
Should FEV1 be used to grade restrictive impairment? A single-center comparison of lung function parameters to 6-minute walk test in patients with restrictive lung disease
*Corresponding Author(s):
Roy Joseph ChoAssociate Professor Of Medicine, University Of Minnesota, Department Of Pulmonary, Allergy, Critical Care And Sleep Medicine, United States
Email:choxx548@umn.edu
Abstract
- Purpose
Evidence supporting current ATS guidelines for using FEV1 to grade severity of restriction is lacking. In this study, we surveyed the PFT interpretation practices of local pulmonologists for grading restrictive impairment; in addition, reviewed restrictive PFTs at our institution to determine which parameters best correlate with disease severity by 6-minute walk test (6MWT) results.
- Methods
We surveyed the PFT interpretation practices among local pulmonologists; then, performed a retrospective review of restrictive PFTs who had 6MWT. All spirometric reference values have been converted to Global Lung Initiative (GLI). We evaluated FEV1, forced vital capacity (FVC), functional residual capacity (FRC), TLC, and diffusing capacity of the lung for carbon monoxide (DLCO) to determine correlation with 6MWT.
- Results
The survey illustrated that TLC (72.7%) rather than FEV1 (4.55%) was the most common parameter used by local pulmonologists to grade restriction. We identified 911 PFTs as having RLD (average age was 58.7±13.4 years, males (63.8%), and BMI was 29.8±6.7). The most frequent causes for RLD was interstitial lung disease (ILD) (60%). 704 (77.28%) patients walked below the lower limit of normal (mean 327.11±4.36m). The FRC, TLC, and DLCO were the only parameters that were significantly associated with whether or not patients could complete the 6MWT (p=0.002, p=0.006, and p < 0.001, respectively). FEV1, FVC, FRC and TLC significantly affected either one or two parameters on 6MWT; however, DLCO was the only variable that was significantly associated with a completely abnormal 6MWT (p < 0.001).
- Conclusions
To our knowledge, this is the largest study investigating which spirometric and lung volume parameters are associated with RLD severity. Notably, DLCO was the only factor that was significantly associated with an abnormal 6MWT. Future studies comparing DLCO to clinical outcomes (i.e. hospitalization and mortality) would be warranted to corroborate our findings.
Keywords
Interstitial lung disease; Restrictive lung disease; Pulmonary function testing; Pulmonary fibrosis.
Introduction
Restrictive pattern on spirometry is associated with functional limitations, fair or poor self-reported health status, reduced physical performance and physical impairment in older adults, and increased morbidity and mortality [1,2]. Restrictive Lung Disease (RLD) has been classically characterized by a reduction in Total Lung Capacity (TLC) with a normal Forced Expiratory Volume in 1-second (FEV1) to Forced Vital Capacity (FVC) ratio [3]. The restrictive physiology is a function of pathological alterations in the lung parenchyma, pleura, chest wall, and/or neuromuscular system. Previous guidelines recommended the use of TLC and FVC as parameters to grade severity of restriction; however, the most recent guidelines recommend using FEV1 [4]. In our experience, we have noted local practice variations with regard to grading severity of restriction which may reflect the lack of clarity and evidence available. The purposes of this study are to investigate what the interpretation strategies are among local pulmonologist for determining the severity of RLD and to investigate which PFT parameters (FEV1, FVC, FRC, TLC, and DLCO) better reflect the severity of RLD based on six-minute walk test (6MWT) results.
Methods
This was a single-center retrospective cohort study conducted at the University of Minnesota Medical Center in Minneapolis, Minnesota. A waiver was granted for written informed consent. The human subject’s research committee of the local institutional review board approved the study protocol.
- Survey Analysis
A survey of 3 questions including
1) Number of years in practice,
2) Type of practice setting, and
3) Which parameter was used for grading restriction was sent to 50 adult pulmonologists actively practicing in the Twin Cities. The survey was constructed, emailed and resulted using SurveyMonkey.
- PFT Data Collection
To construct our data set, we retrieved data from our University of Minnesota pulmonary function test data base. Data was extracted using MGC Patient Query Version 8.50.27. Briefly, we queried patients 18 and above who had complete pulmonary function testing (spirometry, diffusion capacity and plethysmography) and a 6MWT during a 12-year period (2005 to 2017). Pulmonary function test (PFT) was performed using MGC Diagnostic Corporation (St Paul, Minnesota) Platinum Elite testing systems, using Breeze Suite 8.1 software according to ATS-ERS guidelines [4-9]. All test data that did not meet ATS-ERS standards were excluded from the study. If multiple PFT’s were recorded on the same individual, we included only the last PFT in our analysis. Patients included in the query were those who had an FVC < 80% and/or a TLC < 80%. We extracted demographic data from the chart (visit date, age, sex, height, weight, BMI, diagnosis, post-test comments and the pulmonologist interpretation of the test).
We maintained instruments according to manufacturer’s recommendations, calibrated daily with a 3-L syringe and performed routine biocontrol testing. Tests were included for analysis if they met the American Thoracic Society (ATS)/European Respiratory Society (ERS) acceptability and repeatability criteria in use at the time of testing. Categorization of restriction severity was determined using four variables: FEV1, FVC, FRC, TLC, and DLCO (uncorrected) which were then compared to the corresponding 6MWT results (walk distance, presence of hypoxia, and presence of oxygen desaturation. We determined a priori that the 6MWT would be our indicator for severity given established data [10-15].
- Statistical Analysis
Patient demographics and clinical characteristics were summarized and presented using descriptive statistics. To examine the relationship between the independent variables and the outcome variable (abnormal or normal 6MWT), both bivariate and multivariate analysis were performed. An abnormal 6MWT was defined as those who had less than the lower-limit-of-normal walk distance with significant desaturation and hypoxia defined as decrease in SpO2 <4% from resting SpO2 and SpO2 <88% during the test. Bivariate analyses were conducted using two-sample t tests or Chi-square tests depending on the nature of the variable. In multivariate analyses, multiple logistic regression models were developed to model the probability of abnormal. Full model included all independent variables and covariates (age, gender, and BMI). Backward selection was conducted to select the best subset of the variables in the final model. Analyses were performed using SAS 9.3 (SAS Institute, Cary NC).
Results
The results of the survey of local pulmonologists on grading patterns for restrictive lung disease is illustrated in Table 1. In this survey, the majority practiced in an academic center and had 10-20 years or more experience in interpreting PFTs (61.36% and 62.62%, respectively). The most common parameter used to grade restriction was TLC (72.7%), followed by FVC (20.45%), FEV1 (4.55%) and FEV/FVC ratio (2.27%).
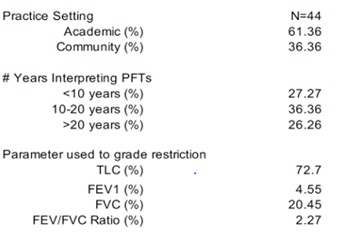 Table 1: Survey of RLD Interpretation by Local Pulmonologists
Table 1: Survey of RLD Interpretation by Local Pulmonologists
A total of 1200 PFTs were identified as restrictive during 2005-2017; however, 911 PFTs were used for our analysis following our exclusion criteria (see Methods). In these 911 patients, the mean age was 58.7 ± 13.4 years, and 63.8% were males. Approximately 848 (93%) patients completed a 6MWT, and 77.28% demonstrated reduced walk distance. The diagnoses associated with restrictive physiology were ILD (594.6, 60%), emphysema (91.1, 10%), chronic lung rejection (91.1, 10%), then musculoskeletal (49.55, 5%) and diaphragmatic paralysis (49.55, 5%). The baseline PFTs are illustrated in Table 2 (mean TLC 3.7 ± 1.1 L and DLCO 11.9 ± 5.6 mL/min/mmHg).
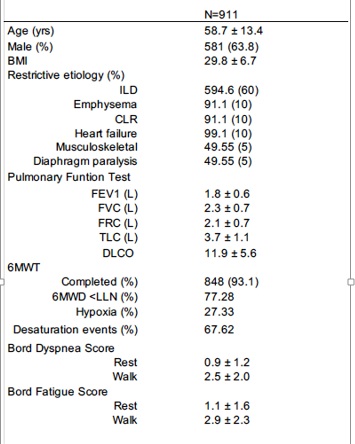 Table 2: Demographic and Baseline Pulmonary Function
Table 2: Demographic and Baseline Pulmonary Function
Tables 3 and 4 list the bivariate and multivariate assessment of the spirometric and lung volume parameters associated with a normal or abnormal 6MWT. In the bivariate assessment, each PFT parameter was compared to an either abnormal walk distance, desaturation or hypoxic event. Each parameter significantly affected either one or two 6MWT parameters (see Table 3). Notably, DLCO correlated best with all three 6MWT parameters (12.9 ± 5.6 (< 0.001), 8.6 ± 4.2 (< 0.001), and 0.68-0.77 (< 0.001). In the multivariate assessment, only DLCO significantly correlated with an abnormal 6MWT (0.73±4.2 [0.68-0.77], p< 0.001). Notably, FEV1 did not correlate with abnormal 6MWT in the multivariate analysis (1.8±0.6 [0.76-4.53], p=0.13).
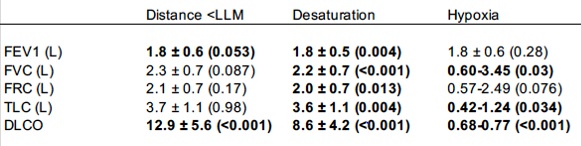 Table 3: Bivariate Analysis of Spirometric and Lung Volume Parameters vs 6MWT
Table 3: Bivariate Analysis of Spirometric and Lung Volume Parameters vs 6MWT
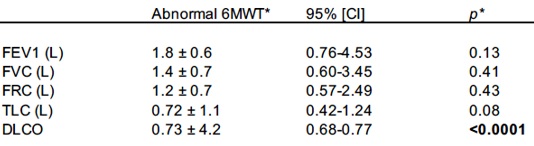 Table 4: Multivariate Analysis of Spirometric and Lung Volume Parameters on 6MWT
Table 4: Multivariate Analysis of Spirometric and Lung Volume Parameters on 6MWT
Discussion
Restrictive lung impairment occurs from either intrinsic and/or extrinsic etiologies. Intrinsic causes can be due to inflammation or fibrotic interstitial lung diseases (ILD) and extrinsic causes are associated with disorders of the chest wall, pleura, or neuromuscular disease affecting respiratory muscle function [16-18]. Although RLD is less common than its obstructive counterpart, centers that specialize in the evaluation of ILD and lung transplantation rely on the PFT assessment for restrictive severity; however, current guidelines demonstrate a lack of clarity and evidenced-based support for the best parameter to assess severity of this impairment. In clinical evaluation, a reduced TLC with evidence of impaired VC is interpreted as restriction; however, several factors may challenge these principles. First, measuring TLC in a population-based study is difficult since epidemiologic studies often use spirometry volume to assume a restrictive pattern when TLC measurements are unavailable [19]. Second, NHANES spirometric testing uses FVC along with the lower limit of normal (LLN) rather than TLC and VC to define a restrictive pattern on spirometry [20]. Third, past epidemiologic studies have used the Global Initiative for Chronic Obstructive Lung Disease fixed-ratio criteria for classifying a restrictive pattern on spirometry, including FVC < 80% predicted and FEV1/FVC ratio ≥ 0.7 [21]. Lastly, aging can be associated with physiological lungs changes affecting FEV1, FVC, and FEV1/FVC [22].
In this study, we have determined that local practice differs with respect to current guidelines grading restrictive impairment; this may be reflective of the lack of data supporting current guidelines. We found that all the spirometric and lung volume parameters had some significant correlation with certain 6MWT results. However, DLCO was the only PFT measurement that correlated with any 6MWT abnormality. Notably, we did not find that FEV1 was associated with an abnormal 6MWT (1.8±0.6 [0.76-4.53], p=0.13). To our knowledge, this is the first study investigating PFT parameters in patients with RLD and correlation with an abnormal 6MWT.
The data in this study are applicable to selected patients with RLD undergoing PFT and 6MWT. Our study was primarily designed to evaluate PFT parameters in comparison to an abnormal 6MWT; this study was not powered to assess differences in mortality outcomes. We selected abnormal 6MWT as the severity indicator given strong established data for symptom severity; therefore, other physiological assessments or surveys may incur different results. Despite these limitations, we feel that our findings are noteworthy in determining that FEV1 was not associated with an abnormal 6MWT compared to other measurements, i.e. DLCO.
In conclusion, there are differing practice patterns when interpreting severity of restrictive impairment which may be due to the lack of supporting data in current guidelines. In this large series of RLD in an academic institution, we found that DLCO, not FEV1, was the best PFT parameter in correlating with an abnormal 6MWT. Large prospective studies looking at hard clinical outcomes including hospitalization, supplemental oxygen requirement and mortality will need to be conducted to corroborate our findings.
Conflicts of interest
There is no conflict of interest by any of the authors.
Clinical Trials.gov Identifier
NA
References
- Mannino DM, Ford ES, Redd SC (2003) Obstructive and restrictive lung disease and functional imitation: data from the third national health and nutrition examination. J Intern Med 254:540-547.
- Guerra S, Sherrill DL, Venker C, Ceccato CM, Halonen M, et al. (2010) Morbidity and mortality associated with the restrictive spirometric pattern: a longitudinal study. Thorax 65: 499-504.
- Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, et al. (2005) ATS task force: Standardization of lung function testing: interpretive strategies for lung function tests. Eur Respir J 26: 948-968.
- Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, et al. (2005) ATS/ERS Task Force: tandardization of spirometry. Eur Respir J 26: 319-338.
- American Thoracic Society (1979) ATS statement: snowbird workshop on standardization of spirometry. Am Rev Respir Dis 119: 831-838.
- Statement of the American Thoracic Society (1987) Standardization of spirometry: 1987 update. Am Rev Respir Dis 136: 1285-1298.
- American Thoracic Society (1995) Standardization of spirometry, 1994 update. Am J Respir Crit Care Med 152: 1107-1136.
- Miller MR, Crapo R, Hankinson J, Brusasco V, Burgos F, et al (2005) ATS/ERS Task Force. General considerations for lung function testing. Eur Respir J 26:153-161.
- Graham BL, Brusasco V, Burgos F, Cooper BG, Jensen R, et al. (2017) 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lungs. Eur Respir J 49: 1-31.
- Lipkin DP, Scriven AJ, Crake T, Poole-Wilson PA (1986) Six-minute walking test for assessing exercise capacity in chronic heart failure. Br Med J 292: 653-655.
- 11 Cahalin LP, Mathier MA, Semigran MJ, Dec GW, DiSalvo TG (1996) The six-minute walk test predicts peak oxygen uptake and survival in patients with advanced heart failure. Chest 110: 325-332.
- Gomberg-Maitland M, Huo D, Benza RL, McLaughlin VV, Tapson VF, et al. (2007) Creation of a model comparing 6-minute walk test to metabolic equivalent in evaluating treatment effects in pulmonary arterial hypertension. J Heart Lung Transplant 26: 732-738.
- Guyatt GH, Pugsley SO, Sullivan MJ, Thompson PJ, Berman L, et al. (1984) Effect of encouragement on walking test performance. Thorax 39: 818-822.
- Bernstein ML, Despars JA, Singh NP, Avalos K, Stansbury DW, et al. (1994) Reanalysis of the 12-minute walk in patients with chronic obstructive pulmonary disease. Chest 105: 163-167.
- 15 Baughman RP, Sparkman BK, Lower EE (2007) Six-minute walk test and health status assessment in sarcoidosis. Chest 132: 207-213.
- Coultas DB, Zumwalt RE, Black WC, Sobonya RE (1994) The epidemiology of interstitial lung diseases. Am J Respir Crit Care Med 150: 967-972.
- Widmann RF, Bitan FD, Laplaza FJ, Burke SW, DiMaio MF, et al. (1999) Schneider R. Spinal deformity, pulmonary compromise, and quality of life in osteogenesis imperfect. Spine 24: 1673-1678.
- Mangera Z, Panesar G, Makker H (2012) Practical approach to management of respiratory complications in neurological disorders. Int J Gen Med 5: 255-263.
- Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, et al. (2005) Interpretative strategies for lung function testing. Eur Respir J 26: 948-968.
- National center for health statistics: plan and operation of the third national health and nutrition examination survey 1988-1994.
- Global initiative for chronic obstructive lung disease: GOLD spirometry guide for health care providers.
- Janssens JP, Pache JC, Nicod LP (1999) Physiological changes in respiratory function associated with ageing. Eur Respir J 13: 197-205.
Citation: Larson J, Wrzos K, Corazalla E, Wang Q, Kim H, et al. (2023) Should FEV1 be used to grade restrictive impairment? A single-center comparison of lung function parameters to 6-minute walk test in patients with restrictive lung disease. J Pulm Med Respir Res 9: 082.
Copyright: © 2023 Jeffrey Larson, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

