
Regenerative Rehabilitation for COVID 19 Sequelae
*Corresponding Author(s):
Santiago Saldarriaga-GómezCell Therapy And Translational Medicine Research Group, BioXcellerator, Colombia
Tel:+57 46041815/109,
Email:santiago.saldarriaga@bioxcellerator.com
Abstract
COVID 19 pandemic has been with us for more than a year now and new insights in pathophysiology and clinical manifestations have emerged. Recent reports have shown that not only is acute COVID a life-threatening disease, but post COVID symptoms are more common than previously thought and may greatly affect quality of life. In this review, we explore the usefulness of regenerative rehabilitation with Mesenchymal Stem Cells (MSC) in post COVID symptoms based on previous knowledge in other medical conditions. We also propose some exercise and MSC regimes that could prove useful for therapy and research based on safety and efficacy data available so far.
Introduction
Regenerative rehabilitation is a relatively new term used to describe the combination between regenerative medicine and rehabilitation therapy. It has been defined as the integration between “regenerative technologies with rehabilitation clinical practices to restitute function and quality of life in individuals with disabilities due to otherwise irreparable tissues or organs damaged by disease or trauma” [1]. Due to the growing interest in this field, the American Physical Therapy Association has defined it as the “the integration of principles and approaches from rehabilitation and regenerative medicine, with the ultimate goal of developing innovative and effective methods that promote the restoration of function through tissue regeneration and repair” [2].
While the majority of research has been conducted in musculoskeletal injuries with encouraging early results [3,4], efforts have also been made in other areas as neurorehabilitation showing promising results in conditions with otherwise poor rehabilitation prognosis, including spinal cord injuries or stroke [5,6]. MSC are one of the most studied alternatives in regenerative therapy given their easy obtention and availability and the observed effects in neurological, autoimmune and musculoskeletal conditions [7].
As this discipline is still in its early stages, mechanisms of action are yet to be totally understood. Nevertheless, based on knowledge to date in each individual therapy, two main mechanisms have been suggested to explain how regenerative medicine added to rehabilitation may exert its effect: first, MSC have the capacity to differentiate into damaged tissue cells and engraft to it, favoring healing. The second hypothesis, and the most accepted to date, lies in MSC potential to release a wide variety of anti-inflammatory and growth factors with paracrine actions that allows regeneration of affected tissue [8].
COVID 19 pandemic has spread rapid over the world, posing a collapse threat to healthcare systems. While Intensive Care Units are cornerstones in early response to the disease, regenerative rehabilitation should play an important role in COVID 19 survivors to prevent disability and to optimize acute inpatient approaches [9,10].
COVID 19 Sequelae, New Information by the Day
As time passes, new information about COVID 19 consequences have become available. It has been reported that in severe patients without intubation requirement, persistent symptoms such as dyspnea (33%), cough (33%) and fatigue (45%) are common, also finding a decrease in 6 minutes walking distance (79%) without alterations in oxygen saturation [11]. It is know that these patients may have damaged lung parenchyma with fibrosis and alveolar space obliteration [12]. Another report found that 41% of COVID patients after discharge presented at least one persistent symptom at 100 days follow up, being dyspnea the most prevalent (36%), with 21% of patients presenting a decline in diffusing capacity of the Lungs for Carbon Monoxide (DLCO) and 63% of patients still had findings in Chest Computed Tomography (CCT) scans such as ground glass opacity and reticular pattern in lower pulmonary lobes [13]. The scenario is worse in patients requiring mechanical ventilation. In CCT scans, ground glass opacity was present in 89% of patients, and findings indicating pulmonary fibrosis were present in 67% of them [14]. To date, pulmonary fibrosis prevalence has been estimated to be around 7 to 10%, similar to patients Acute Respiratory Distress Syndrome from other causes [15,16]. Looking at SARS-CoV data from 2003 it was described that 28% of patients still had similar findings in CCT a year after diagnosis and pulmonary function improvement plateaued at six months from discharge, with alterations persisting for 2 years [17], situation that has raised concerns about possible similarities with SARS-CoV-2.
Besides pulmonary sequelae, a German study including 100 patients found that 60% of patients had myocardial inflammation signs in magnetic resonance 71 days after diagnosis [18]. This finding was present even in 46% of athlete patients with no need of hospitalization [19].
As if it were not enough, mental health has also been heavily affected by this pandemic, estimating that 18% of Spaniards have depressive symptoms and 21% present with anxiety [20].
Post-COVID 19 Rehabilitation
Taking into account the previous information, different authors have urged to include early rehabilitation strategies in COVID 19 patients aiming to improve quality of life and lower sequelae impact attempting a rapid recovery [21,22]. It has been shown that cardiopulmonary rehabilitation may help patients improve 6 minute walking distance [23]. Furthermore, a study evaluating pulmonary rehabilitation in patients older than 65 years found that after 6 weeks, treated patients improved in DLCO, spirometry, quality of life and 6 minutes walking distance [24]. China and Italy are now recommending pulmonary or cardiac rehabilitation in post-acute COVID patients. Based on our medical experience in treatment and rehabilitation of post COVID 19 patients, and supported in available literature [9,10,25-27], we suggest the following cardiac and pulmonary rehabilitation exercise (Figures 1 and 2).
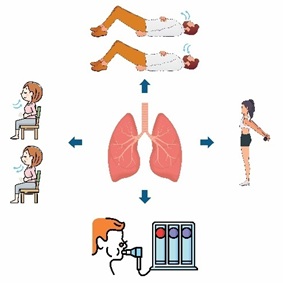 Figure 1: Pulmonary rehabilitation: Two sessions of ten minutes each per week for 4 weeks.
Figure 1: Pulmonary rehabilitation: Two sessions of ten minutes each per week for 4 weeks.
 Figure 2: Mobility and functional rehabilitation: Strength, maximal oxygen consumption (8 to 12 repetitions, 1 to 4 minutes rest, 3 sessions per week for 4 weeks).
Figure 2: Mobility and functional rehabilitation: Strength, maximal oxygen consumption (8 to 12 repetitions, 1 to 4 minutes rest, 3 sessions per week for 4 weeks).
MSC in COVID 19
Some case reports and exploratory studies have been published so far in COVID 19 and MSC. First reports from China showed how MSC use in critical patients produced improvements in clinical and paraclinical variables 4 to 7 days after therapy, lowering mortality. These authors also found that MSC do not express ACE 2 receptor, suggesting they cannot be susceptible to SARS-CoV-2 [28,29]. A study in Spain including 13 patients requiring mechanical ventilation found that intravenously infused MSC induced clinical improvements in 70% of patients and 53% of patients were able to be extubated 14 days after first dose (the majority of patients received 2 doses of 1*106 cells per kilogram of body weight with only a few receiving 3 doses) [30]. Recently, a Chinese study in patients with moderate to severe COVID 19 receiving 3 doses of 3*107 cells found that only 1 patient required mechanical ventilation compared to 4 patients in the control group [31]. No serious adverse events were found in any of these reports. In a randomized control trial involving 24 patients with severe illness, authors found better survival (91% vs 42%), cytokine profile improvement by day 6 and a faster recovery time [32]. This findings added to their regenerative capacities, could prevent long term tissue damage induced by this condition, as they are capable of lowering neutrophil infiltration and release growth factors, mRNA and microRNA that may promote lung tissue repair [33,34]. MSC are also capable of stimulating resident lung MSC into lung epithelial and support cells and also stimulate angiogenesis via vascular endothelial growth factor, basic fibroblastic growth factor and CXCL12, enhancing vascular regeneration [35]. Besides, it has been shown to be safe in pulmonary fibrosis and COPD, modulating immune response in these patients [36-39]. Based on this information, doses of 1*106 cells per kilogram should be used in regenerative rehabilitation research protocols for post COVID symptoms. To the date of writing of this article, clinical trials were yet to be registered in clinicaltrials.gov.
Conclusion
We must consider the threat and challenge that COVID 19 pandemic poses as an opportunity to rearrange and improve rehabilitation services and, at the same time, promote clinical research. We should also be encouraged to implement new therapeutic strategies such as regenerative medicine, MSC therapy and regenerative rehabilitation aiming to improve patient’s quality of life and to alleviate pressure on healthcare systems.
Funding
This work was funded by Fundación Don Roberto Fernández Viña and BioXcellerator Medellin.
References
- Perez-Terzic C, Childers MK (2014) Regenerative Rehabilitation. Am J Phys Med Rehabil 93: S73-S78.
- Head PL (2016) Rehabilitation Considerations in Regenerative Medicine. Phys Med Rehabil Clin N Am 27: 1043-1054.
- Greising SM, Dearth CL, Corona BT (2016) Regenerative and Rehabilitative Medicine: A Necessary Synergy for Functional Recovery from Volumetric Muscle Loss Injury. Cells Tissues Organs 202: 237-249.
- Ambrosio F, Wolf SL, Delitto A, Fitzgerald GK, Badylak SF, et al. (2010) The Emerging Relationship Between Regenerative Medicine and Physical Therapeutics. Phys Ther 90: 1807-1814.
- Moritz CT, Ambrosio F (2017) Regenerative Rehabilitation: Regenerative Rehabilitation: Combining Stem Cell Therapies and Activity-Dependent Stimulation. Pediatr Phys Ther 29: S10-S15.
- Kamelska-Sadowska AM, Wojtkiewicz J, Kowalski IM (2019) Review of the Current Knowledge on the Role of Stem Cell Transplantation in Neurorehabilitation. Biomed Res Int 2019: 1-9.
- Han Y, Li X, Zhang Y, Han Y, Chang F, et al. (2019) Mesenchymal Stem Cells for Regenerative Medicine. Cells 8: 886.
- Portis SM, Sanberg PR (2017) Article Commentary: Regenerative Rehabilitation: An Innovative and Multifactorial Approach to Recovery from Stroke and Brain Injury. Cell Med 9: 67-71.
- Demeco A, Marotta N, Barletta M, Pino I, Marinaro C, et al. (2020) Rehabilitation of patients post-COVID-19 infection: a literature review. J Int Med Res 48: 030006052094838.
- Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ 370: m3026.
- Daher A, Balfanz P, Cornelissen C, Müller A, Bergs I, et al. (2020) Follow up of patients with severe coronavirus disease 2019 (COVID-19): Pulmonary and extrapulmonary disease sequelae. Respir Med 174: 106197.
- Shaw B, Daskareh M, Gholamrezanezhad A (2020) The lingering manifestations of COVID-19 during and after convalescence: update on long-term pulmonary consequences of coronavirus disease 2019 (COVID-19). Radiol Med 126: 40-46.
- Sonnweber T, Sahanic S, Pizzini A, Luger A, Schwabl C, et al. (2020) Cardiopulmonary recovery after COVID-19 - an observational prospective multi-center trial. Eur Respir J 2020: 2003481.
- van Gassel RJJ, Bels JLM, Raafs A, van Bussel BCT, van de Poll MCG, et al. (2021) High Prevalence of Pulmonary Sequelae at 3 Months After Hospital Discharge in Mechanically Ventilated Survivors of COVID-19. Am J Respir Crit Care Med 203: 371-374.
- Sun P, Qie S, Liu Z, Ren J, Li K, et al. (2020) Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: A single arm meta - analysis. J Med Virol 92: 612-617.
- Thille AW, Esteban A, Fernández-Segoviano P, Rodriguez J-M, Aramburu J-A, et al. (2013) Chronology of histological lesions in acute respiratory distress syndrome with diffuse alveolar damage: a prospective cohort study of clinical autopsies. Lancet Respir Med 1: 395-401.
- Wang TJ, Chau B, Lui M, Lam G-T, Lin N, et al. (2020) Physical Medicine and Rehabilitation and Pulmonary Rehabilitation for COVID-19. Am J Phys Med Rehabil 99: 769-774.
- Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, et al. (2010) Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol 5: 1265-
- Rajpal S, Tong MS, Borchers J, Zareba KM, Obarski TP, et al. (2020) Cardiovascular Magnetic Resonance Findings in Competitive Athletes Recovering From COVID-19 Infection. JAMA Cardiol 6: 116-118.
- González-Sanguino C, Ausín B, Castellanos MÁ, Saiz J, López-Gómez A, et al. (2020) Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun 87: 172-176.
- Polastri M, Nava S, Clini E, Vitacca M, Gosselink R (2020) COVID-19 and pulmonary rehabilitation: preparing for phase three. Eur Respir J 55: 2001822.
- Gutenbrunner C, Stokes E, Dreinhöfer K, Monsbakken J, Clarke S, et al. (2021) Why Rehabilitation must have priority during and after the COVID-19-pandemic: A position statement of the Global Rehabilitation Alliance. J Rehabil Med 52: jrm00081.
- Hermann M, Pekacka-Egli A-M, Witassek F, Baumgaertner R, Schoendorf S, et al. (2020) Feasibility and Efficacy of Cardiopulmonary Rehabilitation After COVID-19. Am J Phys Med Rehabil 99: 865-869.
- Liu K, Zhang W, Yang Y, Zhang J, Li Y, et al. (2020) Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement Ther Clin Pract 39: 101166.
- Barker-Davies RM, O’Sullivan O, Senaratne KPP, Baker P, Cranley M, et al. (2020) The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med 54: 949-959.
- Sheehy LM (2020) Considerations for Postacute Rehabilitation for Survivors of COVID-19. JMIR Public Heal Surveill 6: e19462.
- De La Cerna R, Vélez de Villa A, Luzquiños D, Montesinos M, Valdivia L, et al. (2020) Protocolos Y Recomendaciones De Medicina Física Y Rehabilitación Para Pacientes con COVID-19. Figshare 2020: 1-72.
- Shu L, Niu C, Li R, Huang T, Wang Y, et al. (2020) Treatment of severe COVID-19 with human umbilical cord mesenchymal stem cells. Stem Cell Res Ther 11: 361.
- Leng Z, Zhu R, Hou W, Feng Y, Yang Y, et al. (2020) Transplantation of ACE2- Mesenchymal Stem Cells Improves the Outcome of Patients with COVID-19 Pneumonia. Aging Dis 11: 216-228.
- Sánchez-Guijo F, García-Arranz M, López-Parra M, Monedero P, Mata-Martínez C, et al. (2020) Adipose-derived mesenchymal stromal cells for the treatment of patients with severe SARS-CoV-2 pneumonia requiring mechanical ventilation. A proof of concept study. EClinicalMedicine 25: 100454.
- Meng F, Xu R, Wang S, Xu Z, Zhang C, et al. (2020) Human umbilical cord-derived mesenchymal stem cell therapy in patients with COVID-19: a phase 1 clinical trial. Signal Transduct Target Ther 5: 172.
- Lanzoni G, Linetsky E, Correa D, Cayetano SM, Alvarez RA, et al. (2021) Umbilical cord mesenchymal stem cells for COVID-19 acute respiratory distress syndrome: A double-blind, phase 1/2a, randomized controlled trial. Stem Cells Transl Med 5: sctm.20-0472.
- Copcu HE (2020) Potential Using of Fat-derived Stromal Cells in the Treatment of Active Disease, and also, in Both Pre- and Post-Periods in COVID-19. Aging Dis 11: 730-736.
- Mohammadipoor A, Antebi B, Batchinsky AI, Cancio LC (2018) Therapeutic potential of products derived from mesenchymal stem/stromal cells in pulmonary disease. Respir Res 19: 218.
- Bari E, Ferrarotti I, Torre ML, Corsico AG, Perteghella S (2019) Mesenchymal stem/stromal cell secretome for lung regeneration: The long way through “pharmaceuticalization” for the best formulation. J Control Release 309: 11-24.
- Weiss DJ, Casaburi R, Flannery R, LeRoux-Williams M, Tashkin DP (2013) A Placebo-Controlled, Randomized Trial of Mesenchymal Stem Cells in COPD. Chest 143: 1590-1598.
- Armitage J, Tan DBA, Troedson R, Young P, Lam K, et al. (2018) Mesenchymal stromal cell infusion modulates systemic immunological responses in stable COPD patients: a phase I pilot study. Eur Respir J 51: 1702369.
- Stolk J, Broekman W, Mauad T, Zwaginga JJ, Roelofs H, et al. (2016) A phase I study for intravenous autologous mesenchymal stromal cell administration to patients with severe emphysema. QJM 109: 331-316.
- Chambers DC, Enever D, Ilic N, Sparks L, Whitelaw K, et al. (2014) A phase 1b study of placenta-derived mesenchymal stromal cells in patients with idiopathic pulmonary fibrosis. Respirology 19: 1013-1018.
Citation: Viña MF, Halpert K, Quintero-Gil C, Saldarriaga-Gómez S (2021) Regenerative Rehabilitation for COVID 19 Sequelae. J Stem Cell Res Dev Ther 7: 065.
Copyright: © 2021 Matias Fernandez Viña, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

