
Journal of Orthopedic Research & Physiotherapy Category: Medical
Type: Research Article
Physical Activity, Physical Function and Fear of Falling After Hip Fracture
*Corresponding Author(s):
Wilco AchterbergDepartment Of Public Health And Primary Care, Leiden University Medical Center, Leiden, Netherlands
Tel:+31 715268412,
Email:W.P.Achterberg@lumc.nl
Received Date: May 03, 2017
Accepted Date: Jul 03, 2017
Published Date: Jul 18, 2017
Abstract
Background
Physical activity and physical function are reduced after hip fracture and Fear of Falling (FOF) is common. However, relationships between these factors have not been investigated in elderly persons rehabilitating after hip fracture.
Objective
To examine correlations between physical activity, physical function and FOF, and identify predictive factors of physical activity in elderly recovering from hip fracture.
Design
Cross-sectional study performed in ten skilled nursing facilities.
Methods
100 patients (aged ≥ 65 years) after a hip fracture were included. Activity was measured by calculating the number of steps by means of a pedometer. Function was measured with the Performance Oriented Mobility Assessment (POMA) and FOF with the Falls Efficacy Scale International (FES-I). Correlations were calculated for the i) Total patient group and for patients with ii) Low and iii) High FOF. Predictive factors for physical activity were identified by multivariate logistic regression.
Results
In all three groups, activity and function were the most strongly correlated (r=0.71, p<0.001; r=0.59, p<0.001; r=0.73, p<0.001). FOF was negatively correlated with activity and function in the i) total group and in the iii) high FOF group (r=-0.34, p=0.001; r=-0.43, p<0.001; r=-0.44, p<0.01; r=-0.62, p<0.001). Female gender and better physical function were independent predictors of physical activity (OR 5.77, 95% CI=1.28-26.02; OR 1.24, 95% CI=1.09-1.41).
Conclusion
Physical activity and physical function were more strongly related than activity and FOF, indicating the prominent role of physical function in rehabilitation. Women, and patients with better physical functioning, are likely to be more physically active. These results suggest that patients with high FOF may benefit from a combination of reducing FOF and improving physical skills. Patients with low FOF may benefit from enhancing physical function only.
Physical activity and physical function are reduced after hip fracture and Fear of Falling (FOF) is common. However, relationships between these factors have not been investigated in elderly persons rehabilitating after hip fracture.
Objective
To examine correlations between physical activity, physical function and FOF, and identify predictive factors of physical activity in elderly recovering from hip fracture.
Design
Cross-sectional study performed in ten skilled nursing facilities.
Methods
100 patients (aged ≥ 65 years) after a hip fracture were included. Activity was measured by calculating the number of steps by means of a pedometer. Function was measured with the Performance Oriented Mobility Assessment (POMA) and FOF with the Falls Efficacy Scale International (FES-I). Correlations were calculated for the i) Total patient group and for patients with ii) Low and iii) High FOF. Predictive factors for physical activity were identified by multivariate logistic regression.
Results
In all three groups, activity and function were the most strongly correlated (r=0.71, p<0.001; r=0.59, p<0.001; r=0.73, p<0.001). FOF was negatively correlated with activity and function in the i) total group and in the iii) high FOF group (r=-0.34, p=0.001; r=-0.43, p<0.001; r=-0.44, p<0.01; r=-0.62, p<0.001). Female gender and better physical function were independent predictors of physical activity (OR 5.77, 95% CI=1.28-26.02; OR 1.24, 95% CI=1.09-1.41).
Conclusion
Physical activity and physical function were more strongly related than activity and FOF, indicating the prominent role of physical function in rehabilitation. Women, and patients with better physical functioning, are likely to be more physically active. These results suggest that patients with high FOF may benefit from a combination of reducing FOF and improving physical skills. Patients with low FOF may benefit from enhancing physical function only.
INTRODUCTION
Many patients recovering from hip fracture do not reach pre-fracture functional or mobile levels [1,2]. This can have a negative effect on quality of life because physical activity, such as walking, is important for physical and mental health, and reduces the risk of many diseases such as coronary heart disease and type II diabetes mellitus [3,4]. Moreover, physical inactivity is associated with frailty and muscle weakness that are known risk factors for falling [5,6]. In addition, limitations in function and mobility, especially when comorbidity is involved, may increase the use of healthcare services or could even lead to admission to a residential care facility [7]. It has been shown that being physically active reduces the time needed to regain independence in Activities of Daily Living (ADL) in newly disabled older adults hereby stimulating self-sufficiency and social functioning [8]. This indicates the importance of physical activity in elderly who suffer from functional limitations such as hip fractures.
Physical function includes a variety of abilities such as mobility, balance, gait and ADL [9]. In elderly recovering from hip fracture besides the direct consequences of a fracture, physical function may further be reduced due to other factors including older age, lower cognitive status and several comorbidities and living in a residential care facility before fracture [10]. Physical function is an important outcome of rehabilitation after hip fracture because, as mentioned above, not many patients succeed in regaining their pre-fracture functional levels [11].
Fear of Falling (FOF) is associated with poor physical functioning and has been identified as an independent risk factor for disability [9,12-14]. FOF is common among elderly patients, especially in those with hip fractures [15]. After a hip fracture, the prevalence rates of FOF range from 59-68%, with the highest prevalence measured in the second four weeks after the fracture [15]. FOF is related to decreased physical activity, although this has not been confirmed in all studies [16-18].
The relations between physical activity, physical function and FOF have been studied in community-dwelling older adults [19]. It was found that FOF was significantly negatively correlated with physical function [19]. Furthermore, physical activity and physical function were significantly positively correlated; yet this relation was weaker than the relation between FOF and physical function [19]. The findings suggest that if a patient has many concerns about falling, he or she is likely to have limited physical function. Likewise, when a patient is less active, he or she is also likely to have limited physical function. The question remains whether physical activity, physical function and FOF are correlated in elderly patients rehabilitating after hip fracture, and if so, in what way. This is of importance to further develop and evaluate interventions for improving functional levels and activity in this patient population.
It is known that female genders, smoking and slow walking speed are independent predictors of cessation of physical activity in community-dwelling elderly [18]. Predictive factors of physical activity in older patients recovering from hip fracture are not known.
Therefore, the aim of this study was i) to examine the relations between physical activity, physical function and FOF and ii) to identify predictive factors of physical activity in elderly patients who are rehabilitating after hip fracture.
Physical function includes a variety of abilities such as mobility, balance, gait and ADL [9]. In elderly recovering from hip fracture besides the direct consequences of a fracture, physical function may further be reduced due to other factors including older age, lower cognitive status and several comorbidities and living in a residential care facility before fracture [10]. Physical function is an important outcome of rehabilitation after hip fracture because, as mentioned above, not many patients succeed in regaining their pre-fracture functional levels [11].
Fear of Falling (FOF) is associated with poor physical functioning and has been identified as an independent risk factor for disability [9,12-14]. FOF is common among elderly patients, especially in those with hip fractures [15]. After a hip fracture, the prevalence rates of FOF range from 59-68%, with the highest prevalence measured in the second four weeks after the fracture [15]. FOF is related to decreased physical activity, although this has not been confirmed in all studies [16-18].
The relations between physical activity, physical function and FOF have been studied in community-dwelling older adults [19]. It was found that FOF was significantly negatively correlated with physical function [19]. Furthermore, physical activity and physical function were significantly positively correlated; yet this relation was weaker than the relation between FOF and physical function [19]. The findings suggest that if a patient has many concerns about falling, he or she is likely to have limited physical function. Likewise, when a patient is less active, he or she is also likely to have limited physical function. The question remains whether physical activity, physical function and FOF are correlated in elderly patients rehabilitating after hip fracture, and if so, in what way. This is of importance to further develop and evaluate interventions for improving functional levels and activity in this patient population.
It is known that female genders, smoking and slow walking speed are independent predictors of cessation of physical activity in community-dwelling elderly [18]. Predictive factors of physical activity in older patients recovering from hip fracture are not known.
Therefore, the aim of this study was i) to examine the relations between physical activity, physical function and FOF and ii) to identify predictive factors of physical activity in elderly patients who are rehabilitating after hip fracture.
MATERIALS AND METHODS
Design and study population
A cross-sectional study of patients with hip fracture was conducted in ten Skilled Nursing Facilities (SNFs) in the Netherlands. Patients rehabilitating after hip fracture and aged 65 years or older were included during the period between September 2010 and March 2011. Hip fractures were defined as fractures of the cervical, the pertrochanteric and subtrochanteric area of the femur. Patients were excluded when they were unable to adequately reply to questions, did not give informed consent, or had communication problems. In each of the participating facilities data collection took place during a two-week period by two researchers, an elderly care physician and physiotherapists and through questionnaires for the nursing staff and physicians. Because data were collected cross-sectionally patients were assessed at any time between admission and discharge from the SNF.
The Medical Ethical Commission of the VU University Medical Center approved the study and protocol.
The Medical Ethical Commission of the VU University Medical Center approved the study and protocol.
Demographic and health-related data
Data were collected on age, gender (male vs. female), site of fall (indoors vs. outdoors), type of fracture (cervical, trochanteric, subtrochanteric, other/not known), kind of surgery (hemiarthroplasty, total arthroplasty, proximal femur nail or gamma nail, dynamic hip screw, surgical screws, other/not operated), fall history (no fall vs. fall), use of benzodiazepines (no vs. yes), use of antihypertensive drugs (no vs. yes), use of analgesics (including paracetamol and Non Steroidal Anti-Inflammatory Drugs (NSAIDs)) (no vs. yes), number of complications during rehabilitation, number of comorbidities, hearing impairment (no vs. yes), vision impairment (no vs. yes), and presence of dizziness (yes vs. no). Physicians obtained information on medication use, comorbidity and number of complications from medical records; nursing staff obtained information on fall history, hearing and vision impairment, and dizziness from questionnaires [20].
Physical activity
Physiotherapists obtained data on physical activity. Physical activity was defined as walking and was measured with a pedometer (the Digi-walker SW-200; Yamax) that measures vertical accelerations of the hip and translates these into number of steps. Despite the fact that a pedometer does not provide information on the duration of activities and does not measure the intensity of physical activity [21], it is considered a reliable instrument for measuring physical activity [21]. Patients wore the pedometer for one day, which was attached to their waistlines or belts, and physiotherapists documented the number of steps. The pedometer was detached only when a shower was taken.
Range values for steps in various populations, including adults with disabilities, have been identified [22]. A range of 3,500-5,500 steps per day can be considered normal for adults with disabilities (between 18 and 65 years of age) [22]. Normal range values for elderly with disabilities (over 65 years of age), such as hip fractures have not yet been determined. Mean number of steps per day or medians are often used to reliably assess physical activity [23-27]. Due to the lack of consensus on the cut-off values for the pedometer, the median score in this sample was used as a cut-off value for low or high physical activity [28].
Range values for steps in various populations, including adults with disabilities, have been identified [22]. A range of 3,500-5,500 steps per day can be considered normal for adults with disabilities (between 18 and 65 years of age) [22]. Normal range values for elderly with disabilities (over 65 years of age), such as hip fractures have not yet been determined. Mean number of steps per day or medians are often used to reliably assess physical activity [23-27]. Due to the lack of consensus on the cut-off values for the pedometer, the median score in this sample was used as a cut-off value for low or high physical activity [28].
Physical function
Data on physical function was also obtained by physiotherapists. Physical function was measured by means of the Performance-Oriented Mobility Assessment (POMA). The POMA is a reliable and validated performance-based instrument to measure balance and gait [29-31]. It consists of 16 items including 9 balance-related items and 7 gait-related items. Items are evaluated on an ordinal scale that ranges from 0 to 1 or from 0 to 2, with the highest total score being 28 points [32]. A general cut-off value is not known in elderly patients; a cut-off value of less than or equal to 17 has been shown to be associated with an increased risk of falls in patients with stroke [32].
Fear of falling
FOF was assessed by a research assistant who filled in the Falls Efficacy Scale International (FES-I). The FES-I is a reliable and valid method for measuring FOF [33]. The FES-I is a questionnaire containing 16 questions on concerns about falling while performing ADL tasks. Questions are evaluated on an ordinal scale which ranges from 1 not at all concerned to 4 very concerned. The total score can range from 16-64. Consensus on a cut-off point for the FES-I is not known; for example, Delbaere et al., defined a cut-off point of 23 while Ulus et al., calculated a cut-off point of 24 [34,35]. Hence, in the present study the median value was used as a cut-off point [28].
Depressive symptoms
Information on depressive symptoms was obtained by a researcher who interviewed patients and recorded the results by means of the Geriatric Depression Scale 8-item version (GDS-8) questionnaire. The GDS-8 is a reliable tool for detecting depressive symptoms in elderly living in nursing homes [36]. It is based on the GDS-15 and includes 8 questions [36].
In the present study a cut-off value of 3 was used because it has been shown that a cut-off point of 3 has high sensitivity and high specificity for detecting depression [36].
In the present study a cut-off value of 3 was used because it has been shown that a cut-off point of 3 has high sensitivity and high specificity for detecting depression [36].
Pain
A researcher asked the patients to score the severity of their pain by means of the Visual Analogue Scale (VAS). The VAS is a 10-cm long horizontal line on which patients can score the severity of their pain [37]. The scale ranges from 0 no pain to 10 worst pain ever [37]. The VAS is a valid tool for measuring pain at a given point in time which means that a single assessment suffices [37].
Statistical analysis
To analyze the characteristics of the patient population, descriptive statistics were calculated and data distribution for the different variables was assessed. To examine the relations between physical activity, physical function and FOF, Spearman correlations were calculated for the i) Total patient group, and for the patients with ii) Low FOF (<33) and iii) High FOF (≥33). A p-value of <0.05 was considered statistically significant.
Where possible, potentially predictive factors of physical activity were dichotomized. Each of the variables was then included in the univariate logistic regression analysis with steps per day as dependent outcome variable. Because it was expected that data for activity were not normally distributed low and high levels of activity were used. Variables with a p-value of <0.10 were considered statistically significant in the univariate analysis. Variables with a p<0.20 were selected and entered into a multivariate logistic regression model. Using a backward stepwise procedure, variables with a p-value of >0.10 were removed resulting in the final predictive multivariate model in which a p-value of <0.05 was considered statistically significant. Statistical analysis was performed with SPSS 20.
Where possible, potentially predictive factors of physical activity were dichotomized. Each of the variables was then included in the univariate logistic regression analysis with steps per day as dependent outcome variable. Because it was expected that data for activity were not normally distributed low and high levels of activity were used. Variables with a p-value of <0.10 were considered statistically significant in the univariate analysis. Variables with a p<0.20 were selected and entered into a multivariate logistic regression model. Using a backward stepwise procedure, variables with a p-value of >0.10 were removed resulting in the final predictive multivariate model in which a p-value of <0.05 was considered statistically significant. Statistical analysis was performed with SPSS 20.
RESULTS
Baseline characteristics
Of the 124 eligible patients, 13 were excluded because they were unable to adequately reply to questions, 6 did not give informed consent and 4 were excluded because of communication problems. One patient was excluded from the analysis because of incomplete data. This resulted in a study group of 100 patients (Figure 1). Data were collected on the 52nd day on average after hip fracture (median 44.5 days, IQR 28-63).
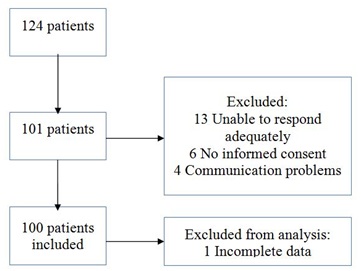
Figure 1: Flow chart of the study population.
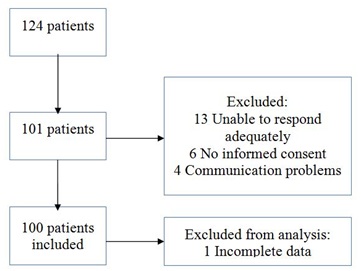
Figure 1: Flow chart of the study population.
Table 1 presents the characteristics of the i) total study population and of the subgroups for ii) low FOF and iii) high FOF including descriptive statistics for each of the variables. Mean age was 83.1 (SD 8.3) years and 75% of the study population was female. Median score for steps per day was 259.5 (IQR 76.8-606.8) and median score for physical function was 17.5 (IQR 13-22). The median score for FOF was 32.2 (IQR 24-39).
| i) Total group n=100 | ii) Low FoF (FES-I <33) n=50 | iii) High FoF (FES-I >=33) n=50 | ||
| Age in years, mean (SD) | 83.1 (8.3) | 81.9 (8.5) | 84.3 (8.0) | |
| Female (%) | 75 | 72 | 78 | |
| Days after hip fracture, median (IQR) | 44.5 (28-63) | 48.5 (28-68) | 42.0 (28-55) | |
| Steps per day, median (IQR) | 259.5 (76.8-606.8) | 298 (135-743) | 126 (49-585) | |
| Fallen indoors (%) | 70 | 68 | 72 | |
| Fall history (%) | 10 | 8 | 12 | |
| Use of benzodiazepines (%) | 27 | 22 | 32 | |
| Use of antihypertensive drugs (%) | 62 | 64 | 60 | |
| Use of analgesics* (%) | 82 | 84 | 80 | |
| Number of complications during rehabilitation, mean (SD) | 1.6 (1.4) | 1.3 (1.1) | 1.9 (1.6) | |
| Number of comorbidities, mean (SD) | 3.5 (1.5) | 3.4 (1.6) | 3.6 (1.5) | |
| Depressive symptoms (GDS-8 ³3) (%) | 11 | 10 | 12 | |
| Hearing impairment (%) | 35 | 36 | 34 | |
| Visual impairment (%) | 27 | 20 | 34 | |
| Pain (VAS), mean (SD) | 2.7 (2.1) | 2.4 (2.1) | 3.0 (2.1) | |
| Dizziness (%) | 14 | 14 | 14 | |
| Physical function (POMA), median (IQR) | 17.5 (13-22) | 19 (15.8-23) | 16 (11-20) | |
| Fear of falling (FES-I), median (IQR) | 32.2 (24-39) | 24 (20.8-27) | 39 (35-43.3) |
*Including paracetamol and NSAIDs.
GDS-8=Geriatric Depression Scale, VAS=Visual Analogue Scale, POMA=Performance Oriented Mobility Assessment, FES-I=Falls Efficacy Scale-International, SD=Standard Deviation, IQR = InterquartileRange.
GDS-8=Geriatric Depression Scale, VAS=Visual Analogue Scale, POMA=Performance Oriented Mobility Assessment, FES-I=Falls Efficacy Scale-International, SD=Standard Deviation, IQR = InterquartileRange.
Relations between physical activity, physical function and FOF
Spearman coefficients for the relations between physical activity, physical function and FOF were calculated (Figure 2A, 2B). In the i) Total patient group, physical activity, physical function and FOF were all related (r=-0.34, p=0.001; r=-0.43, p<0.001; r=0.71, p<0.001). In the i) Total patient group and in the groups with ii) Low FOF and iii) High FoF, physical activity and physical function were the most strongly related (r=0.71, p<0.001; r=0.59, p<0.001; r=0.73, p<0.001). Figure 2B shows that in the (ii) low FOF group, FOF was not related to physical activity or to physical function (r=-0.07, p=0.66; r=-0.06, p=0.72). In the i) total patient group and in the iii) high FOF group, FOF was negatively correlated with physical activity and physical function(r=-0.34, p=0.001; r=-0.43, p<0.001; r=-0.44, p<0.01; r=-0.62, p<0.001). Figure 2A shows that in the iii) high FoF group, physical activity was most strongly correlated with physical function (r=0.73, p<0.001).
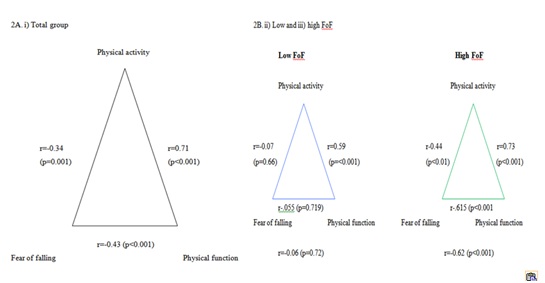
Figure 2: Correlations between physical activity, physical function and Fear of Falling (FOF).
Predictive factors of physical activity
Table 2 shows the results of the univariate logistic regression using low steps (<260) vs. high steps (>=260 steps) as dependant outcome variable. Five variables (age, gender, site of fall, physical function and FOF) were significantly associated with physical activity.
Table 2: Univariate logistic regression for physical activity.
Table 3 shows that the final predictive multivariate model consisted of four variables. Of these, female gender and better physical function were identified as statistically significant factors for physical activity (OR 5.77, 95% CI=1.28-26.02; 1.24, 95% CI=1.09-1.41). Women have an Odds Ratio (OR) of 5.77 for walking more than the median number of steps. When the POMA is one point higher, the OR for a patient walking more steps than the median number of steps is 1.24.
Table 3: Final predictive multivariate model for physical activity.
| OR (95% CI) | P-value | |
| Age (continuous) | 0.92 (0.86-0.97) | 0.01** |
| Gender (male vs. female) | 2.98 (1.02-8.70) | 0.05** |
| Site of fall (indoors vs. outdoors) | 2.86 (1.07-7.64) | 0.04** |
| Fall history (no fall vs. fall) | 0.30 (0.06-1.58) | 0.16 |
| Benzodiazepines (no use vs. use) | 0.53 (0.19-1.44) | 0.21 |
| Antihypertensive drugs (no use vs. use) | 2.00 (0.83-4.86) | 0.12 |
| Analgesics* (no use vs. use) | 0.61 (0.20-1.90) | 0.4 |
| Number of complications in elderly care facility (continuous) | 0.86 (0.63-1.18) | 0.36 |
| Number of comorbidities (continuous) | 0.95 (0.72-1.26) | 0.72 |
| Depressive symptoms (GDS-8) (less than 3 vs. 3 or more) | 0.30 (0.06-1.58) | 0.16 |
| Hearing (not impaired vs. impaired) | 1.12 (0.44-2.84) | 0.81 |
| Vision (not impaired vs. impaired) | 0.49 (0.19-1.30) | 0.15 |
| Pain (VAS) (continuous) | 0.95 (0.78-1.17) | 0.65 |
| Dizziness (yes vs. no) | 0.81 (0.23-2.89) | 0.75 |
| Physical function (POMA) (continuous) | 1.26 (1.12-1.41) | <0.001** |
| Fear of falling (FES-I) (continuous) | 0.94 (0.89-0.99) | 0.01** |
* Including paracetamol and NSAIDs.
**A p-value of <0.10 was considered significant
GDS-8=Geriatric Depression Scale, VAS=Visual Analogue Scale, POMA=Performance-Oriented Mobility Assessment, FES-I=Falls Efficacy Scale International, OR=Odds Ratio, 95% CI=95% Confidence Interval
**A p-value of <0.10 was considered significant
GDS-8=Geriatric Depression Scale, VAS=Visual Analogue Scale, POMA=Performance-Oriented Mobility Assessment, FES-I=Falls Efficacy Scale International, OR=Odds Ratio, 95% CI=95% Confidence Interval
Table 3 shows that the final predictive multivariate model consisted of four variables. Of these, female gender and better physical function were identified as statistically significant factors for physical activity (OR 5.77, 95% CI=1.28-26.02; 1.24, 95% CI=1.09-1.41). Women have an Odds Ratio (OR) of 5.77 for walking more than the median number of steps. When the POMA is one point higher, the OR for a patient walking more steps than the median number of steps is 1.24.
| B | OR | 95% CI | p-value | |
| Gender | 1.75 | 5.77 | 1.28-26.02 | 0.023* |
| Age | -0.07 | 0.94 | 0.87-1.01 | 0.102 |
| Physical function (POMA) | 0.21 | 1.24 | 1.09-1.41 | 0.001* |
| Depressive symptoms (GDS-8) | -1.9 | 0.15 | 0.02-1.30 | 0.085 |
*A p-value of <0.05 was considered significant
DISCUSSION
This study shows that in the total patient group the relation between physical activity and physical function is stronger than the relation between physical function and FOF. The relation between activity and function is also stronger than the relation between physical activity and FOF. Furthermore, we identified female gender and better physical functioning as predictive factors for higher physical activity levels after hip fracture.
Interestingly, Hornyak et al., found that in community-dwelling older adults, physical function and FOF were more strongly correlated than physical activity and physical function [19]. Obviously, this difference can be explained in terms of study population since the present study included older adults rehabilitating after hip fracture while Hornyak et al., only included healthy elderly. Moreover, in our study, only walking was examined, whereas Hornyak et al., evaluated free-living physical activity that included other activities as well [19]. In addition, the difference might also be explained in terms of the way physical function was assessed: where in the present study physical function was measured, in Hornyak et al., it was self-assessed, notwithstanding the comparability between self-reported and performance-based measurements in terms of their validity, sensitivity, and responsiveness as Latham et al., have shown [19,38].
Physical activity and physical function are positively correlated, which might suggest that when physical function is enhanced, physical activity also improves. This emphasizes the prominent role of physical function in the rehabilitation process. As such, there does not seem to be a discrepancy between what elderly patients with hip fractures are capable of doing (physical function) and what they actually end up doing (physical activity). This correlation is the strongest overall: it was found in the i) Total group, and in the ii) Low and iii) High FOF group, respectively.
The results of this study show that when FOF is high it can be predicted that physical activity and physical function will be low, as the correlation coefficients are negative. In other words, when patients have many concerns about falling they are likely to have lower scores on the POMA and walk fewer steps per day. As suggested by Tinetti et al., patients with many concerns about falling need to improve their physical function and increase confidence in their abilities [9]. By means of this dual intervention, FOF might be reduced and function and activity might be improved. In addition, Scheffers et al have developed an intervention directed at reducing FOF that may also improve physical functioning after hip fracture [7]. A possible effect of this intervention is reflected in figure 2B for the ii) low FOF group. Figure 2B shows that when FOF is low the only correlation that remains is between activity and physical function, which could mean that improving physical function is very important in the aim to increase physical activity after hip fracture.
We also identified female gender as an independent predictor of activity. In contrast, male gender was identified as a predictor of adequate physical activity in community-dwelling elderly [17]. Overall, it remains questionable if walking more than 260 steps per day could be considered as being highly physically active. In patients aged over 60 years who had elective total hip arthroplasty an average of 265 steps per day was measured on the first post-operative day [39]. The mean number of steps per day increased to 2500 steps per day within the next 30 days [39]. From this, the median in this study is comparable to the findings of Toogood et al. It might be suggested that for elderly who had surgery (elective or not) a definition of high levels of physical activity needs to be adjusted to the circumstances of surgery and vulnerability.
Nevertheless, men with hip fractures are likely to have higher American Society of Anaesthesiologists (ASA) ratings of operative risk, indicating that men with a hip fracture are more ill and therefore more vulnerable than women with hip fractures [40,41]. Due to this vulnerability, in an elderly population after hip fracture, men might be less physically active than women. Furthermore, the activity of older women may in fact be underestimated in community-dwelling elderly [17]. Women tend to be more involved in household tasks than men and these tasks are sometimes accompanied by ‘shuffling steps’ rather than actual steps; pedometers are not as effective as triaxial accelerometers in measuring these shuffling steps [42]. Therefore, physical activity in elderly women might be underestimated in community studies, leading to the conclusion that older men are physically more active whereas women are in fact just as active or even more active, as observed in the present study.
We identified better physical functioning as an independent factor for physical activity in elderly with a hip fracture. A similar finding was found among community-dwelling elderly, in whom Shimada et al., evaluated physical function by examining balance using the functional reach test, and gait by walking speed; they concluded that high walking speed was associated with improved physical activity [18]. Moreover, Lim et al.,determined a higher Short Form health survey (SF-36) physical functioning score as an independent factor for physical activity [17]. Our results also show that better physical functioning is an important predictive factor for physical activity in older persons after a hip fracture.
This study has some strengths and limitations. One strength is that physical function was measured instead of being assessed by self-reported questionnaires, which reduces the possibility of bias (e.g., selective memory bias). Another strength is that, with a sample size of 100 patients, the results are less likely to be a result of chance. Also, our sample size of vulnerable elderly patients after a hip fracture is relatively large considering that these patients are often not eligible/ available for participation, generally leading to relatively small sample sizes.
A limitation of this study is that the data are cross-sectional, meaning that patients were not followed throughout the rehabilitation process. This implies that data were collected on a selected group of patients only, i.e., patients with a slower process of rehabilitation. Therefore, caution is required when generalizing these results to other groups. Another limitation is that due to the cross-sectional design, causality between activity, function and FOF cannot be determined. Furthermore, physical activity was assessed by measuring only the number of steps per day (duration and intensity of the walks were not evaluated). This means that only one element of activity was measured and that conclusions drawn from this study regarding activity need to be interpreted with caution. Moreover, because walking in a skilled nursing facility is different from walking at home, the relations found in this study should be evaluated again among elderly that have been discharged home. Although the pedometer that we used (YX200) has been validated by Schneider et al.,as one of the most suitable pedometers for research purposes, reliability increases when activity is measured over a minimum of three days [21,22,43].
Interestingly, Hornyak et al., found that in community-dwelling older adults, physical function and FOF were more strongly correlated than physical activity and physical function [19]. Obviously, this difference can be explained in terms of study population since the present study included older adults rehabilitating after hip fracture while Hornyak et al., only included healthy elderly. Moreover, in our study, only walking was examined, whereas Hornyak et al., evaluated free-living physical activity that included other activities as well [19]. In addition, the difference might also be explained in terms of the way physical function was assessed: where in the present study physical function was measured, in Hornyak et al., it was self-assessed, notwithstanding the comparability between self-reported and performance-based measurements in terms of their validity, sensitivity, and responsiveness as Latham et al., have shown [19,38].
Physical activity and physical function are positively correlated, which might suggest that when physical function is enhanced, physical activity also improves. This emphasizes the prominent role of physical function in the rehabilitation process. As such, there does not seem to be a discrepancy between what elderly patients with hip fractures are capable of doing (physical function) and what they actually end up doing (physical activity). This correlation is the strongest overall: it was found in the i) Total group, and in the ii) Low and iii) High FOF group, respectively.
The results of this study show that when FOF is high it can be predicted that physical activity and physical function will be low, as the correlation coefficients are negative. In other words, when patients have many concerns about falling they are likely to have lower scores on the POMA and walk fewer steps per day. As suggested by Tinetti et al., patients with many concerns about falling need to improve their physical function and increase confidence in their abilities [9]. By means of this dual intervention, FOF might be reduced and function and activity might be improved. In addition, Scheffers et al have developed an intervention directed at reducing FOF that may also improve physical functioning after hip fracture [7]. A possible effect of this intervention is reflected in figure 2B for the ii) low FOF group. Figure 2B shows that when FOF is low the only correlation that remains is between activity and physical function, which could mean that improving physical function is very important in the aim to increase physical activity after hip fracture.
We also identified female gender as an independent predictor of activity. In contrast, male gender was identified as a predictor of adequate physical activity in community-dwelling elderly [17]. Overall, it remains questionable if walking more than 260 steps per day could be considered as being highly physically active. In patients aged over 60 years who had elective total hip arthroplasty an average of 265 steps per day was measured on the first post-operative day [39]. The mean number of steps per day increased to 2500 steps per day within the next 30 days [39]. From this, the median in this study is comparable to the findings of Toogood et al. It might be suggested that for elderly who had surgery (elective or not) a definition of high levels of physical activity needs to be adjusted to the circumstances of surgery and vulnerability.
Nevertheless, men with hip fractures are likely to have higher American Society of Anaesthesiologists (ASA) ratings of operative risk, indicating that men with a hip fracture are more ill and therefore more vulnerable than women with hip fractures [40,41]. Due to this vulnerability, in an elderly population after hip fracture, men might be less physically active than women. Furthermore, the activity of older women may in fact be underestimated in community-dwelling elderly [17]. Women tend to be more involved in household tasks than men and these tasks are sometimes accompanied by ‘shuffling steps’ rather than actual steps; pedometers are not as effective as triaxial accelerometers in measuring these shuffling steps [42]. Therefore, physical activity in elderly women might be underestimated in community studies, leading to the conclusion that older men are physically more active whereas women are in fact just as active or even more active, as observed in the present study.
We identified better physical functioning as an independent factor for physical activity in elderly with a hip fracture. A similar finding was found among community-dwelling elderly, in whom Shimada et al., evaluated physical function by examining balance using the functional reach test, and gait by walking speed; they concluded that high walking speed was associated with improved physical activity [18]. Moreover, Lim et al.,determined a higher Short Form health survey (SF-36) physical functioning score as an independent factor for physical activity [17]. Our results also show that better physical functioning is an important predictive factor for physical activity in older persons after a hip fracture.
This study has some strengths and limitations. One strength is that physical function was measured instead of being assessed by self-reported questionnaires, which reduces the possibility of bias (e.g., selective memory bias). Another strength is that, with a sample size of 100 patients, the results are less likely to be a result of chance. Also, our sample size of vulnerable elderly patients after a hip fracture is relatively large considering that these patients are often not eligible/ available for participation, generally leading to relatively small sample sizes.
A limitation of this study is that the data are cross-sectional, meaning that patients were not followed throughout the rehabilitation process. This implies that data were collected on a selected group of patients only, i.e., patients with a slower process of rehabilitation. Therefore, caution is required when generalizing these results to other groups. Another limitation is that due to the cross-sectional design, causality between activity, function and FOF cannot be determined. Furthermore, physical activity was assessed by measuring only the number of steps per day (duration and intensity of the walks were not evaluated). This means that only one element of activity was measured and that conclusions drawn from this study regarding activity need to be interpreted with caution. Moreover, because walking in a skilled nursing facility is different from walking at home, the relations found in this study should be evaluated again among elderly that have been discharged home. Although the pedometer that we used (YX200) has been validated by Schneider et al.,as one of the most suitable pedometers for research purposes, reliability increases when activity is measured over a minimum of three days [21,22,43].
CONCLUSION
In conclusion, in these elderly individuals rehabilitating after hip fracture, physical activity and physical function are more strongly related than physical activity and FOF, indicating the prominent role of physical function in the rehabilitation process. Women and patients with better physical functioning, as measured by a higher score on the POMA, are likely to walk more. For future interventions on physical activity, physical function and FOF, it is important to take into account that patients with high FoF may benefit from interventions aimed at both reducing FOF and improving physical function, whilst patients with less FoF may benefit from enhancing physical function only.
REFERENCES
- Balen R van, Cools HJM, Steyerberg EW, Habbema JDF (2003) Hip fracture in the elderly: epidemiology and rehabilitation. A review. Dissertation. The Netherlands.
- Latham NK, Harris BA, Bean JF, Heeren T, Goodyear C, et al. (2014) Effect of a home-based exercise program on functional recovery following rehabilitation after hip fracture: a randomized clinical trial. JAMA 311: 700-708.
- Health USDO (1996) Physical activity and health: a report of the Surgeon General. DIANE Publishing, Pennsylvania, USA.
- Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, et al. (1995) Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA 273: 402-407.
- Puts MT, Lips P, Deeg DJ (2005) Static and dynamic measures of frailty predicted decline in performance-based and self-reported physical functioning. J ClinEpidemiol 58: 1188-1198.
- Szulc P, DuBoeuf F, Marchand F, Delmas PD (2004) Hormonal and lifestyle determinants of appendicular skeletal muscle mass in men: the MINOS study. Am J ClinNutr 80: 496-503.
- Scheffers-Barnhoorn MN, van Haastregt JC, Schols JM, Kempen GI, van Balen R, et al. (2017) A multi-component cognitive behavioural intervention for the treatment of fear of falling after hip fracture (FIT-HIP): protocol of a randomized controlled trial. BMC Geriatr 17.
- Hardy SE1, Gill TM (2005) Factors associated with recovery of independence among newly disabled older persons. Arch Intern Med 165: 106-112.
- Tinetti ME, Mendes de Leon CF, Doucette JT, Baker DI (1994) Fear of falling and fall-related efficacy in relationship to functioning among community-living elders. J Gerontol 49: 140-147.
- Van Balen R, Essink-Bot ML, Steyerberg E, Cools H, Habbema DF (2003) Quality of life after hip fracture: a comparison of four health status measures in 208 patients. Disabil Rehabil 25: 507-519.
- Zidén L, Frändin K, Kreuter M. (2008) Home rehabilitation after hip fracture. A randomized controlled study on balance confidence, physical function and everyday activities. ClinRehabil. England 22: 1019-1033.
- Howland J, Lachman ME, Peterson EW, Cote J, Kasten L, et al. (1998) Covariates of fear of falling and associated activity curtailment. Gerontologist 38: 549-555.
- Salkeld G, Cameron ID, Cumming RG, Easter S, Seymour J, et al. (2000) Quality of life related to fear of falling and hip fracture in older women: a time trade off study. BMJ 320: 341-346.
- Burker EJ, Wong H, Sloane PD, Mattingly D, Preisser J, et al. (1995) Predictors of fear of falling in dizzy and nondizzy elderly. Psychol Aging 10: 104-110.
- Visschedijk J, van Balen R, Hertogh C, Achterberg W (2013) Fear of falling in patients with hip fractures: prevalence and related psychological factors. J Am Med Dir Assoc 14: 218-220.
- Bruce DG, Devine A, Prince RL (2002) Recreational physical activity levels in healthy older women: the importance of fear of falling. J Am Geriatr Soc 50: 84-89.
- Lim K, Taylor L (2005) Factors associated with physical activity among older people--a population-based study. Prev Med 40: 33-40.
- Shimada H, Lord SR, Yoshida H, Kim H, Suzuki T (2007) Predictors of cessation of regular leisure-time physical activity in community-dwelling elderly people. Gerontology 53: 293-297.
- Hornyak V, Brach JS, Wert DM, Hile E, Studenski S, et al. (2013) What is the relation between fear of falling and physical activity in older adults? Arch Phys Med Rehabil 94: 2529-2534.
- Visschedijk JH, Caljouw MA, van Balen R, Hertogh CM, Achterberg WP (2014) Fear of falling after hip fracture in vulnerable older persons rehabilitating in a skilled nursing facility. J Rehabil Med 46: 258-263.
- Berlin JE, Storti KL, Brach JS (2006) Using activity monitors to measure physical activity in free-living conditions. Phys Ther 86: 1137-1145.
- Tudor-Locke C, Bassett DR (2004) How many steps/day are enough? Preliminary pedometer indices for public health. Sports Med 34: 1-8.
- Almeida GJ, Wasko MC, Jeong K, Moore CG, Piva SR (2011) Physical activity measured by the SenseWear Armband in women with rheumatoid arthritis. Phys Ther 91: 1367-1376.
- Bohannon RW (2007) Number of pedometer-assessed steps taken per day by adults: a descriptive meta-analysis. Phys Ther 87: 1642-1650.
- Brach JS, VanSwearingen JM, Newman AB, Kriska AM (2002) Identifying early decline of physical function in community-dwelling older women: performance-based and self-report measures. Phys Ther 82: 320-328.
- Robinson CA, Shumway-Cook A, Ciol MA, Kartin D (2011) Participation in community walking following stroke: subjective versus objective measures and the impact of personal factors. Phys Ther 91: 1865-1876.
- Stevens-Lapsley JE, Balter JE, Wolfe P, Eckhoff DG, Kohrt WM (2012) Early neuromuscular electrical stimulation to improve quadriceps muscle strength after total knee arthroplasty: a randomized controlled trial. Phys Ther 92: 210-226.
- Peeters GM, van Schoor NM, Pluijm SM, Deeg DJ, Lips P (2010) Is there a U-shaped association between physical activity and falling in older persons? Osteoporos Int 21: 1189-1195.
- Tinetti ME, Williams TF, Mayewski R (1986) Fall risk index for elderly patients based on number of chronic disabilities. Am J Med. 80: 429-434.
- Faber MJ, Bosscher RJ, van Wieringen PC (2006) Clinimetric properties of the performance-oriented mobility assessment. Phys Ther 86: 944-954.
- Kloos AD, Bello-Haas VD, Thome R, Cassidy J, Lewis L, et al. 2004 Interrater and Intrarater Reliability of the Tinetti Balance Test for Individuals with Amyotrophic Lateral Sclerosis. J Neurolog Phys Ther 28: 12-19.
- Canbek J, Fulk G, Nof L, Echternach J (2013) Test-retest reliability and construct validity of the tinetti performance-oriented mobility assessment in people with stroke. J Neurol Phys Ther 37: 14-19.
- Kempen GI, Zijlstra GA, van Haastregt JC (2007) The assessment of fear of falling with the Falls Efficacy Scale-International (FES-I). Development and psychometric properties in Dutch elderly. TijdschrGerontolGeriatr 38: 204-212.
- Delbaere K, Close JC, Mikolaizak AS, Sachdev PS, Brodaty H, Lord SR (2010) The Falls Efficacy Scale International (FES-I). A comprehensive longitudinal validation study. Age Ageing 39: 210-216.
- Ulus Y, Durmus D, Akyol Y, Terzi Y, Bilgici A, et al. (2012) Reliability and validity of the Turkish version of the Falls Efficacy Scale International (FES-I) in community-dwelling older persons. Arch GerontolGeriatr 54: 429-433.
- Jongenelis K, Gerritsen DL, Pot AM, Beekman ATF, Eisses AMH, et al. (2007) Construction and validation of a patient- and user-friendly nursing home version of the Geriatric Depression Scale. Int J Geriatr Psychiatry 22: 837-842.
- Kersten P, White PJ, Tennant A (2014) Is the pain visual analogue scale linear and responsive to change? An exploration using Rasch analysis. PLoS One 9.
- Latham NK, Mehta V, Nguyen AM, Jette AM, Olarsch S, et al. (2008) Performance-based or self-report measures of physical function: which should be used in clinical trials of hip fracture patients? Arch Phys Med Rehabil 89: 2146-2155.
- Toogood PA, Abdel MP, Spear JA, Cook SM, Cook DJ, et al. (2016) The monitoring of activity at home after total hip arthroplasty. Bone Joint J 98: 1450-1454.
- Endo Y, Aharonoff GB, Zuckerman JD, Egol KA, Koval KJ (2005) Gender differences in patients with hip fracture: a greater risk of morbidity and mortality in men. J Orthop Trauma 19: 29-35.
- Arinzon Z, Shabat S, Peisakh A, Gepstein R, Berner YN (2010) Gender differences influence the outcome of geriatric rehabilitation following hip fracture. Arch GerontolGeriatr 50: 86-91.
- Dijkstra B, Zijlstra W, Scherder E, Kamsma Y (2008) Detection of walking periods and number of steps in older adults and patients with Parkinson's disease: accuracy of a pedometer and an accelerometry-based method. Age Ageing 37: 436-441.
- Schneider PL, Crouter S, Bassett DR (2004) Pedometer measures of free-living physical activity: a comparison of 13 models. Med Sci Sports Exerc 36: 331-335.
Citation: Willems E, Visschedijk J, Balen RV, Achterberg W (2017) Physical Activity, Physical Function and Fear of Falling After Hip Fracture. J Orthop Res Physiother 3: 031
Copyright: © 2017 Eva Willems, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

Journal Highlights
© 2026, Copyrights Herald Scholarly Open Access. All Rights Reserved!
