
Resolution of a Clinical Case of Severe Bone Deficit in a Patient with Marked Osteoporosis with the use of Growth Factors
*Corresponding Author(s):
Maurizio SerafiniPrivate Practitioner, Via Caduti Sul Lavoro, 37 - 66100 Chieti, Italy
Email:serafinidrmaurizio@gmail.com
Abstract
Many patients lack both vertical and horizontal bone dimensions required for endosseous implant insertion. Removable prostheses are also unsuccessful in situation with severe bone resorption. Bone regeneration is the crucial key for a correct implant positioning and allows patients to have fixed prosthesis which is a much more accepted rehabilitation. This clinical case report describes and demonstrates how advanced modern implantology can successfully handle severe vertical and horizontal bone defects.
Keywords
Bone graft; Dental implants; Growth factors; Oral rehabilitation; Platelet rich plasma; Severe Bone defects; Severe osteoporosis; Vertical and horizontal bone defects
Introduction
Modern implantology replaced vertical and horizontal severe bone defects regeneration with easier procedures such as all on four, few implant full arch or sinus lift with zygomatic implants.
Compared to bone regeneration, these procedures are on one side less expensive and the prosthesis can be realized in shorter time, but on the other side it is harder to keep clean and maintain an adequate oral hygiene which lead often to peri-implant inflammation and failure of one or more implants. The result for the patient is frequent dental checks and professional cleanings and if implant failure occurs, it needs to be replaced and a new prosthesis has to be made.
Severe resorbed ridges regeneration requires expert surgeon skills in manipulating growth factors in combination with autogenous block grafts.
Intraoral donor sites are:
- • Mandibular ramus
- • Symphysis
- • Edentulous ridges
- • Tuber to
Extraoral donor sites like:
- • Tibia
- • Iliac crest
- • Calvaria, etc.
Intraoral donor sites have several benefits, such as, less bone resorption after healing when compared to extraoral donor sites and graft harvesting can be performed under local anesthesia. Their limitations are donor site morbidity and limited availability [1]. Although horizontal bone augmentation is reasonably predictable, vertical bone augmentation usingblock grafts remains unpredictable [2]. This is because in severe atrophies with reduced vertical dimension, there is usually a lack of primary wound closure due to insufficient soft tissue which is often transplanted from the palatal mucosa.
Healing process is conditioned by age, medical status, systemic disease, osteoporosis, patient compliance and many others factors [3]. Considered what has been said, adding a more invasive surgery in both donor and recipient site, longer healing time, more expensive costs, longer and more difficult work with more responsibilities for the surgeon, adds up with choosing modern implantology.
Henceforth, the purpose of this case report is to describe bone regeneration of an atrophic residual ridge with restitutio ad integrum and achievement of a successful functional and esthetic implant supported restoration.
Clinical Case
A 50-years old female patient presented at our observationwilling to replace her 30-years old full arch gold-ceramic prosthesis which is no longer congruous (Figures 1-3).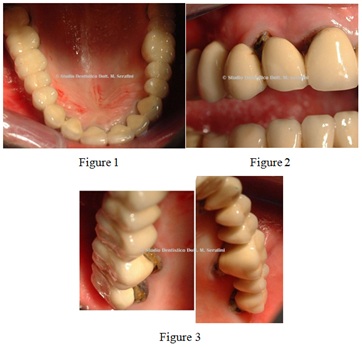
Figures 1-3: Initial presentation.
Orthopantomography, computed tomography scan and bone mineralography reveal severe bone deficit (Figure 4).
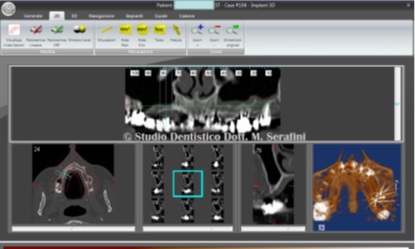 Figure 4: Computer tomography scan.
Figure 4: Computer tomography scan.
On the right side the bone presents as a triangular knife edged shaped with hyperpneumatization of maxillary sinus, for this reason the treatment plan is split crest and crestal sinus lift with insertion of one 3.50 per 16 mm one piece implant in position 1.2 and two 4.20 x 13 mm in position 1.4 and 1.5.
On the left side the bone presents as a bowl edged shaped and the treatment plan includes also a split crest and the insertion of dental implant 4.20 per 16 in position 2.5 one piece and a 5 per 13 mm in position 2.7. Tooth n. 2.6 will be extracted in a second stage surgery in order to preserve adjacent bone (Figures 5 & 6).
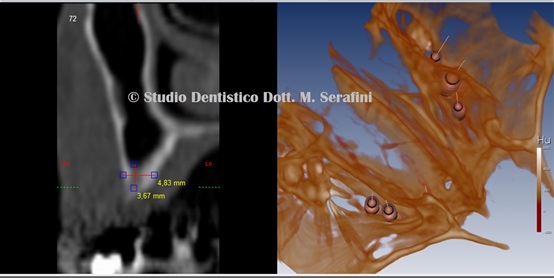 Figure 5: Particular and 3D reconstruction.
Figure 5: Particular and 3D reconstruction.
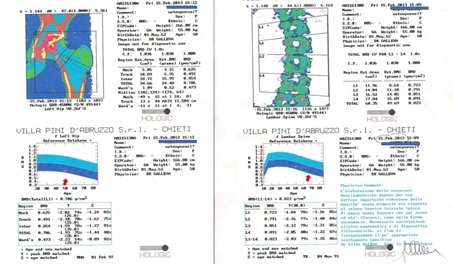 Figure 6: Bone mineralography.
Figure 6: Bone mineralography.
Prior to surgery patient was prescribed antibiotic therapy (Amoxicillin and Clavulanic acid 1 g, two times a day for 1 week). After removal of the old full-arch prosthesis (Figure 7), impressions are taken and a provisional prosthesis is manufactured.
 Figure7: Full arch prosthesis removed
Figure7: Full arch prosthesis removed
8 venous blood tubes samples of 3.5 ml each are taken and centrifuged with sodium citrate as anticoagulant for 20 minutes at 1000 rpm obtaining PRP (Figure 8).
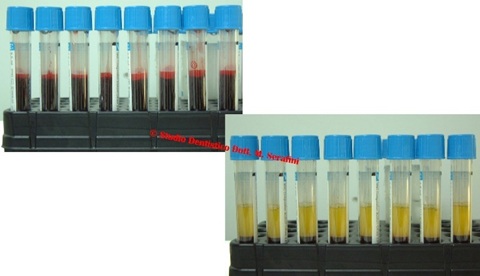 Figure 8: Venous blood samples and PRP.
Figure 8: Venous blood samples and PRP.
Under local anesthesia, a full thickness flap both palatal and vestibular is reflected on the right side exposing a triangular knife edged shaped bone very thin as expected from the CT scan (Figure 9).
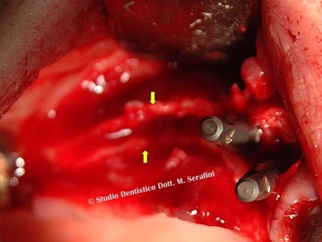 Figure 9: Full thickness flap on the right side.
Figure 9: Full thickness flap on the right side.
A split-crest is performed malleating chisels and surgical hammer without the use of piezo surgery or bursin order to prevent further bone loss [4] (Figure 10).
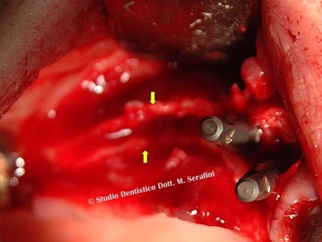 Figure 10: Bone separation.
Figure 10: Bone separation.
After the split crest, a crestal sinus lift is performed by placing PRP imbibed fibrin sponges.
Three implants are placed in position 1.2, 1.4 and 1.5 and a mix of PRP, calcium chloride and animal bone is inserted as scaffold both palatal and vestibular (Figure 11).
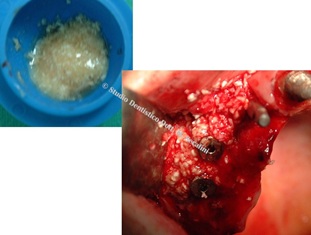
Figure 11: Bone graft.
On the left side after reflecting a mucoperiosteal flap, a bowl shaped bone defect is exposed (Figure 12).
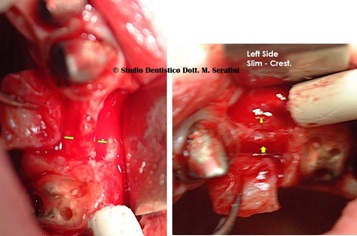 Figure 12: Bowl shaped bone defect on left side.
Figure 12: Bowl shaped bone defect on left side.
On the left side a split crest is also performed with chisels and surgical hammer and two implants are placed in position 2.5 and 2.7 with bone graft (Figures 13-17).
 Figure 13: Split crest, bone graft and 2 implants on the left side.
Figure 13: Split crest, bone graft and 2 implants on the left side.
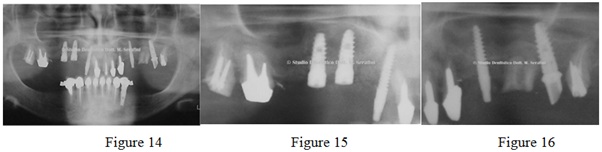 Figures 14-16: Post Surgery X-ray.
Figures 14-16: Post Surgery X-ray.
 Figure 17: Sutures.
Figure 17: Sutures.
Temporary prosthesis is placed on 3 immediate loaded implants while on the right side implants are buried and not loaded because of the crestal sinus lift (Figure 18). 
Figure 18: Provisional prosthesis inside.
After 14 months tooth 2.6 is extracted and an immediate loaded implant 6 per 10 mm is inserted. Wax up is made after bone healing is achieved (Figures 19-21). 
Figures 19,20: Wax up.
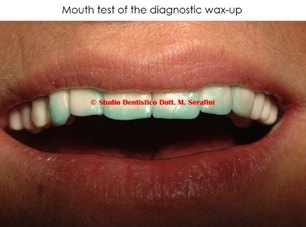 Figure 21: Wax up tested intraorally.
Figure 21: Wax up tested intraorally.
Once occlusal, phonetical and esthetical tests are satisfying, final zirconia-ceramic prosthesis is made (Figures 22-24).
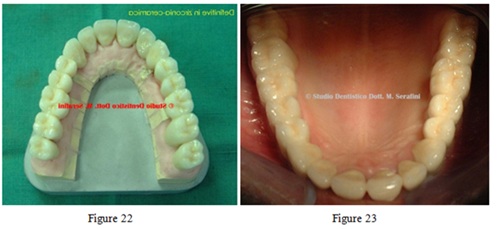
Figures 22,23: Zirconia-ceramic final prosthesis.
 Figure 24: Definitive in zirconia-ceramica (her smile).
Figure 24: Definitive in zirconia-ceramica (her smile).
Figure 25 shows the seven years x-ray control.
 Figure 25: Seven years x-ray control.
Figure 25: Seven years x-ray control.
Discussion
In dentistry, bone regeneration is essential in order to achieve a successful occlusal rehabilitation, hence the possibility of inserting stable and osseointegrated dental implants.
In case of major bone deficits, like the one reported in the present case report, research has focused on the use of autologous growth factors as the best way to induce tissue regeneration. Growth factors are often used in association with the scaffold, with the aim of improving hard and soft tissue healing.
Platelet-Derived Growth Factor (PDGF), Transforming growth factor-β 1 (TGF-β 1) and β 2 (TGF-β 2), Fibroblast Growth Factor (FGF), Vascular Endothelial Growth Factor (VEGF), Insulin-Like Growth Factor (IGF) are some of the growth factors involved which stimulate cell proliferation, enhance angiogenesis and make regeneration more significant and predictable [5].
Conclusion
As reported in the present clinical case report, growth factors improved on one sidesurgical outcomes and on the other side patient’s postoperative phases. Certainly, further studies are needed to analyze in more detail the differences between the different growth factors and their role in the regeneration process but, as shown in the 7-years x-ray control, the use of growth factors it is a valid and a long-term successful aid in the dental field.
References
- Schwartz-Arad D, Levin L (2005) Intraoral autogenous block onlay bone grafting for extensive reconstruction of atrophic maxillary alveolar ridges. J periodontol 76: 636-641.
- Felice P, Pistilli R, Lizio G, Pellegrino G, Nisii A, et al. (2009) Inlay versus onlayiliac bone grafting in atrophic posterior mandible: a prospective controlled clinical trial for the comparison of two techniques. Clin Implant Dent Relat Res 11: 69-82.
- Rocchietta I, Moreno F, Nisand D (2020) Bone augmentation by anatomical region: techiques and decision making. Pg No’s: 235-254.
- Dmiler DJ, Johnson PW, et Lozada JL, Misch C, Rosenlicht JL, et al. (1992) Dental Clinics of North America 36: 151-86
- Cicciù M (2020) Growth Factor Applied to Oral and Regeneraive Surgery. Int J Mol Sci: 21: 7752.
Citation: Serafini M, Zagaria L, Teodoro SD, Romondio L (2021) Resolution of a Clinical Case of Severe Bone Deficit in a Patient with Marked Osteoporosis with the use of Growth Factors. J Stem Cell Res Dev Ther 7: 071.
Copyright: © 2021 Maurizio Serafini, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

