tolerance and alcohol-related cue exposure may be important components of relapse.
Keywords
Alcohol use disorder; Moderate drinking; Relapse; Tolerance; Withdrawal
INTRODUCTION
“Addiction [is] a chronic relapsing brain disease,” [1] and “post-treatment drinking is not the exception but the norm” [2]. Miller and coworkers reported that an average of 24% of individuals with Alcohol Use Disorder (AUD) maintained abstinence for >12 months after treatment, 10% engaged in moderate asymptomatic drinking, and the remainder had some heavy drinking with reduced problems [3]. The consumption of alcohol itself is not a disorder; however, its persistent problematic consumption is [4]. A medical relapse is the return of a disease after its apparent cessation or after an interval of improvement [5,6]. Marlatt’s definition of a behavioral relapse is “failure to maintain behavior change over time: a breakdown or setback in the person’s attempt to change or, modify a target behavior” [7]. In alcohol use disorder, that target behavior is persistent problematic drinking.
Pattison pointed out that “abstinence is not the only goal of alcohol rehabilitation” and that “other goals include improvement in emotional, interpersonal, vocational and physical health.” He also noted that “abstinence is not necessarily correlated with improvement in life health” and that “some alcoholics do not become abstinent, yet demonstrate major improvements in all areas of life function.” He pointed out that studies have shown a low correlation between improvement in alcohol consumption and improvement in those four areas of life function. Thus, two major goals of AUD treatment are: 1) identifying the areas of life dysfunction caused by alcohol and 2) establishing a goal to alleviate them. This approach provides both individualized treatment goals, and includes both abstinence and non-abstinence [8].
Recent follow-up studies have supported this approach. Wilson and coworkers used 12 month post-baseline COMBINE (Combined Pharmacotherapies and Behavioral Interventions) data and 15 month post-baseline Project MATCH (Matching Alcoholism Treatments to Client Heterogeneity) data to investigate post-treatment psychosocial function in binge drinkers (>5 drinks per day for men and >4 for women) and non-binge drinkers (individuals with light drinking or abstinence). Latent profile analysis divided the subjects into low, average, and high functioning with respect to alcohol consequences, health, Quality of Life (QoL), mental health, and social functioning. They reported that a substantial number of high-functioning binge drinkers exhibited “equal or better” psychosocial functioning than the abstinent and light drinkers despite having more alcohol-related negative consequences. The investigators pointed out that occasional post-treatment binge drinking may not impair psychosocial improvement and that post-treatment alcohol consumption criteria may not be as relevant in recovery as improvement in psychosocial functioning [9].
Witkiewitz and coworkers used project MATCH data in latent profile analysis to classify patients into 4 profiles at 3 years after outpatient treatment: (1) poor-functioning, frequent-heavy drinkers, (2) poor-functioning, infrequent-heavy drinkers, (3) high-functioning, occasional-heavy drinkers, and (4) high-functioning, infrequent non-heavy drinkers. Comparing the high-functioning, occasional-heavy drinkers (67.9% drinking days and 5.9 drinks per drinking day) with high-functioning, infrequent non-heavy drinkers (6.9% drinking days and 2.1 drinks per drinking day) revealed that even though the occasional-heavy drinkers had heavier alcohol consumption with more negative consequences than the infrequent non-heavy drinkers, their psychosocial functioning was comparable. This analysis also indicated that drinking status after treatment provided incomplete information about an individual’s psychosocial functioning and that certain individuals with heavy drinking may function as well as those who were mostly abstinent [10].
There has been much debate in the alcohol treatment community concerning post-treatment alcohol consumption, and guidelines have been proposed for controlled drinking as a treatment goal. The bases for considering post-treatment controlled drinking are: an absence of severity (e.g. no severe medical nor legal problems), client refusal to consider abstinence, prior failures in abstinence-oriented treatment, and strong occupational demands for alcohol consumption [11,12].
Researchers have evaluated and formulated criteria for controlled drinking, and certain treatment programs have accepted controlled drinking as a viable outcome. Investigators have addressed the quantity of alcohol that may be safely consumed in a day and in a week, the time of day of consumption, situations in which alcohol should not be consumed, the importance of not using alcohol as a coping device, the importance of ingesting food with alcohol consumption, refraining from more than one drink within half an hour, avoidance of excessive or secret drinking, and avoidance of daily drinking. Additional guidelines have also emphasized the need to keep the Blood Alcohol Level (BAL) below 55mg% [13-21].
This current analysis is unique in that it does not address the problems associated with post-treatment alcohol consumption but investigates the temporal stability of abstinence and five patterns of alcohol consumption over a 21-year follow-up period in a subset of patients who had been psychiatrically hospitalized for AUD. This evaluation of alcohol consumption stability allows for the differentiation of stable non pathological consumption and the initiation of unstable consumption leading to pathological consumption.
This study used the order of drinking severity as defined in the Home Environment and Lifetime Psychiatric Evaluation Record (HELPER) [22] and hypothesized that frequent-social drinking (consuming <3 drinks per day, 3-4 days per week or consuming >3 drinks per day, 1-2 days per week or intoxication 4-11 times per year) would represent the first unstable pattern. Pattern stability was defined by the proportion of individuals able to maintain pattern for >5 years and by the mean maximum consecutive year duration of a given pattern.
METHODS
The baseline research sample included 259 patients hospitalized in a public or private psychiatric hospital in nearly equal proportions in St. Louis for treatment of alcohol use disorder in 1967-68 [23,24]. A 21-year follow-up study was conducted in 1989-91. At follow up, 142 (54.8%) of the baseline participants were verified as deceased with a death certificate, and 117 (45.2%) were confirmed alive. Among these 117 known survivors, follow-up interviews were completed by 96 (82.1%), and 76 (65.0%) had yearly drinking pattern data available for the entire 21 years. These 76 surviving patients with complete follow-up data provide the sample for these analyses. Because of the constraint of >21 years of post-treatment survival, this sample was younger and less medically debilitated than the original participants admitted to the study.
During the baseline hospitalization, the study participants received a structured psychiatric interview focused on alcohol use history, including the extent and time sequence of problem drinking, periods of abstinence, consequences of alcohol use, chronology of development of psychiatric symptoms, and family history. Complementary collateral interviews were conducted with all available first-degree relatives, or with the closest available family member if a first-degree relative was not available, to confirm the information provided by the patient. Participants’ pertinent medical and psychiatric records were also reviewed. Further details of the methods are provided in earlier work published from this study [25-27].
Data obtained at the baseline interview provided demographic variables (gender, ethnicity, age, marital status, private vs. public hospital of ascertainment, and a parental or sibling history of problem drinking) and diagnostic classification. Married status was classified as living with a partner in a committed relationship, including common-law marriage.
Because the baseline study was conducted before the 1980 advent of the empirically-based Diagnostic and Statistical Manual for Mental Disorders, Third Edition (DSM-III), the baseline diagnostic assessment was conducted with structured interviews using Feighner-based criteria [28]. The DSM criteria from DSM-III onward are very similar to-and are based on-the criteria used for the baseline diagnostic assessment [29]. Baseline drinking severity variables included counts of Feighner alcohol symptoms and alcohol-related medical problems, lifetime proportion taken up by problem drinking, lifetime problem-drinking magnitude (the sum of Feighner symptom and medical problem counts multiplied by the number of problem-drinking years), and problem-drinking intensity (the sum of Feighner symptom and medical problem counts divided by the number of problem-drinking years).
All patients in the baseline sample met Feighner criteria for a diagnosis of probable or definite alcohol use disorder, summarized as patterns of alcohol consumption interfering with psychosocial functioning, as evidenced by job loss, two or more non-traffic arrests, marital separation or divorce, or hospitalization related to drinking other than the index admission [28]. Other diagnoses assessed were Antisocial Personality Disorder (ASP) [30,31], affective disorder [32], schizophrenia [33], panic disorder [34], obsessional disorder [35] and somatization disorder [36]. Drug use disorder was defined by withdrawal, hospitalization for abuse or withdrawal, and prolonged use of drugs.
According to the diagnostic classification schema at baseline, all patients were eligible for one diagnosis in addition to alcohol use disorder. Three baseline diagnostic groupings were established: 1) alcohol use disorder only (no other diagnosis identified besides alcohol use disorder); 2) alcohol use disorder with non-ASP comorbidity (any diagnosis present along with alcohol use disorder other than ASP); and 3) alcohol use disorder with ASP comorbidity (ASP diagnosed along with alcohol use disorder).
For the follow-up study, a structured psychiatric interview, the National Institute of Mental Health Diagnostic Interview Schedule for DSM-III-R [37], was utilized with expanded sections on alcohol and drug use, health, work, and marital and family history from the HELPER. To determine alcohol consumption patterns by year over the follow-up period, participants were asked to estimate the number of days per week that they drank, the number of drinks per drinking day, the number of intoxications per year, personal problems caused by alcohol, and age of onset and recency of each of these variables. The HELPER specified 7 categories of consumption. This analysis combined the very heavy and binge drinking categories. The HELPER regular or heavy drinking category is herein presented as simply “regular-heavy drinking” because it has a maximum of 14 drinks per week, which has been determined to be a high-risk level for men [38].
Table 1 provides the specifics of each of these drinking patterns in terms of drinking days per week, number of drinks per drinking day, number of drinks per week, and number of intoxications per year for each pattern. Drinking patterns were categorized for each follow-up year as the highest level of alcohol consumption in that year in the following categories:
- Abstinence (no drinking);
- Occasional-social drinking (<3 drinks per day, 1-2 days per week; or intoxication <4 times per year);
- Frequent-social drinking (<3 drinks per day, 3-4 days per week; or >3 drinks per day, 1-2 days per week; or intoxication 4-11 times per year);
- Regular-light drinking (1 drink only 5-7 days per week with no intoxication);
- Regular-heavy drinking (<3 drinks per day 5-7 days per week, >3 drinks per day >3 days per week; or intoxication >12 times per year but < weekly);
- Very-heavy drinking (>7 drinks per day >1 times per week; or weekly intoxication) or binge drinking (staying intoxicated for >2 days and then drinking nothing at all for weeks or months before the next binge).
|
Drinking Pattern |
# Drinking Days/Week |
# Drinks/Drinking Day |
# Drinks/Week |
# Intoxications/Year |
|
Abstinence |
0 |
0 |
0 |
0 |
|
Occasional-social |
1-2 |
1-2 |
1-4 |
<3 |
|
a. Frequent-social |
3-4 |
1-2 |
3-8 |
4-11 |
|
b. Frequent-social |
1-2 |
>3 |
>3 |
4-11 |
|
Regular-light |
5-7 |
1 |
5-7 |
0 |
|
a. Regular-heavy |
5-7 |
1-2 |
5-14 |
12-52 |
|
b. Regular-heavy |
3-7 |
>3 |
>9 |
12-52 |
|
a. Very-heavy |
1-7 |
>7 |
>7 |
>52 |
|
b. Binge |
-- |
-- |
-- |
>2 consecutive days of intoxication |
Table 1: Detailed descriptions of alcohol consumption patterns.
STATISTICAL ANALYSIS
Data analysis was conducted using SAS 9.4 [39]. Descriptive data are provided with counts and percentages, and with means and standard deviations. Comparisons of two categorical variables were completed using chi-squared tests, substituting Fisher’s exact tests for instances with expected cell sizes <5. Comparisons of dichotomous and numerical variables were completed using t-tests, with Satterthwaite analysis for instances of inequality of variance. Level of statistical significance was set as alpha=0.05.
Analysis of variance using Duncan’s multiple range test was conducted to examine patterns of alcohol consumption during periods of the study’s follow up. Comparison of two alcohol consumption patterns with one another was conducted with Wilcoxon Rank Sum tests [39].
RESULTS
Baseline characteristics of the sample
Table 2 provides baseline characteristics of the 76 study participants who constitute the sample for this article. There was a slight preponderance of males, and the Mean (SD) years of age was 34.8 (9.8). More than three-fourths were white, nearly one-half were currently married, and half were blue-collar workers. The largest baseline comorbid diagnostic category was alcohol use disorder with non-ASP comorbidity, constituting more than one-half of the sample. The 76 surviving participants with complete follow-up data did not differ significantly from the 41 surviving baseline participants without complete follow-up data in regard to sex, age, race, married status, employment status, or proportion with a diagnosis of alcohol use disorder without a comorbid psychiatric disorder.
|
Baseline Variables |
% (n) |
|
Total N |
100% (76) |
|
Age |
34.8 (9.8) |
|
Gender |
|
|
Male |
55.3 (42) |
|
Female |
44.7 (34) |
|
Race |
|
|
Caucasian |
76.3 (58) |
|
African-American |
23.7 (18) |
|
Marital status |
|
|
Currently married |
47.4 (36) |
|
Divorced or separated |
27.6 (21) |
|
Widowed |
1.3 (1) |
|
Never married |
23.7 (18) |
|
Occupational status |
|
|
White collar |
7.9 (6) |
|
Blue collar |
50.0 (38) |
|
Student |
5.3 (4) |
|
Housewife |
15.8 (12) |
|
Unemployed |
21.1 (16) |
|
Financial aid |
40.8 (31) |
|
Psychiatric facility |
|
|
Private |
51.3 (39) |
|
Public |
48.7 (37) |
|
Diagnosis group |
|
|
Alcohol use disorder without comorbidity |
22.4 (17) |
|
Alcohol use disorder with non-ASP comorbidity |
59.2 (45) |
|
Alcohol use disorder with ASP comorbidity |
18.4 (14) |
Table 2: Baseline characteristics of surviving participants with complete follow-up data.
Post-treatment drinking patterns
Most (63/76, 82.9%) participants with complete follow-up data for all 21 follow-up years had consumed alcohol in regular-heavy and very-heavy or binge patterns for at least one year, and most (88.9%) of these 63 did so within the first year after discharge from the hospital. Over the entire 21-year follow-up period, only 6 participants (7.9%) were completely abstinent; 4 (5.3%) consumed in an occasional-social pattern or were abstinent; 1 (1.3%) consumed in occasional-social and frequent-social patterns; 1 (1.3%) consumed in an occasional-social level; and 1 (1.3%) consumed in a frequent-social pattern.
Stability of post-treatment drinking patterns
Table 3 shows the proportions of participants with >5 consecutive years in each drinking pattern and the average maximum number of consecutive years of each pattern. The proportions sustaining >5 consecutive years in each pattern differed significantly across the patterns (c2=73.96, df=5, p<0.001). Abstinence and very-heavy or binge drinking patterns had the highest proportions, and frequent-social and regular-light drinking patterns had the lowest. The occasional-social category had a significantly higher proportion with >5 consecutive years than both the frequent-social (c2=6.69, df=1, p=0.010) and the regular-light categories (Fisher’s exact 2-tailed p<0.001). The frequent-social pattern had a non-significantly higher proportion with >5 consecutive years than the regular-light pattern (Fisher’s exact 2-tailed p=0.058).
|
Drinking Pattern |
% (n) with >5 Years in Pattern |
Mean (SD) of Maximum # Consecutive Years in Pattern |
|
Abstinence |
43.4 (33) |
6.7 (7.8) |
|
Occasional-social |
21.1 (16) |
2.7 (5.7) |
|
Frequent-social |
6.6 (5) |
0.9 (3.4) |
|
Regular-light* |
0.0 (0) |
0.0 (0.2) |
|
Regular-heavy |
19.7 (15) |
2.5 (4.9) |
|
Very-heavy or binge |
44.7 (34) |
7.3 (8.4) |
Table 3: Proportions with >5 consecutive years in drinking patterns and average maximum number of consecutive years in each pattern.
Note: *One individual sustained regular-light drinking for 2 years, and the other 75 individuals sustained this drinking pattern for 0 years, yielding a mean maximum consecutive years of regular-light drinking of exactly 03 years (approximately 11 days) for the entire sample.
Percentage with >5 consecutive years in drinking pattern: χ2=73.96, df=5, p<0.001
Occasional-social drinking vs. frequent-social drinking: χ2=6.69, df=1, p=0.001
Occasional-social drinking vs. regular-light drinking: Fisher’s exact 2-tailed p<0.001
Frequent-social drinking vs. regular-light drinking: Fisher’s exact 2-tailed p=0.058
Mean maximum consecutive years pattern: F=20.14, df=5, p<0.001
Abstinence vs. occasional, frequent-social, and regular-light drinking: z=5.82, p<0.001
Very-heavy or binge drinking vs. occasional-social, frequent-social, and regular-light drinking: z=7.08, p<0.001
Occasional-social drinking vs. regular-light drinking: z=3.89, p<0.001
The maximum mean number of consecutive years in each pattern differed significantly across the patterns (F=20.14, df=5, p<0.001). The maximum number of consecutive years of abstinence and very-heavy or binge drinking did not differ significantly, but both were significantly greater than the remaining patterns (abstinence z=5.82, p<0.001; very-heavy or binge drinking z=7.08, p<0.001). The maximum number of consecutive years spent in occasional-social drinking was significantly greater than in regular- light drinking (z=3.89, p<.001). Figure 1 shows the proportions of individuals able to maintain >5 consecutive years in each pattern and figure 2 shows the maximum time spent in each pattern.
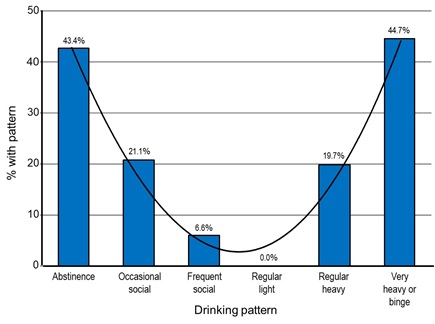 Figure 1: Proportions with >5 consecutive years for each drinking pattern.
Figure 1: Proportions with >5 consecutive years for each drinking pattern.
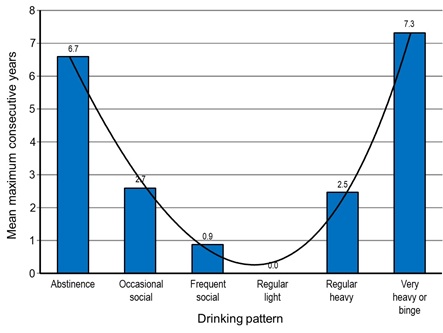 Figure 2: Mean maximum consecutive years in follow-up drinking patterns.
Figure 2: Mean maximum consecutive years in follow-up drinking patterns.
DISCUSSION
Relapse to problem drinking after treatment is a component of the addictive process; however, individuals with alcohol use disorder are known to be capable of consuming alcohol in a non-pathological manner, and moderate-drinking guidelines have been put forth [13-21]. This study analyzed the stability of post-treatment abstinence and the yearly patterns of consumption in individuals psychiatrically hospitalized for AUD. This study represents the first analysis of the stability of drinking patterns.
Stability of post-treatment drinking patterns
Drinking patterns in this study yielded bimodal curves. Abstinence and very-heavy or binge drinking were maximal at both ends and represented the two most stable patterns. Occasional-social and regular-heavy drinking represented the two intermediate patterns. Frequent-social and regular-light represented the two least stable patterns. The regular-heavy and very-heavy or binge drinking pattern with a minimum of 9 drinks per week and a maximum of 52 intoxications a year encompassed pathological levels of consumption where as occasional-social, frequent-social, and regular-light drinking with no more than 8 drinks per week were classified as non pathological.
Of these latter three drinking patterns, occasional-social drinking was the most stable with >20% maintaining it for >5 consecutive years; this pattern had a mean maximum duration of 2.7 years. Frequent-social and regular-light drinking were the least stable patterns. The former had only 7% maintaining it for >5 consecutive years and a maximum mean duration of <1 year, and the latter had none maintaining it for >5 consecutive years and a maximum mean duration of 0.0 years.
Occasional-social drinking with a maximum of 4 drinks per week was below the moderate weekly post-treatment consumption guidelines for AUD [13,18,21]; however, it did include 3 intoxications a year which are not in those guidelines. Because of its stability at a lower level of consumption, occasional-social drinking is defined in the current study as a non pathological pattern.
Frequent-social drinking with a minimum of 6 drinks per week and a maximum of 11 intoxications per year was classified as the beginning of relapse due to its aforementioned instability with only 7% maintaining it for >5 years and a mean maximum duration of <1 year. Regular-light drinking regularly consuming one drink a day was the most unstable pattern. None of the participants were able to maintain it for >5 years, and only one was able to maintain it for 2 years. Its marked instability also places it at the beginning of relapse.
The marked instability of regular-light drinking reflects the importance of alcohol tolerance and alcohol cues in relapse. Tolerance is a potent motivation to increase consumption to obtain the desired effect [40]. Protracted tolerance develops after a period of chronic drinking, may be carried over periods of abstinence, and may even develop more rapidly with the exposure to ethanol [41]. Some animal models demonstrated that rats receiving daily doses of alcohol developed greater tolerance and lost it more rapidly than rats receiving 3-day dosing cycles [42]. However, others showed a more rapid development of tolerance with repeated cycles [43,44]. The current study indicated daily or near daily consumption of one drink may very well have led to more rapid development of tolerance than the less regular pattern of occasional-social drinking.
Alcohol cues such as the sight, smell, taste, associated cognitions, time of day, and proximity to locations of ethanol ingestion have been shown to evoke conditioned responses such as craving, salivation, and alcohol seeking and have been associated with relapse [45-47]. Seo and Sinha [48], pointed out that alcohol-associated cues and stress are major factors that trigger alcohol craving and relapse and that neuro adaptations in key brain regions of emotional regulation and decision-making interact with environmental factors to modulate alcohol-seeking behavior. The brain regions altered by alcohol that were significantly associated with craving were the Ventral Striatum (VS), Orbital Frontal Cortex (OFC), Anterior Cingulate Cortex (ACC) and medical Prefrontal Cortex (PFC). The regular consumption of one drink daily in the regular-light drinking pattern would result in more alcohol cue exposure than the consumption of a maximum of 2 drinks per day 1-2 days a week in the occasional-social drinking pattern.
Differences in treatment settings and in the definitions of post-treatment alcohol consumption have been two major issues in the evaluation of controlled drinking after treatment [49]. Witkiewitz discussed the “difficulties in establishing a cut point for low-risk drinking” and the “lack of an agreed upon definition of ‘treatment success’ for non consumption outcome measures” [50] and Maisto and coworkers also noted a lack of consistency in the consumption criteria for relapse [51]. Both pointed out that treatment outcome should focus less on post-treatment alcohol consumption and more on post-treatment quality of life. However, research has shown that more severely addicted individuals with either alcohol or drug use disorder have abstinence as a goal [52,53]. Indeed, post-treatment consumption is contraindicated for individuals with very severe dependence and with serious medical and psychiatric comorbidities, which also affect QoL.
Johnson and coworkers pointed out that individuals with alcohol use disorder and psychiatric comorbidity had lower QoL scores than those with only alcohol use disorder [54]. Schaar and Ojehagen reported that the improvement in QoL of individuals with either alcohol use disorder or drug use disorder and psychiatric comorbidity was significantly associated with the number of months abstinent and that it was related to a decrease in psychological and psychiatric symptoms [55].
Additional research has also pointed out that low QoL in AUD was also associated with female gender, unmarried status, living alone, low socioeconomic status, and minimal education and that individuals with long-term abstinence had greater improvements in QoL [56]. However, although QoL appeared to improve with both and a reduction in pathological drinking and abstinence, it may not have returned to premorbid levels and may not have reached that of individuals without alcohol use disorder [57].
Although the focus on the addictive behavior is a good starting point, it is not the endpoint. Laudet pointed out that recovery went beyond abstinence and included the long-term process of improvement in QoL which required a change in “attitudes, thinking, and behaviors.” Investigators noted that the longer the period of total abstinence, the more likely an individual would be able to focus on these
QoL aspects of recovery and that having achieved these, highly-valued QoL improvements makes relapse more devastating. In contrast, not having achieved these QoL improvements makes relapse more inviting [53].
Relapse of AUD is not just the consumption of alcohol itself but persistent problematic consumption that negatively affects the individual’s QoL. This analysis is consistent with prior research indicating that certain patterns of post-treatment alcohol consumption are more likely than others to lead to persistent problematic consumption. This study found that regular-light drinking (regularly consuming one drink a day) was the most unstable and that frequent-social drinking (consuming 2 drinks 3-4 days per week or consuming 3 or more drinks a day 1-2 days per week, or intoxication 4-11 times per year)was the second most unstable pattern. Occasional-social drinking was the most stable even though it included 3 intoxications per year. This pattern included consuming low amounts of alcohol on a weekly basis and higher amounts very infrequently. The infrequent consumption of alcohol appears to be crucial in that it likely lowers the development of tolerance and decreases cue exposure.
Strengths and limitations
This study had import ant methodological strengths, including systematic diagnosis at baseline hospitalization using established diagnostic criteria and systematic follow-up with high study retention during a long follow-up over more than two decades. Another strength was the collection of data on detailed drinking patterns each year over more than two decades.
Limitations of the study include the retrospective collection of data on yearly drinking patterns over the 21-year follow-up period which might be expected to diminish accuracy of recall, yet even with this limitation, the data yielded distinct patterns of alcohol consumption. Additionally, alcohol consumption patterns were not collected on the more than one-half of the sample that did not live through the follow-up period, and thus the findings of this study are limited to the less severe AUD patients who were able to survive for two decades and do not apply to all hospitalized patients with AUD. This study
did not examine the baseline characteristics of the individuals comprising each pattern of consumption. Although the data were collected decades ago, no other studies in this time have examined the post-treatment course of alcohol consumption in patients hospitalized for AUD in such detail; thus, this study provides important new knowledge not preciously available about long-term patterns of alcohol consumption after hospitalization for AUD.
Implications for clinical practice
Individuals with alcohol use disorder have unique mental, physical, and quality of life profiles. For some with severe medical conditions, abstinence is required for survival; for others, abstinence is not required; however, for all, decreased alcohol consumption is required for an improved QoL. Individuals with AUD need to understand that their bodies have changed and that the population drinking guidelines do not apply to them. This is the same way in which the population guidelines for sugar and salt intake do not apply for patients with diabetes and hypertension respectively. Their brain structure has changed with a higher tolerance for alcohol and a greater sensitivity to alcohol cues. By definition, their quality of life has decreased due to AUD, and they may have mental-health and physical comorbidities that are exacerbated by its consumption. Thus, each individual with AUD must identify the personal areas of life dysfunction caused by alcohol and establish goals to alleviate them. This approach provides individualized treatment including both abstinence and non-abstinence [8].
Although the occasional drinking pattern was found to be most stable for a less severe sample of individuals who were discharged from inpatient psychiatric treatment, this pattern is not universal for all post-treatment individuals with AUD. There have been difficulties in establishing a non-abstinent measure of drinking “success,” and for some individuals, only abstinence is indicated [8,50].
Future research
In the original sample admitted to the study, age, preadmission liver cirrhosis, and marital divorce and separation were significantly associated with time to death in men and age, preadmission binge drinking, delirium tremens, antisocial comorbidity, and post-treatment pathological drinking were significantly associated with time to death in women; however, these characteristics have not been analyzed in association with long-term post-treatment drinking patterns [26,27]. Further analyses of the baseline psychosocial and clinical variables of individuals in this sample at the time hospital admission, including psychosocial, comorbid medical and psychiatric disorders, and characteristics of the AUDs, will focus on their relationship to abstinence and drinking patterns identified in this study to provide information that may be used for the individualization of treatment.
Additional analysis is also required to determine the direction of changes in the drinking patterns. Did the most unstable patterns progress to higher or lower levels of consumption? Did regular-heavy or very-heavy and binge drinking lead to lower levels of consumption or abstinence? These analyses will be forthcoming from this study.
CONCLUSION
This study used drinking-pattern stability over a 21-year follow-up period to determine criteria for controlled drinking in 76 surviving patients hospitalized with AUD. The follow-up sample excluding those deceased over the follow-up period was younger and had less severe alcohol use disorder than the larger sample admitted to the original study. The 21-year patterns showed a bimodal distribution similar to that described by Gaul [58]. Abstinence and occasional-social drinking were at one end of the spectrum and regular-heavy and very-heavy or binge drinking were at the other. Frequent-social drinking and regular-light drinking were the least stable drinking patterns and pointed to the initiation regular-heavy, very-heavy, or binge drinking. Occasional-social drinking was the most stable pattern of consumption with only 1-2 drinking days per week, a maximum of 4 drinks per week and 3 intoxications per year. Occasional-social drinking consumption was below post-treatment consumption guidelines which did not include intoxication [13,18,21]. The data from this study paralleled other research reporting high functioning in certain binge-drinking and occasional-heavy drinking groups [9,10].
REFERENCES
- Volkow ND, Li TK (2005) Drugs and alcohol: Treating and preventing abuse, addiction and their medical consequences. Pharmacol Ther 108: 3-17.
- Miller WR (1996) What is a relapse? Fifty ways to leave the wagon. Addiction 91: 15-27.
- Miller WR, Scott W, Bennett ME (2001) How Effective is alcoholism treatment in the United States? J Stud Alcohol 62: 211-220.
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental disorders (DSM-5®). American Psychiatric Publishing, Washington, DC, USA.
- Dorland (2011) Dorland’s Illustrated Medical Dictionary 32nd Elsevier, Philadelphia, USA.
- Stedman's (2011) Stedman’s Medical Dictionary for the Health Professionals and Nursing. Lippincott Williams & Wilkins, New York, USA.
- Daley DC, Marlatt GA, Douaihy A (2005) Substance abuse: A comprehensive Lippincott Williams & Wilkins, New York, USA.
- Pattison EM (1976) Non-abstinent drinking goals in the treatment of alcohol use disorder. Arch Gen Psychiatry 33: 923-930.
- Wilson AD, Bravo AJ, Pearson MR, Witkiewitz K (2016) Finding success in failure: using latent profile analysis to examine heterogeneity in psychosocial functioning among heavy drinkers following treatment. Addiction 111: 2145-2154.
- Witkiewitz K, Wilson AD, Pearson MR, Montes KS, Kirouac M, et al. (2018) Profiles of recovery from alcohol use disorder at three years following treatment: Can the definition of recovery be extended to include high functioning heavy drinkers? Addiction 114: 69-80.
- Sobell MB, Sobell LC (1995) Controlled drinking after 25 years: How important was the debate? Addiction 90: 1149-1153.
- Miller WR, Caddy GR (1977) Abstinence and controlled drinking in the treatment of problem drinkers. J Stud alcohol 38: 986-1003.
- Kishline A (1994) The steps, in moderate drinking: The moderation management guide for people who want to reduce their drinking, Crown Trade Paperbacks, New York, USA.
- Sobell MB, Sobell LC (1973) Alcoholics treated by individualized behavior therapy: One year treatment outcome. Behav Res Ther 11: 599-618.
- Sanchez-Craig M, Annis HM, Bornet AR, MacDonald KR (1984) Random assignment to abstinence and controlled drinking: Evaluation of a cognitive-behavioral program for problem drinkers. J Consult Clin Psych 52: 390-403.
- Sanchez-Craig M, Wilkinson A, Davila R (1995) Empirically based guidelines for moderate drinking: 1-year results from three studies with problem drinkers. Am J Public Health 85: 823-828.
- McIntosh MC, Sanchez-Craig M (1984) Moderate drinking: An alternative treatment goal for early-stage problems drinking. Can Med Assoc J 131: 873-876.
- Sanchez-Craig M (2015) Saying when, how to quit drinking or cut. Centre for Addiction and Mental Health, Toronto, Canada.
- Vogler RE, Bartz WR (1982) The better way to drink. New Harbinger Publications, Inc., Oakland, USA.
- Rosenberg H (1993) Prediction of controlled drinking by alcoholics and problem drinkers. Psychol Bull 113: 129-139.
- Rotgers F (2002) Responsible drinking: A moderation management approach for problem drinkers with worksheet. New Harbingre Publications, Inc., Oakland, USA.
- Coryell W, Cloninger CR, Reich T (1978) Clinical assessment: Use of non-physician interviewers. J Nerv Mental Dis 166: 599-606.
- Schuckit M, Pitts FN, Reich T, King LJ Winokur G (1969) Alcoholism I: Two types of alcoholism in women. Arch Gen Psychiatry 20: 301-306.
- Rimmer J, Pitts FN, Reich T, King LJ Winokur G (1971) II: Sex socioeconomic status, race in two hospitalized samples. QJ Study Alcohol 32: 942-952.
- Lewis CE, Smith E, Kercher C, Spitznagel E (1995) Assessing gender interactions in the prediction of mortality in alcoholic men and women: A 20-year follow-up study. Alcohol Clin Exp Res 19: 1162-1172.
- Lewis CE, Smith E, Kercher C, Spitznagel E (1995) Predictors of mortality in alcoholic men: A 20-year follow-up study. Alcohol Clin Exp Res 19: 984-991.
- Smith E, Lewis CE, Kercher C, Spitznagel E (1994) Predictors of mortality in alcoholic women: A 20- year follow-up study. Alcohol Clin Exp Res 19: 1177-1186.
- Feighner JP, Robins E, Guze SB, Woodruff RA, Winokur G, et al. (1972) Diagnostic criteria for use in psychiatric research. Arch gen Psychiatry 26: 57-62.
- Surís A, Holliday R, North CS (2016) The evolution of the classification of psychiatric disorders. Behav Sci 6: 5.
- Guze SB, Wolfgram ED, McKinney JK, Cantwell DP (1967) Psychiatric illness in the families of convicted criminals: A study of 519 first-degree relatives. Dis Nerv system 28: 651-659.
- Guze SB, Tuason VB, Stewart MA, Picken B (1963) The drinking history: A comparison of reports by subjects and their relatives. Q J Stud Alcohol 24: 249-260.
- Cassidy WL, Flanigan NB, Spellman M, Cogen ME (1957) Clinical observations in manic-depressive disease: A quantitative study of one hundred manic-depressive patients and fifty medically sick controls. JAMA 64: 1535-1546.
- Langfeld G, Ettinger L, Loane CL (1958) The prognostic value of the clinical picture and the therapeutic value of physical treatment in schizophrenia and the schizophreniform states. Acta Psychiatr Scand 33: 33-55.
- Wheeler EO, White PD, Reed EW, Cohen ME (1950) Neurocirculatory asthenia (anxiety neurosis, effort syndrome, neurasthenia). JAMA 142: 878-888.
- Politt J (1957) Natural history of obsessional states. Br Med J 1: 194-198.
- Perly M, Guze SB (1962) Hysteria: The stability and usefulness of clinical criteria. N Engl J Med 266: 421-426.
- Robins LN, Helzer JE, Croughan J, Ratcliff KS (1981) National institute of mental health diagnostic interview schedule. Arch Gen Psychiatry 38: 381-389.
- Department of Health and Human Services and the US. Department of Agriculture. 2015-2020 Dietary Guidelines for Americans.
- SAS Software. Version 9.4, SAS Institute Inc., Cary, NC, USA
- Kalant HK (1996) Current state of knowledge about the mechanisms of alcohol tolerance. Addict Biol 1: 133-141.
- Cicero TJ (1980) Alcohol self-administration, tolerance and withdrawal in humans and animals: Theoretical and methodological issues. In Rigter H, Crabbe JC (eds.). Alcohol Tolerance and Dependence. (NY) Elsevier/North-Holland Biomedical Press, New York, USA.
- Pohorecky LA, Roberts P (1991) Development of tolerance to and physical dependence on ethanol: Daily versus repeated cycles treatment with ethanol. Alcohol Clin Exp Res 15: 824-833.
- Kalant HK, LeBlanc AE, Gibbins RJ, Wilson A (1978) Accelerated development of tolerance during repeated cycles of ethanol exposure. Psychopharmacology 60: 59-65.
- Maier DM, Pohorecky LA (1987) The effect of repeated withdrawal episodes on acquisition and loss of tolerance to ethanol in ethanol-treated rats. Physiol Behav 40: 411-424.
- Lowman C, Hunt WA, Litten RZ, Drummond DC (2000) Research perspectives on alcohol craving: An overview. Addiction 95: 45-54.
- Drummond DC (2000) What does cue-reactivity have to offer clinical research? Addiction 95: 129-144.
- Gaultier S, Drummond DC (1994) Alcohol dependence and cue reactivity. J Stud Alcohol 55: 224-229.
- Pfefferbaum A, Sullivan EV (2014) Alcohol and the Nervous System. Elsevier Science, New York, USA.
- Heather N, Tebbutt J (1989) Definitions of non-abstinent and abstinent categories in alcoholism treatment outcome classifications: A review and proposal. Drug Alcohol Depend 24: 83-93.
- Witkiewitz K (2013) “Success” following alcohol treatment: Moving beyond abstinence. Alcohol Clin Exp Res 1: 9-13.
- Maisto SA, Roos CR, Hallgren KA, Moskal D, Wilson A, et al. (2016) Do alcohol relapse episodes during treatment predict long-term outcomes? Investigating the validity of existing definitions of alcohol use disorder relapse. Alcohol Clin Exp Res 40: 2180-2189.
- Berglund, KJ, Svensson I, Berggren U, Balldin J, Fahlke C ((2016) Is there a need for congruent treatment goals between alcohol-dependent patients and caregivers? Alcohol Clin Exp Res 40: 874-879.
- Laudet AB (2007) What does recovery mean to you? Lessons from the recovery experience for research and practice. J Subst Abuse Treat 33: 243-256.
- Johnson JG, Spitzer RL, Williams JBW, Linzer M, deGruy F, et al. (1995) Psychiatric comorbidity, health status, and functional impairment associated with alcohol abuse and dependence in primary care patients: Findings of the PRIME MD-1000 study. J Consult Clin Psychol 63: 133-140.
- Schaar I, Ojehagen A (2003) Predictors of improvement in quality of life of severely mentally ill substance abusers during 18 months of co-operation between psychiatric and social services. Soc Psychiatry Psychiatr Epidemiol 38: 83-87.
- Ogochukwu C, Bagot KS, Delaloye S, Pi S, Vien L, et al. (2013) The importance of quality of life in patients with alcohol abuse and dependence. Harv Rev Psychiatry 21: 1-17.
- Donovan D, Mattson ME, Cisler RA, Longabough R, Zweben A (2005) Quality of life as an outcome measure in alcoholism treatment research. J Stud Alcohol Suppl 15: 119-139.
- Gaul A, Lligona A, Colom J (1999) Five-year outcome in alcohol dependence: A naturalistic study of 850 patients in Catalonia. Alcohol Alcoholism 34: 183-192.
Citation: Lewis CE, North CS (2020) Patterns of Alcohol Consumption Data Over 21 Years Following Hospitalization for Alcohol Use Disorder. J Addict Addictv Disord 7: 55.
Copyright: © 2020 Collins E Lewis, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

