
Single US Guided HA Injection Reduced Hip Pain and Improved Function for 20 Months: A Case of Osteonecrosis
*Corresponding Author(s):
Asmaa Mahmoud Ali MoustafaDepartment Of Physical Medicine, Rheumatology And Rehabilitation, Department Of Clinical Sciences And Translational Medicine, Tor Vergata University, Ain Shams University, Cairo, Egypt; Rome, Italy, Italy
Tel:+20 1006415074; +39 8812935378,
Email:dr.asmaa.mahmoud@hotmail.com; mhmsma01@uniroma2.it
Abstract
Hip Osteoarthritis (OA) and Osteonecrosis (ON) are two separate kinds of arthropathies; each has its distinct features regarding epidemiology, histopathology and radiographic findings. However both could be presented with similar arthritis-like symptoms, and may result in marked pain and disability which eventually ends with Total Hip Arthroplasty (THA). In this case report, we present a 67 years old male has hip ON with osteoarthritic component; surgery was a treatment option however, the patient described unexpected long term amelioration after single US guided Hylastan SGL80 injection upon his refusal to THA. Results showed continuous significant improvement in Visual Analogue Scale (VAS), McGill Pain Questionnaire (McGill), Western Ontario McMaster Questionnaire (WOMAC), Lequesne Index, and tenderness scale up to 20 months follow up, even in the presence of femoral head collapse. Hyaluronic acid (HA) could be a feasible option to treat painful osteonecrotic hip when THA is not applicable or refused by the patient.
Keywords
INTRODUCTION
In addition to THA and joint preserving procedures [4,5], non-operative management was described in literature [6], this includes drugs such as anticoagulants, bisphospohanates and vasodilators [7-10] or physical modalities as extra-corporeal shock wave treatment, pulsed electromagnetic therapy, and hyperbaric oxygen [11-13]. The results of these different treatment options vary according to diverse factors based on patient and lesion characteristics [14,15]. However the ultimate goal of all suggested treatments in ON management was the reservation of the involved hip with less concern to resolve the symptomatic problems secondary to the osteoarthritic component of the osteonecrotic hip.
Visco supplementation with exogenous Hyaluronic Acid (HA) has become lately one of the most widely used treatment in osteorthritis, it is suggested to be one of the best conservative therapy before surgery, acting on pain relief and function. There are few data about the use of HA in other hip disorders rather than osteoarthritis, with no definite evidence to prove its ability to modify the morphological structure of the pathological hip and the natural history of the disease. The most relevant evidence seems to show the utility of HA injections in improving synovial inflammation, with only a few studies have been conducted [16], the timing of treatment, the volume of the HA doses employed, and the correct indication for HA use, such as the more suitable phenotypes or stages of OA, especially for joints other than the knee, is still unclear, and controversial [17,18].
Here within we report a long term clinical improvement of 67 years old male with hip ON, that was maintained over a period of 20 months following single ultrasound guided injection of 4 ml Hylastan SGL-80.
CASE REPORT
The patient described right hip pain (dominant hip) started January 2012 following dancing for long time in the previous night, the pain was of gradual onset, progressive course, partially improved with rest, later the pain worsened at the end of the day especially after prolonged weight bearing and climbing stairs. The patient declared that this pain was associated with stiffness and significant impairment of daily activities. Paracetamol was taken in case of pain exacerbation.
The physical examination revealed limited range of motion of the right hip in abduction, internal and external rotation with painful adduction and external rotation, tenderness was positive in anterior, posterior and lateral hip, antalgic gait was observed, spine and left hip joint evaluation was irrelevant, for radiological evaluations at baseline and 20 months post injection (see Table 1).
| Radiological examination | Date | Findings |
| Baseline | ||
| Plain X-ray | 27-09-2012 | Bilateral osteoarthritis with signs of a vascular necrosis of the proximal femoral epiphysis more evident on the right side. |
| MRI | 25-01-2012 | Reduction of articular space of right hip. Right femoral head has an area of hypo intense signal that becomes hyper intense on sequences merging with intra- and peri-articular fluid expressing reactive synovitis as signs of necrotic bone.Left femoral head shows vugs formation. With subchondral distress of acetabular roof bilaterally.No pathological changes in signal intensity of myotendinous structures at the site of interest. |
| 20 months post-injection | ||
| Plain X-ray | 26-09-2014 | Marked osteoarthritis, bone resorption of the femoral head with slight collapse of the upper bone profile, most probably osteonecrosis. |
| MRI | 15-09-2014 | Images were taken in axial and coronal planes using SE, TSE, TIRM sequences.The right femoral head is oval in shape, with signal alteration of the antero-medial side, (49 mm) heterogeneously hyperintense signal intensity on T2-weighted images and hypointense on T1-weighted images, bounded by sclerotic margin denoting avascular necrosis. Associated with cancellous bone edema. Concomittant intra-articular synovial reaction.Acetabular marginal osteophytic irregularities, with degenerative changes of labrum, joint space narrowing with thinning of articular hyaline cartilage. subcondral cysts are seen on both sides of the left joint with mild reactive synovitis |
Our impression - based on the patient’s history, clinical examination, and radiographic findings - was that the patient’s symptoms arose directly from the degenerative osteoarthritic changes of the articular surface associated with right femoral head osteonecrosis.
After discussing the risks, benefits, and alternatives of treatment options, the patient chose to go for viscosupplimentation. Single ultrasound guided injection of 4 ml Hylastan SGL-80 was prescribed, to be followed by exercise program to improve hip Range of Motion (ROM) and muscle strength. Appointments for the procedure and follow up visits were fixed.
METHOD
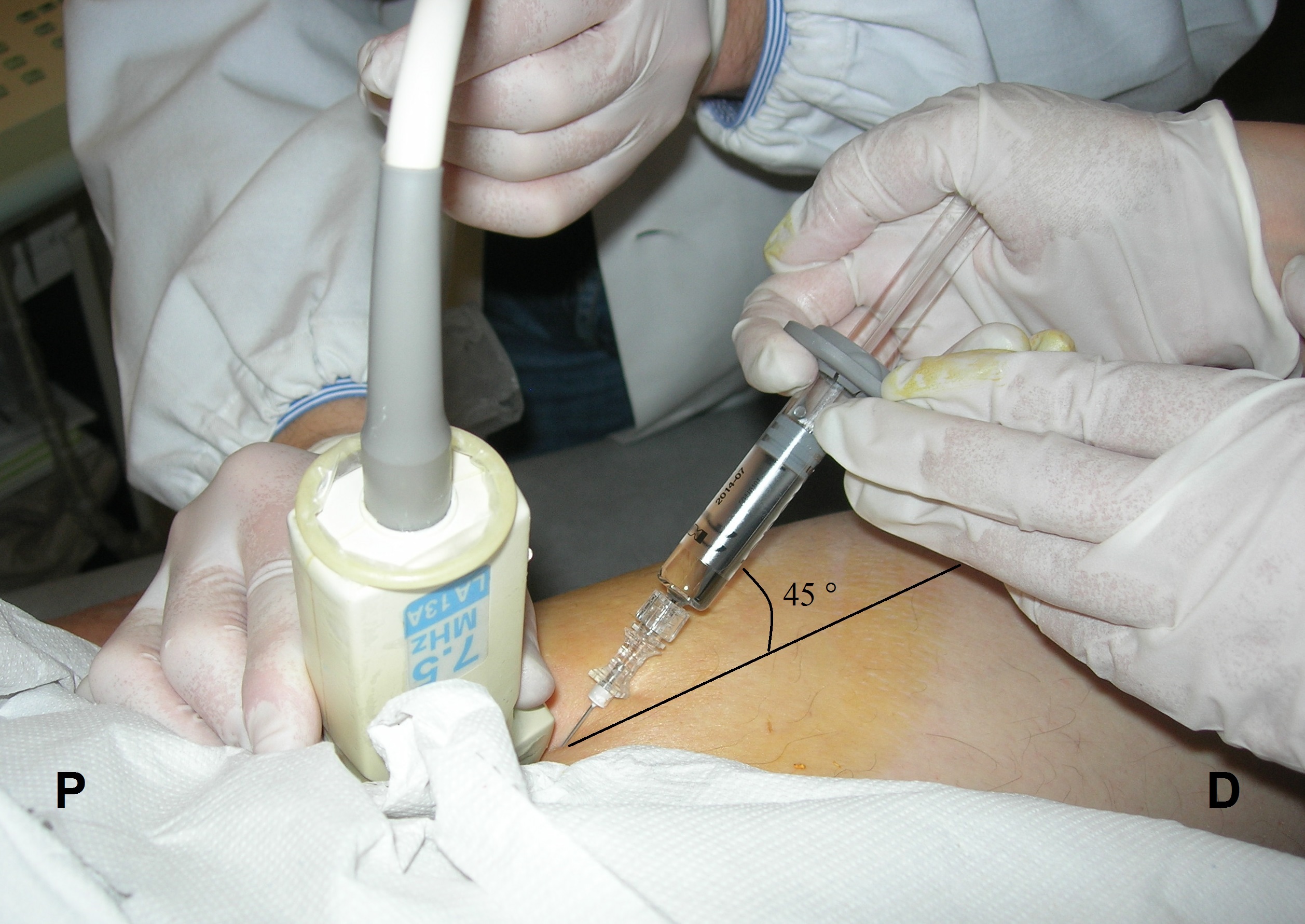
Figure 1: 4 ml of Hylastan SGL-80 injected under real time ultrasound guidance. P, Proximal; D, Distal.
The main outcome measures for assessment of the injection efficacy applied before and after injection were: Visual Analogue Scale (VAS), McGill Pain Questionnaire (McGill) and Western Ontario McMaster Questionnaire (WOMAC), Lequesne Index, and tenderness scale [19] that was considered positive if at least one side of the hip joint - anterior, lateral or posterior - is tender on palpation. Patient was followed 1 month, 3, 6, 12, 18, and 20 months post-injection (T1, T2, T3, T4, T5, T6 respectively).
RESULTS
The percentage of the change in applied scales was calculated and compared to baseline (T0), results revealed significant clinical improvement in all time points with observation of complete absence of hip pain at 6 and 12 months post injection as measured by VAS and McGill (Table 2), the trend of improvement toward T6 showed ups and downs without reaching to baseline values in any of the scales except VAS at T1 and T5 (Figure 2). Clinical evaluation compared to first assessment described before, showed pain-free ROM with partial improvement regarding the limitation of internal/external rotation and abduction over the time points from T2 till T6, absence of limping and joint tenderness on palpation in all time points since one month till 20 months after injection.
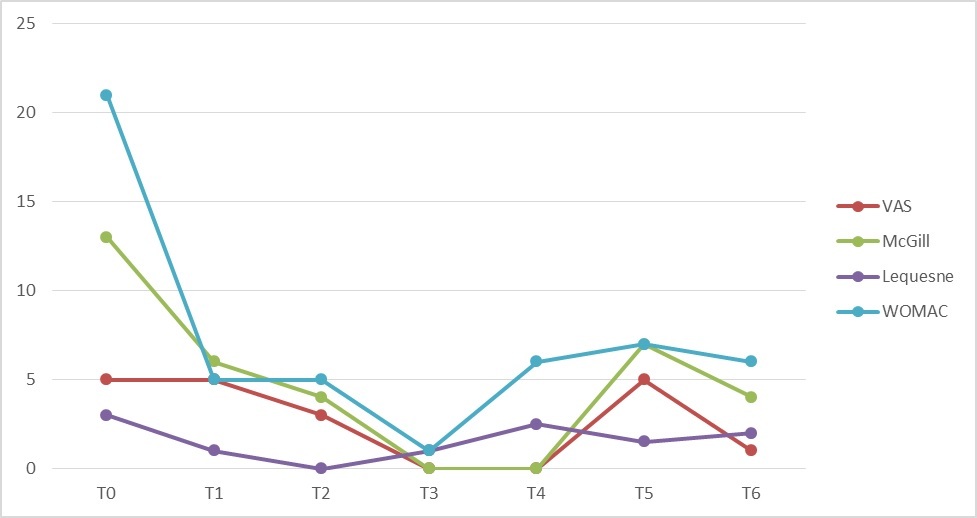
Figure 2: Trend of improvement of outcome measures from baseline till 20 months post-injection (T0-T6), without reaching to baseline values in any of the scales except VAS at T1 and T5. With complete absence of hip pain at 6 and 12 months post injection, VAS, Visual Analogue Scale; McGill, McGill Pain Questionnaire; WOMAC, Western Ontario McMaster Questionnaire.
| Scales | T0 | T1 | T0/T1% | T2 | T0/T2% | T3 | T0/T3% | T4 | T0/T4% | T5 | T0/T5% | T6 | T0/T6% |
| VAS | 5 | 5 | 0 | 3 | -40 | 0 | -100 | 0 | -100 | 5 | 0 | 1 | -80 |
| McGill | 13 | 6 | -54 | 4 | -69 | 0 | -100 | 0 | -100 | 9 | -31 | 4 | -69 |
| Lequesne | 3 | 1 | -67 | 0 | -100 | 1 | -67 | 2.5 | -17 | 1.5 | -50 | 2 | -33 |
| WOMAC | 21 | 5 | -76 | 5 | -76 | 1 | -95 | 8 | -62 | 8 | -62 | 6 | -71 |
*McGill: McGill Pain Questionnaire
*WOMAC: Western Ontario McMaster Questionnaire
DISCUSSION
Among these conservative measures, supplementation of hyaluronic acid was not suggested as a treatment option, instead it is mentioned in literature as the main endogenous component of the extracellular matrix in ischemic necrosis, with suggestions that quantity analysis of HA can be used as a good indicator in early diagnosis and prognosis of femoral head ON [22,23].
HA injection in hip disorders rather than OA was reviewed using various combinations of key words and mesh terms including: hyaluronic acid, hyaluronic injections, hip joint, hip osteoarthritis, hip diseases, rheumatoid arthritis, femoral head avascular necrosis, hip dysplasia, femoroacetabular impingement, hip disorders, hip cartilage, conservative treatment. No studies identified about HA efficacy in femoral head avascular necrosis [16].
In spite of the long term improvement in the pain and function of the treated hip in our case, the HA effect in protecting the femoral head from collapse cannot be assumed. Nothing was found in literature in this regard and to the best of our knowledge no study has tested HA injection as one of conservative modalities in hip ON. On the other hand, Osteonecrosis of the femoral head often results in secondary osteoarthritis of the hip joint [24]; the maintained amelioration in our case after single HA injection could be through improving the physiological environment of the associated osteoarthritic changes by restoring the protective viscoelasticity of synovial fluid [25,26], which possibly was the main source of patients` pain and dysfunction rather than the Osteonecrotic process itself.
Our results gives a chance for HA to be suggested as an option for effective symptomatic treatment in hip ON specially when THA is refused by the patient, not applicable or needed to be postponed. Literature is missing clear information about its safety and efficacy in such cases. Randomized controlled trials are required to investigate the impact of HA Intra-articular injection on hip disruption in different stages of femoral necrosis, while the ability of the external HA supplementation to substitute the degraded HA in the necrotic bone is a matter of discussion.
CONCLUSION
REFERENCES
- Hernigou P, Trousselier M, Roubineau F, Bouthors C, Chevallier N, et al. (2016) Stem Cell Therapy for the Treatment of Hip Osteonecrosis: A 30-Year Review of Progress. Clin Orthop Surg 8: 1-8.
- Pivec R, Johnson AJ, Harwin SF, Mont MA (2013) Differentiation, diagnosis, and treatment of osteoarthritis, osteonecrosis, and rapidly progressive osteoarthritis. Orthopedics 36: 118-125.
- Zeng Y, Qi X, Feng W, Li J, Li F, et al. (2015) One-sided hip-preserving and concurrent contralateral total hip arthroplasty for the treatment of bilateral osteonecrosis of the femoral head in different stages: short-medium term outcomes. BMC Musculoskelet Disord 16: 133.
- Israelite C, Nelson CL, Ziarani CF, Abboud JA, Landa J, et al. (2005) Bilateral core decompression for osteonecrosis of the femoral head. Clin Orthop Relat Res 441: 285-290.
- Seyler TM, Marker DR, Ulrich SD, Fatscher T, Mont MA (2008) Nonvascularized bone grafting defers joint arthroplasty in hip osteonecrosis. Clin Orthop Relat Res 466: 1125-1132.
- Johannson HR, Zywiel MG, Marker DR, Jones LC, McGrath MS, et al. (2011) Osteonecrosis is not a predictor of poor outcomes in primary total hip arthroplasty: a systematic literature review. Int Orthop 35: 465-473.
- Glueck CJ, Freiberg RA, Sieve L, Wang P (2005) Enoxaparin prevents progression of stages I and II osteonecrosis of the hip. Clin Orthop Relat Res 435: 164-170.
- Agarwala S, Shah SB (2011) Ten-year follow-up of avascular necrosis of femoral head treated with alendronate for 3 years. J Arthroplasty 26: 1128-1134.
- Jager M, Tillmann FP, Thornhill TS, Mahmoudi M, Blondin D, et al. (2008) Rationale for prostaglandin I2 in bone marrow oedema: from theory to application. Arthritis Res Ther 10: 120.
- Disch AC, Matziolis G, Perka C (2005) The management of necrosis-associated and idiopathic bone-marrow oedema of the proximal femur by intravenous iloprost. J Bone Joint Surg Br 87: 560-564.
- Alves EM, Angrisani AT, Santiago MB (2009) The use of extracorporeal shock waves in the treatment of osteonecrosis of the femoral head: a systematic review. Clin Rheumatol 28: 1247-1251.
- Massari L, Fini M, Cadossi R, Setti S, Traina GC (2006) Biophysical stimulation with pulsed electromagnetic fields in osteonecrosis of the femoral head. J Bone Joint Surg Am 88: 56-60.
- Camporesi EM, Vezzani G, Bosco G, Mangar D, Bernasek TL (2010) Hyperbaric oxygen therapy in femoral head necrosis. J Arthroplasty 25: 118-123.
- Amanatullah DF, Strauss EJ, Di Cesare PE (2011) Current management options for osteonecrosis of the femoral head: part II, operative management. Am J Orthop (Belle Mead NJ) 40: 216-225.
- Malizos KN, Karantanas AH, Varitimidis SE, Dailiana ZH, Bargiotas K, et al. (2007) Osteonecrosis of the femoral head: etiology, imaging and treatment. Eur J Radiol 63: 16-28.
- Piccirilli E, Oliva F, Murè MA, Mahmoud A, Foti C, et al. Viscosupplementation with intra-articular hyaluronic acid for hip disorders. A systematic review and meta-analysis. Muscles Ligaments Tendons J 6: 293-299.
- Castañeda S, Roman-Blas JA, Largo R, Herrero-Beaumont G (2014) Osteoarthritis: a progressive disease with changing phenotypes. Rheumatology (Oxford) 53: 1-3.
- Strand V, McIntyre LF, Beach WR, Miller LE, Block JE (2015) Safety and efficacy of US-approved viscosupplements for knee osteoarthritis: a systematic review and meta-analysis of randomized, saline-controlled trials. J Pain Res 8: 217-228.
- Hubbard DR, Berkoff GM (1993) Myofascial trigger points show spontaneous needle EMG activity. Spine (Phila Pa 1976) 18: 1803-1807.
- Castro FP, Jr, Barrack RL (2000) Core decompression and conservative treatment for avascular necrosis of the femoral head: a meta-analysis. Am J Orthop (Belle Mead NJ) 29: 187-94.
- Mont MA, Cherian JJ, Sierra RJ, Jones LC, Lieberman JR (2015) Nontraumatic Osteonecrosis of the Femoral Head: Where Do We Stand Today? A Ten-Year Update. J Bone Joint Surg Am 97: 1604-1627.
- Luo N, Yang D, Fu Z, Sun W, Chen S (1998) [Hyaluronic acid and laminin in patients with ischemic necrosis of femoral head]. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi 15: 291-293.
- Kato S, Yamada H, Terada N, Masuda K, Lenz ME, et al. (2005) Joint biomarkers in idiopathic femoral head osteonecrosis: comparison with hip osteoarthritis. J Rheumatol 32: 1518-1523.
- Jingushi S, Lohmander LS, Shinmei M, Hoerrner LA, Lark MW, et al. (2000) Markers of joint tissue turnover in joint fluids from hips with osteonecrosis of the femoral head. J Orthop Res 18: 728-33.
- Hui AY, McCarty WJ, Masuda K, Firestein GS, Sah RL (2012) A systems biology approach to synovial joint lubrication in health, injury, and disease. Wiley Interdiscip Rev Syst Biol Med 4: 15-37.
- Henrotin Y, Raman R, Richette P, Bard H, Jerosch J, et al. (2015) Consensus statement on viscosupplementation with hyaluronic acid for the management of osteoarthritis. Semin Arthritis Rheum 45: 140-149.
Citation: Moustafa AMA, Massimiani A, Oliva F, Foti C (2017) Single US Guided HA Injection Reduced Hip Pain and Improved Function for 20 Months: A Case of Osteonecrosis. J Orthop Res Physiother 3: 029
Copyright: © 2017 Asmaa Mahmoud Ali Moustafa, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

