
Rare Complication of Orotracheal Intubation: Obstructive Fibrinous Tracheal Pseudomembrane, About a Case and Review of the Literature
*Corresponding Author(s):
Anass BenaliService De Pneumologie, De L’hôpital Militaire D’instruction Mohamed V. BP 10045 Rabat, Morocco
Tel:+212 537714419,
Email:anass-ab@hotmail.fr
Abstract
We report a case of obstructive fibrinous tracheal pseudomembrane as being complication of endotracheal intubation in a 73 year-old woman, whose particularities are: The non-urgent clinical presentation with non-specific symptoms, the biopsy with anatomopathological study exceptionally found in the literature for the same case and the favorable evolution under medical treatment without recourse to the interventional bronchoscopy which represents the treatment the most frequent and the most effective of this affection.
Keywords
Complication; Endotracheal intubation; Fibrinous; Pseudomembrane; Trachea
ABBREVIATIONS
OFTP: Obstructive Fibrinous Tracheal Pseudomembrane
INTRODUCTION
Obstructive Fibrinous Tracheal Pseudomembrane (OFTP) is a rare condition, secondary to ischemia of the tracheal mucosa generally of iatrogenic origin in relation to traumatic endotracheal intubations, inducing abnormal growth and regeneration [1]. We report a case of (OFTP) in a 73-year-old woman, the peculiarity of our presentation lies in the non-urgent clinical picture, biopsy achievement with anatomopathological study and favorable evolution under medical treatment.
OBSERVATION
Ms. FB aged 73 admitted to the pneumology department for chronic productive cough, bringing back mucopurulent sputum associated with a stage 3 mMRC dyspnea that had been evolving for 1 month, and beginning 4 days after her hospitalization in resuscitation, with an orotracheal intubation for severe acute respiratory failure involving the life-threatening condition following severe bilateral extensive pneumonia, settling immediately after his arrival from the pilgrimage. Clinical examination showed condensation syndrome of the upper third of the left lung. C-reactive protein was elevated to 38 mg/l and white blood cells to 15,000 elements/mm3 predominantly polynuclear neutrophils at 11,000 elements/mm3. The chest scan revealed a circumferential endotracheal formation (Figure 1). Bronchial fibroscopy revealed circumferential whitish membranes attached to the right side wall of the upper third of the trachea, the rest of the tracheal duct and the bronchial shaft without abnormality (Figures 2 & 3). Anatomopathological examination of the biopsies of this formation showed a fibrinous and leukocyte product associated with a tissue of granulations, made of polymorphic inflammatory elements (Figure 4). The patient was put on systemic corticosteroid therapy (prednisolone) at the 60 mg per day dose for 10 days and a bronchoscopy check was scheduled in 1 month, which revealed a marked improvement with an almost total disappearance of the formations pseudomembrane (Figure 5), the patient reported expectorating a whitish membrane fragment one week after the end of corticosteroid treatment and there was no recurrence after 7 months of this episode.
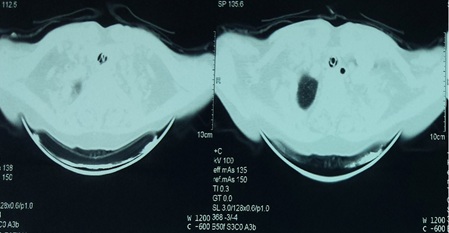 Figure 1: Chest CT showing circumferential endotracheal formation.
Figure 1: Chest CT showing circumferential endotracheal formation.
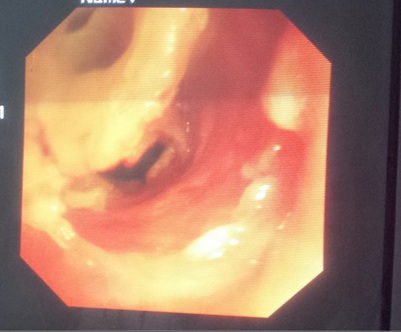 Figure 2: Bronchial fibroscopy revealed circumferential whitish membranes.
Figure 2: Bronchial fibroscopy revealed circumferential whitish membranes.
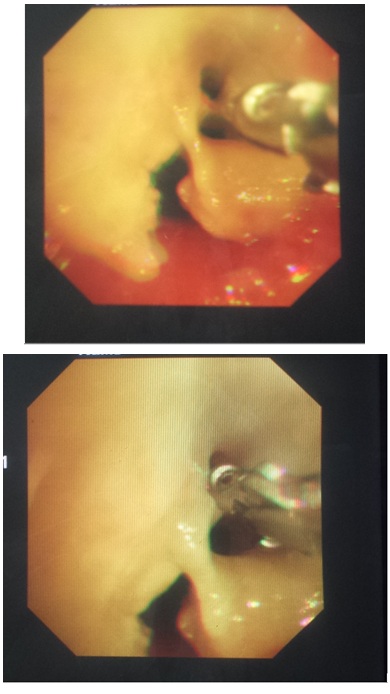 Figure 3: Biopsy of the whitish pseudomembranous formation.
Figure 3: Biopsy of the whitish pseudomembranous formation.
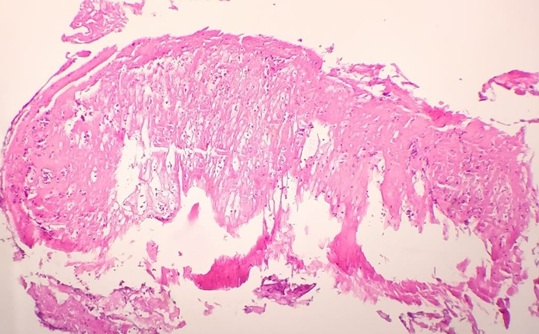 Figure 4: Anatomopathological examination of the biopsy of the pseudomembranous formation (coloring HE, magnification ×100).
Figure 4: Anatomopathological examination of the biopsy of the pseudomembranous formation (coloring HE, magnification ×100).
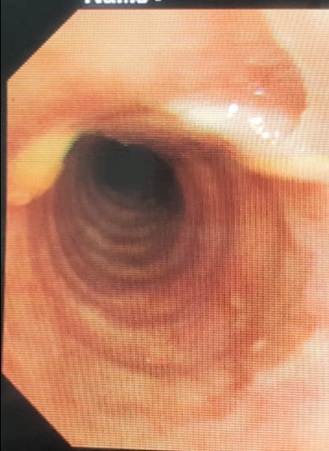 Figure 5: Bronchoscopy check showing improvement after medical treatment.
Figure 5: Bronchoscopy check showing improvement after medical treatment.
DISCUSSION
Obstructive Fibrinous Tracheal Pseudomembrane (OFTP) is a rare but serious complication of endotracheal intubation but misidentified etiopathogenesis [2]. Post-intubation trachea iatrogenic stenosis is well known and has an incidence of 4.9 cases per million per year, OFTP is a potentially rarer and less known complication of orotracheal intubation [3,4]. The diagnosis of OFTP can be a challenge because clinical presentation is often misleading in the face of the positional and intermittent nature of dyspnea and stridor, which are the most common signs [4], it must be considered among the diagnoses evoke in front of a high-pitched stridor in post-intubation [5]. In our case, OFTP is revealed by a productive dyspnea and cough in the context of a non-urgent table, in the literature review it is found that 54% of OFTPs are discovered by acute respiratory symptoms with acute respiratory distress in 17% of the first signs occur 3.1±3 days after extubation [6]. The diagnosis is confirmed by bronchoscopy which shows a fibrinous tubular sleeve obstructing tracheal light [6]. Regarding treatment, these inflammatory lesions may regress spontaneously or under systemic corticosteroid therapy (although it has no formal recommendations), however most of these cases require the application of techniques endoscopic (rigid bronchoscopy, laser resection, ct.) [7,8], mechanical extraction of these abnormalities by bronchoscopy is performed in 85% of cases, effective in all cases without recurrence after 6-11 months of follow-up [6]. In our case, the progression is favorable without recurrence after 7 months of corticosteroid treatment without the use of an interventional bronchoscopy.
CONCLUSION
OFTP is a rare complication of orotracheal intubation, often misleading clinical presentation, confirmed by bronchoscopy which also helps guide possible endoscopic treatment which represents the most but the positive development under corticosteroid therapy is also described and this is the case with our presentation.
THANKS
The doctors of pneumology department and the doctors of pathology department of the military hospital Mohamed V of Rabat who contributed to the realization of this article.
DECLARATION OF INTERESTS
The authors declare that they have no conflicts of interest in relation to this article.
REFERENCES
- Yildirim BB, Karalezli A, Hasanoglu HC, Kandemir O (2012) Obstructive fibrinous tracheal pseudomembrane. J Bronchol Interv Pulmonol 19: 129-131.
- Sehgal IS, Dhooria S, Bal A, Aggarwal AN, Behera D, et al. (2016) Obstructive fibrinous tracheal pseudomembrane after endotracheal intubation. Respir Care 61: 1260-1266.
- Nouraei SA, Ma E, Patel A, Howard DJ, Sandhu GS (2007) Estimating the population incidence of adult post-intubation laryngotracheal stenosis. Clin Otolaryngol 32: 411-412.
- Deslee G, Brichet A, Lebuffe G, Copin MC, Ramon P, et al. (2000) Obstructive fibrinous tracheal pseudomembrane. A potentially fatal complication of tracheal intubation. Am J Respir Crit Care Med 162: 1169-1171.
- Rice BL, Culver DADO, Santacruz JF, Catherine AL, McCarthy K, et al. (2011) Obstructive fibrinous tracheal pseudomembrane. Ann Thorac Surg 92: 115-117.
- Ammar Y, Vella-Boucaud J, Launois C, Vallerand H, Dury S, et al. (2016) Pseudomembrane fibrineuse obstructive de trachée: Revue systématique. Rev Mal Respir 33: 207-207.
- Wang KP, Mehta A, Turner J (2004) Flexible bronchoscopy. 2nd Blackwell, New York.
- Soong WJ, Jeng MJ, Lee YS, Tsao PC, Yang CF, et al. (2011) Pediatric obstructive fibrinous tracheal pseudomembrane-characteristics and management with flexible bronchoscopy. Int Pediatr Otorhinolaryngol 75: 1005-1009.
Citation: Benali A, Rhorfi IA, Essaoudi MA, Souhi H, Ouazzani HE, et al. (2020) Rare Complication of Orotracheal Intubation: Obstructive Fibrinous Tracheal Pseudomembrane, About a Case and Review of the Literature. J Pulm Med Respir Res 6: 038.
Copyright: © 2020 Anass Benali, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

