
Sarcoma on Ski: Individual Skiing Concepts Enable Autonomous Skiing After Multimodal Therapy for Pediatric Muscular-Skeletal Tumors
*Corresponding Author(s):
Joachim BoosDepartment Of Pediatric Hematology And Oncology, University Hospital Münster, Münster, Germany
Tel:+49 2518347865,
Email:boos@ukmuenster.de
Abstract
Long-term physical impairments are frequent consequences of multimodal therapy for malignant pediatric sarcomas. Surgical interventions like endoprosthetic support or amputations limit participation in many popular sportive activities. Demanding sports like alpine skiing are automatically avoided. Due to the potentials of skiing as an individually adaptable sport, preexisting family-oriented skiing camps for survivors of pediatric cancer since 1994 were expanded to children with sarcomas even with accompanying physical impairments or reduced movement patterns.
This work summarizes the individual solutions for 31 participants with soft-tissue sarcomas and bone tumors (age 14 ± 6.5 years, 48% male, various surgical techniques) to detect underlying challenges, benefits and limits of skiing and to improve the decision making process with regard to the optimal skiing technique.
All children and adolescents learned skiing in accordance to their individual abilities and limitations. Skiing techniques varied from conventional upright skiing, to one-leg skiing or sit ski. Four case examples are presented in detail.
Findings suggest that skiing after pediatric sarcoma is feasible. The wide range of possible adaptions and skiing techniques obviate exclusion of handicapped children in skiing holidays or school ski trips. Interdisciplinary collaborations, professional support and specific equipment and methodology are the key points of successful concepts.
Keywords
INTRODUCTION
They all represent life threatening diseases with cure rates below average. Approximately 70% of the patients are cured, but adverse consequences of multimodal therapy persist lifelong [1]. These children and adolescents had received intensive chemotherapy and high cumulative dosages of anthracyclines, vinca-alkaloides and alkylating agents. Besides the need of systemic therapy, local control of the tumor still is challenging. The local therapy of soft-tissue sarcomas as well as Ewing’s sarcomas often includes intensive radiotherapy. All patients with muscular-skeletal tumors however undergo local surgery aiming for complete removal of the tumor without any remaining cell at the tumor site [2]. Acute side effects, for example immunosuppression, neuropathy, fatigue, a substantial degree of changes and deprivation in social life during acute treatment phase are followed by an outlasting probability of persisting or developing related late effects like muscular weakness, peripheral neuropathy, osteoporosis and potential organ deficits in addition [3-7].
As a consequence most of the patients experience this as more or less relevant alteration of their body image [8] and often as significant change in function and movement pattern [9, 10]. As the majority of bone tumors involve the extremities, normal motion and participation in sports becomes a major topic on the way back to normality. Although limb-salvage surgery is a major goal and became more and more successful [11], endoprosthetic support, arthrodesis, rotationplasty and other technical solutions cannot substitute amputation in all cases and even if the function is quite good, patients feel handicapped [10].
Physical activity levels and motor performance are dramatically reduced during and shortly after treatment [12-15] and such limitations persist throughout adulthood [5,6,16-19]. There is no doubt that physical activity and sports interventions contribute to the reduction of late effects and influence clinical and psychosocial outcome positively [20-23]. However, our experience and a survey in one outpatient Clinic of Pediatric Oncology showed that the questioned children and adolescents with sarcoma are not attending school and are excluded from activities in sports clubs [24]. Reintegration into physical education at school as well as in grassroots sports and sports clubs is challenging, participation in skiing activities however seems impossible-from patients', parents' and often teachers' and trainers' point of view. Skiing as a non-competitive individual, but demanding outdoor sports activity might be an alternative solution to highly risky contact sports for some children and adolescents. However, the conditions, limitations and even contraindications of skiing are subject of intense discussion. Intuitive skepticism and overprotection frequently seem to cover the positive exploration of benefits and chances.
At our institution, annual one-week skiing camps were started in 1994. These family-orientated camps offer skiing lessons for beginners as well as experienced skiers and are open for families all over Germany. The mountain hut in Kleinwalsertal/Austria is settled at the top of a hill and is not barrier-free. At the beginning, we shared the mentioned skepticism and excluded patients after treatment for pediatric sarcomas due to concerns of inherent risk and lack of experience.
With increasing experience and after state-approved amateur ski instructor’s training for adapted skiing for amputees, blind and the visually impaired, individuals with cerebral palsy, intellectual disabilities and wheelchair athletes at the Government Sports Academy in Innsbruck [25], our program was expanded in 2008 to children and adolescents after treatment for sarcoma even with significantly reduced movement pattern and severe physical impairments. Until now, 87 courses ended successful and currently 7 courses for about 50 families and a total of 180 participants are offered every year.
To overcome the concerns of participants, parents and even physicians, specific reflection and detailed information on preexisting experience and an algorithm of individual decision making is required. Based on our experience and documentation, we aim at deducting practical implications representing scopes and limits. We therefore retrospectively analyzed our mono-center experience of the last six years in order to enable better informed decision making for participants and involved professionals.
MATERIALS AND METHODS
Data assessment
Skiing methodology
There are several skiing techniques for participants treated for pediatric sarcomas that can be adapted according to their individual requirements and physical impairments: 1) skiing upright on both legs with two skies and conventional ski poles, 2) skiing upright on both legs with two skis and two outriggers (4-ski-method) instead of ski poles, 3) skiing upright on one leg using two outriggers (3-ski-method), 4) using sit ski devices (Bi-ski, Dualski or Monoski). Outriggers used in upright skiing increases stability (4-ski-method) or enables skiing on one leg (3-ski-method). These different adaptive skiing techniques can also be used in combination and/or with additional tools ((e.g., ski tip holder, elastic retaining band). Examples for each approach of adaptive skiing techniques are shown in the results (Examples A-D).
RESULTS
Participants
| Characteristics | n (%) | Mean ± SD | Median | Range |
| Age at first participation (years) | 31 (100) | 14 ± 6.5 | 15 | 5-36 |
| Gender | ||||
| Male | 15 (48) | |||
| Female | 16 (52) | |||
| Time since diagnosis at first participation (months) | 31 (100) | 30.0 ± 17.7 | 26 | 12-91 |
| Cancer type, age (years) and location | 31 (100) | |||
| Bone tumor | 24 (77) | 15.2 ± 6.2 | 15 | 6-36 |
| Ewing’s sarcoma | 10 (32) | |||
| Osteosarcoma | 12 (39) | |||
| NOS | 2 (6) | |||
| Lower limb | 17 (55) | |||
| Trunk/upper limb | 7 (23) | |||
| Soft-tissue sarcoma | 7 (23) | 9.7 ± 5.9 | 7 | 5-20 |
| Trunk/head | 5 (16) | |||
| Lower limb | 2 (7) | |||
| Local therapy | 31 (100) | |||
| Surgery | 28 (90) | |||
| Tumor endoprosthesis | 12 (39) | |||
| Resection only | 6 (19) | |||
| Amputation | 5 (16) | |||
| Rotationplasty | 4 (13) | |||
| Hemipelvektomy | 1 (3) | |||
| Radiation | 11 (35) | |||
The participants attended the skiing camps on average 2.6 times (range 1-7 times). They all made relevant progress in skiing. The variation of participations is not representing learning curves. All ended up with different but increased skiing skills. As a standard the participation had been limited to 1-2 courses due to limited places. Families with children with a higher need of support were invited more often. This could be due to the need of technical skiing materials (outriggers, sit ski…) or to complex functional impairments. Four participants died in the meantime.
Adaptive skiing techniques
| Tumor Localisation Lower Extremity | Tumor Localisation Upper Extremity/Trunk/Head | ||||||||
| Skiing Technique | Endoprosthesis | Resection | Amputation | Endoprosthesis | Resection | (n) | |||
| Proximal Femur | Distal Femur | Proximal Tibia | Proximal Humerus | ||||||
| Conventional upright skiing | 2 | 1 | 2 | 8 | 13 | ||||
| Upright skiing with tools | 1 | 1 | 2 | ||||||
| One-leg skiing with outriggers | 8 | 8 | |||||||
| Bi-ski/Dual ski accompanied | 3 | 1 | 4 | ||||||
| Bi-ski/Dual ski/Mono ski accompanied on their own | 2 | 2 | |||||||
| Bi-ski/Dual ski accompaniedupright skiing | 1 | 1 | 2 | ||||||
| (n) | 10 | 1 | 9 | 2 | 9 | 31 | |||
We do not advise skiing upright on both legs with an artificial limb after rotationplasty. The changes in joint and bone structure make it difficult to evaluate and control the biomechanical function of the lower limb during skiing. We have been informed of a fracture occurring following upright skiing of a participant with a rotationplasty. For these reasons we recommend one-leg skiing for participants with amputation including rotationplasty.
To clarify individual approaches of applied techniques regarding different impairments four representative cases of adaptive skiing techniques are presented in the following section in categories: (A) One-leg skiing, (B) Mono-ski highly sportive, (C) Sit ski to upright skiing and (D) Skiing with special tools.
(A) A seven year old girl, diagnosed with Ewing’s sarcoma at the left distal femur was treated with EURO-EWING 99 and underwent rotationplasty Type B III a according to Winkelmann with maintenance of the vascular system at the age of three years (Figure 1). Post-operative chemotherapy was applied following surgery according to treatment regime. Prosthetic care enables walking on two legs in everyday life. To prevent injuries of the residual limb and due to preservation of the exoprosthesis, one-leg skiing was taught. Problems often occur due to uncommon load on one leg. Participants are used to walk on both legs in everyday life and skiing on one leg requires increased muscular strength.

Figure 1: Post-operative radiograph of rotationplasty and one-leg skiing technique.
After five years of participation, intensive training with an adaptive skiing instructor and security tools (elastic retaining band), autonomous one-leg skiing is possible with only slightly further assistance (Figure 1). The girl gained a lot of self-confidence in skiing which made her choose a secondary school selectively that conducts a school ski trip.
(B) A 13 year old boy, diagnosed with an osteosarcoma at the left distal femur underwent neoadjuvant chemotherapy according to EURAMOS-1/COSS prior to surgery. Surgical procedure included tumor resection and implantation of endosprosthetic replacement (Figure 2). Following surgery post-operative chemotherapy was applied and further surgical intervention was necessary due to metastatic suspected pulmonary nodules in the lungs, infection of the endoprosthetic replacement and following revision and implantation of a new endoprosthesis.
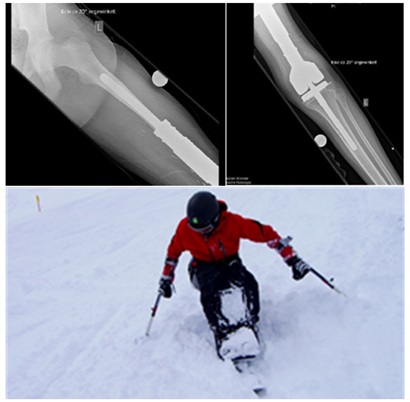
Figure 2: Post-operative radiograph of endoprosthetic replacement of the distal femur distinct shielding at the prosthesis stem and picture of sit ski technique. (Enneking score was 27 in the first camp).
After five years of continuous support and intensive training with experts in sit ski technique, the boy is now skiing completely autonomously and on a very sportive level owing his own Mono-ski. He decided to continue skiing in a sitting position even though upright skiing would be possible regarding muscular status and stability of the femur and prosthesis.
(C) A 15 years old girl was diagnosed with an osteosarcoma in the right proximal tibia. After undergoing standard neoadjuvant chemotherapy according to EURAMOS-1/COSS, broad partial extra-articular tumor resection and an endoprosthetic replacement of the proximal tibia including transposition of M. gastrocnemius and reconstruction with mesh-graft plastic were performed ((Figure 3). Following surgery post-operative chemotherapy was applied in accordance with treatment regime.

Figure 3: Post-operative radiograph of endoprosthetic replacement of proximal tibia and picture of the girl in the second year of skiing (Enneking score 26 at the first camp).
One year after finishing anticancer therapy the girl participated in the skiing camp for the first time. In the first year, she started in the sitting position to slowly get used to skiing and to minimize the risk of injury due to missing muscles and the ongoing rehabilitation process shortly after cessation of treatment. The girl was accompanied and guided by an adaptive ski instructor and always secured with an elastic retaining band. Due to personal reasons she could not finish the week after two days in the skiing camp. In her second year, she started skiing in an upright position with conventional skiing poles accompanied by an adaptive ski instructor. To maximize safety aspects like length of the ski, fixation and torque as well as active observation of fixation release were considered to prevent injuries as far as possible. Additionally, a physiotherapist from the Department of Pediatric Oncology was part of the ski team. This physiotherapist oversaw the home-based physiotherapy scheme and was able to continue additional physiotherapy during the skiing camp. Ski biomechanics were also analyzed in collaboration with the ski teacher and the physician.
(D) A 17 years old girl diagnosed with a bone sarcoma (NOS) originating from the os sacrum with paravertebral expansion and infiltration of the lamina L5/S1 was treated according to EURO-EWING 2008. After surgery including internal hemipelvectomy and hemisacrectomy, spinal decompression and bone defect reconstruction (Figure 4), post-operative chemotherapy following CWS-Protocol and radiation was applied. This severe surgical treatment caused a peronaeus paresis as well as the loss of sensitivity and control in the lower limb and half of the upper limb in the left leg. These complex physical impairments required testing of different techniques of adaptive skiing (Figure 4).

Figure 4: Post-operative radiograph of the surgical intervention around the os sacrum and presentation of testing different techniques with tools (Enneking score 17 at the first camp).
After the first approaches in a sitting position and security measures with ropes, the final solution required a ski-tip holder to control the positioning of the skis and outriggers to ensure stability. After two years of training skiing technique and balance, this girl is now skiing with conventional ski poles optimized by a wedge of about one centimeter beneath the affected foot. This heel rise helps to reduce the tendency to load through the dorsal part of the foot.
Deduction of a concept on decision making strategies
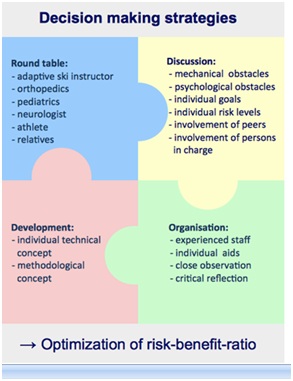
Figure 5: Concept of decision making strategies for integration in winter sports activities after treatment for pediatric sarcomas.
DISCUSSION
There are no general solutions available to gain autonomy in skiing after severe surgery, coping with physical impairments and therapy-related late effects. The approaches are individual and sometimes complex. But nevertheless, there are ways and support should be offered as long as necessary. By developing an individual skiing didactic and applying specific adaptive skiing support to maximize safety, skiing is feasible even after severe surgery and despite functional limitations (Figure 5). Decision making strategies including round table meetings with all persons involved, discussions on goals, risks and barriers, the development of individual approaches and concepts and a well prepared organization are indispensable to optimize the risk-benefit-ratio. All parts shown should be addressed carefully to maximize safety, minimize risks and increase the participants’ individual benefit in learning how to ski: “Face the risk and face the chances”.
Tables 2 and 3 show that there are different individual approaches of skiing after treatment for pediatric sarcoma and every single participant has his or her own aim and wish that needs to be considered and respected. All participants began with close supervision and individual training, but integration into groups is always the aspired aim that should be realized as soon as possible. Moreover, it should also be considered that some of the children and adolescents treated for pediatric sarcomas do not suffer from severe orthopedic impairments, but all of them underwent intensive treatment and everyone has his or her individual tumor- and therapy-related side effects like e.g., neuropathy, pressure pain, impaired balance that lead to specific consequences in equipment and assistance. Functional impairments clearly differ related to location of the tumor. Most of our participants included in this analysis were treated for tumors at the lower limb. As shown in the case reports these children and adolescents must face limitations like e.g., reduced muscle strength, instability or neurological impairments as the loss of sensitivity. Participants treated for tumors at the upper limb might have difficulties holding the skiing pole or balancing. Furthermore, regarding anxiety of falling on the prosthesis balance and coordination should be trained in advance. Soft-tissue sarcoma at the trunk (e.g., Rhabdomyosarcoma) does not result in severe functional impairments at first glance, but common disease- and therapy-related limitations like reduced physical fitness also require close support. Due to all those different impairments and limitations individual approaches needed to be developed for every participant.
| Case | (Orthopedic) Impairment | Participant’s Wish/Ambition | Adaptive Skiing Technique | Outcome/Reality |
| (A)Female7-12 yrs | Rotationplasty(Type B IIa) | Upright skiing, Autonomy | One-leg skiing with intensive support and annual training during 5 years | (Autonomous) skiingwith only little support needed, Plan of participation in school ski trip |
| (B)Male14-20 yrs | Tumor resection,Enprosthetic device, Distal femur | Sporty skiing, autonomy,Skiing with peers, Participation in school skiTrip | Training in sit-ski (Bi-ski, Dual-ski,Mono-ski) during skiing camp (6 times), Companionship on school ski trip, Additional training in ski hall and supply of devices for own training | Autonomous and sporty skiingwith own Mono-ski (skiing inupright position not favoured),Integration in peer group |
| (C)Female15-19 yrs | Tumor resection,Enprosthetic device, Proximal tibia | Upright skiing, Skiing with peers and family | Accompanied sit-ski (Bi-ski) training during 1st and partly 2ndparticipation, Upright skiing with intensive support during 2ndparticipation and further training during 3rd and 4thparticipation, Physiotherapeutic support | Autonomous and safe skiing in upright position, skiing with peers and familiy possible |
| (D)Female16-19 yrs | Internal hemipelvectomy and hemisacrectomy, Dorsaldecompression L4-S2, Bone defect reconstruction | Upright skiing, autonomy,Nosit-ski device, Participation in school skitrip | Accompanied sit-ski (Bi-ski) training during 1st participation (partly), change to upright skiingwith tools and intensive support,Companionship on school ski trip,Intensive training during 2nd and 3rdParticipation, physiotherapeutic support | Autonomous and safe skiing in upright position with ski tipholder, Integration intopeer group |
These approaches include detailed risk-benefit information to children and families. They include the cautious adopting of the ski-length and bindings and their z-scores to the estimated individual condition and avoid breakage of bone or prosthesis or other injuries. They include awareness to avoid losing ski and prosthesis in chair lifts and a couple of comparable individually foreseeable risks. In addition, they include a prospective plan of checkups and controls for example for pressure sores and frostbites if kids may have neurological deficits at their extremities potentially related to tumors, surgeries or chemotherapy.
Up to now, we did not see any no-go situation in skiing related to physical impairments. Only for one patient after treatment for a Ewing’s Sarcoma who wanted to participate, skiing was not recommended due to an instable spine.
Skiing is a non-competitive outdoor sport, has the potential to improve autonomy and might be a motivating sports activity especially for severely impaired adolescents who cannot engage in common high impact and team sports. The children and adolescents in our camps are highly accepted in peer groups and they are not retarding others while skiing together. They experience positive general recognition and acceptance rather than cautious thoughtfulness.
Little is known about skiing after limb-salvage surgery. Hobusch et al. [27] retrospectively questioned long-term survivor after treatment of bone tumors and limb-salvage surgery (n=27 malignant bone sarcomas) regarding continuation and activity levels of sports activities. Of N=4 analyzed patients who engaged in alpine skiing prior to diagnosis, N=2 continued more than five years later. There’s no information on skiing technique and level of intensity given.
All of the analyzed children and adolescents were able to learn autonomous skiing, some of them were even fully integrated into school ski trips. All were extremely surprised and developed significant changes in their body perception. Skiing requires several skills (e.g., strength, balance, coordination) and, the other way round, could have training effects. Nasuti and Temple [28] reviewed existing intervention studies on snow sports for people with disabilities and concluded that research is rare, but there is some evidence for positive influence of skiing on self-perception and motor performance. Furthermore, they estimate the risk to engage in snow sports not greater than in the general population.
In our skiing camps, we didn’t assess any data of motor performance or physical fitness prior to and after the week of skiing, but in most cases, we got the strong impression that skiing supported their physical recovery in general and especially according to their restrictions after surgery. The most important aspects of our skiing camps are experience of an outdoor sports activity, participation in family and peer groups, regain quality of life after a long and exhausting period of treatment, try a new kind of sports activity or retry after anticancer treatment in a protected environment and with professional support.
Specific training regarding preservation and improvement of muscle strength seems to be an important aspect for children and adolescents during and after anticancer treatment, especially after prosthetic replacement at the upper and lower limb. We recommend the concept of continuous sports interventions from diagnosis to aftercare to support pediatric cancer patients that we implemented in Münster and as well as in some more departments up to now during the last years (Figure 6).
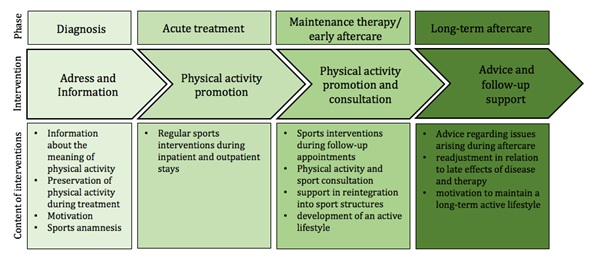
Figure 6: Continuity of intervention strategies during different phases of therapy. (Modified version of Kesting et al. 2016) [29].
CONCLUSION
By sharing our experience, we would like to encourage sarcoma patients and their families, but in particular orthopedic surgeons and other professionals working in orthopedic aftercare to dare to think about apparently hardly possible sports activities after severe surgery and discuss feasible approaches with their patients and involved experts.
CONFLICTS OF INTEREST
ACKNOWLEDGEMENTS
We acknowledge support by Open Access Publication Fund of University of Muenster.
REFERENCES
- Kaatsch P, Spix C (2014) “German Childhood Cancer Registry - Report 2013/14 (1980-2013)”, Institute of Medical Biostatistics, Epidemiology and Informatics (IMBEI) at the University Medical Center of the Johannes Gutenberg University Mainz.
- Abed R, Grimer R (2010) Surgical modalities in the treatment of bone sarcoma in children. Cancer Treat Rev 36: 342-347.
- Hudson MM, Mertens AC, Yasui Y, Hobbie W, Chen H, et al. (2003) Health status of adult long-term survivors of childhood cancer: a report from the childhood cancer survivor study. JAMA 290: 1583-1592.
- Mansky P, Arai A, Stratton P, Bernstein D, Long L, et al. (2007) Treatment late effects in long-term survivors of pediatric sarcoma. Pediatr Blood Cancer 48: 192-199.
- Ness KK, Hudson MM, Ginsberg JP, Nagarajan R, Kaste SC, et al. (2009) Physical performance limitations in the childhood cancer survivor study cohort. J Clin Oncol 27: 2382-2389.
- Ginsberg JP, Goodman P, Leisenring W, Ness KK, Meyers PA, et al. (2010) Long-term survivors of childhood Ewing sarcoma: a report from the childhood cancer survivor study. J Natl Cancer Inst 102: 1272-1283.
- Fidler MM, Frobisher C, Guha J, Wong K, Kelly J, et al. (2015) Long-term adverse outcomes in survivors of childhood bone sarcoma: the British Childhood Cancer Survivor Study. Br J Cancer 112: 1857-1865.
- Eiser C, Darlington AS, Stride CB, Grimer R (2001) Quality of life implications as a consequence of surgery: limb salvage, primary and secondary amputation. Sarcoma 5: 189-195.
- Bekkering WP, Vliet Vlieland TP, Koopman HM, Schaap GR, Schreuder HW, et al. (2010) Quality of life in young patients after bone tumor surgery around the knee joint and comparison with healthy controls. Pediatr Blood Cancer 54: 738-745.
- Stokke J, Sung L, Gupta A, Lindberg A, Rosenberg AR (2015) Systematic review and meta-analysis of objective and subjective quality of life among pediatric, adolescent, and young adult bone tumor survivors. Pediatr Blood Cancer 62: 1616-1629.
- Gosheger G, Gebert C, Ahrens H, Streitbuerger A, Winkelmann W, et al. (2006) Endoprosthetic reconstruction in 250 patients with sarcoma. Clin Orthop Relat Res 450: 164-171.
- Winter C, Müller C, Brandes M, Brinkmann A, Hoffmann C, et al. (2009) Level of activity in children undergoing cancer treatment. Pediatr Blood Cancer 53: 438-443.
- Winter C, Müller C, Hoffmann C, Boos J, Rosenbaum D (2010) Physical Activity and Childhood Cancer. Pediatr Blood Cancer 54: 501-510.
- Götte M, Kesting SV, Winter CC, Rosenbaum D, Boos J (2015) Motor performance in children and adolescents with cancer at the end of acute treatment phase. Eur J Pediatr 174: 791-799.
- Kesting SV, Götte M, Seidel CC, Rosenbaum D, Boos J (2015) Motor performance after treatment for pediatric bone tumors. J Pediatr Hematol Oncol 37: 509-514.
- Ness KK, Mertens AC, Hudson MM, Wall MM, Leisenring WM,et al. (2005) Limitations on physical performance and daily activities among long-term survivors of childhood cancer. Annals Int Med 143: 639-647.
- Rueegg CS, von der Weid NX, Rebholz CE, Michel G, Zwahlen M, et al. (2012) Daily physical activities and sports in adult survivors of childhood cancer and healthy controls: a population-based questionnaire survey. Plos One 7: 34930.
- Wampler MA, Galantino ML, Huang S, Gilchrist LS, Marchese VG , et al. (2012) Physical activity among adult survivors of childhood lower-extremity sarcoma. J Cancer Surviv 6: 45-53.
- Hoffman MC, Mulrooney DA, Steinberger J, Lee J, Baker KS, et al. (2013) Deficits in physical function among young childhood cancer survivors. J Clin Oncol 31: 2799-2805.
- Götte M, Taraks S, Boos J (2014) Sports in pediatric oncology: the role(s) of physical activity for children with cancer. J Pediatr Hematol Oncol 36: 85-90.
- Braam KI, van der Torre P, Takken T, Veening MA, van Dulmen-den Broeder E , et al. (2016) Physical exercise training interventions for children and young adults during and after treatment for childhood cancer.Cochrane Database Syst Rev 30. CD008796.
- Baumann F, Bloch W, Beulertz J (2013) Clinical exercise interventions in pediatric oncology: a systematic review. Pediatr Res 74: 366-374.
- Rustler V, Hagerty M, Daeggelmann J, Marjerrison S, Bloch W, et al. (2017) Exercise interventinos for patients with pediatric cancer during inpatient cure: a systematic review of literature. Pediatric Blood Cancer 64.
- Kesting SV, Götte M, Seidel CC, Rosenbaum D, Boos J (2015) One in four questioned children faces problems regarding reintegration into physical education at school after treatment for pediatric cancer. Pediatr Blood Cancer 63: 737-739.
- Mössenböck B, Pamler G (2015) Schneesport ohne Handicap. In: Die Österreichische Skischule (3rdedn). Hollinek, Pukersdorf, Austria. Pg no: 457-521.
- Walter R (2010) Snowsport Austria Die Österreichische Skischule. Österreichischer Skischulverband (Hrsg.) Hollinek, Pukersdorf, Austria.
- Hobusch GM, Bollmann J, Puchner SE, Lang NW, Hofstaetter JG,et al. (2016) What sports activity levels are achieved after resection and endoprosthetic reconstruction for a proximal femur bone sarcoma? Clin Orthop Relat Res 475: 817-826.
- Nasuti G, Temple VA (2010) The risks and benefits of snow sports for people with disabilities: a review of the literature. Int J Rehabil Res 33: 193-198.
- Kesting S, Götte M, Seidel CC, Müller C, Michel T, et al. (2016) Bewegungs- und Sportförderung in der Pädiatrischen Onkologie am Universitätsklinikum Münster – Erfahrungen und Ergebnisse aus 5 Jahren. Bewegungstherapie und Gesundheitssport 32: 60-65.
Citation: Kesting S, Götte M, Boll E, Taraks S, Boos J, et al. (2017) Sarcoma on Ski: Individual Skiing Concepts Enable Autonomous Skiing After Multimodal Therapy for Pediatric Muscular-Skeletal Tumors. J Orthop Res Physiother 3: 034
Copyright: © 2017 Sabine Kesting, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

