
The Association between Beta-Natriuretic Peptide (BNP) Serum Levels and Liberation from Mechanical Ventilation
*Corresponding Author(s):
Edward P ManningSection Of Pulmonary, Critical Care, And Sleep Medicine, Yale School Of Medicine VA Connecticut Healthcare System, West Haven, CT, United States
Email:edward.manning@yale.edu
Abstract
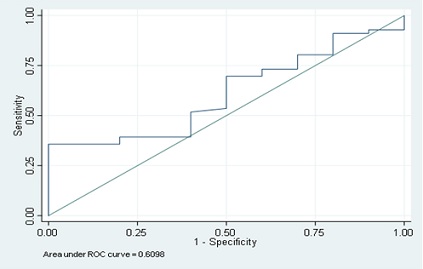
Prolonged time on mechanical ventilation is associated with multiple consequences for both the patient and medical facility. Based on anecdotal evidence that sustained elevation of beta-natriuretic protein (BNP) during a patient’s stay in a Long-Term Acute Care Hospital (LTACH) was associated with failure to wean from prolonged mechanical ventilation, we investigated if there is an association between a decrease in BNP levels during one’s stay and successful weaning from prolonged mechanical ventilation. We performed a retrospective study of 66 patient records revealing no correlation between lowering BNP levels and probability of liberating a patient from prolonged mechanical ventilation in an LTACH environment where the probability of liberation from mechanical ventilation is high (> 85%). BNP measurements by itself does not appear to be a helpful tool in the likelihood of liberation from mechanical ventilation AUC = 0.61 (CI: 0.48-0.72). In an LTACH setting with high success rates of liberation from mechanical ventilation, it does not appear to be necessary to trend BNP measurements in attempts to liberate patients from prolonged mechanical ventilation.
Keywords
BNP; Intubation; LTACH; Ventilation
Background
Prolonged time on mechanical ventilation is associated with multiple consequences for both the patient and medical facility-decreased quality of life, increased medical expenses, and extensive use of medical material and personnel [1,2]. Identifying associations or correlations with liberation from mechanical ventilation may be predictive of potential patients with the greatest chances of successfully weaning from prolonged ventilation ideally within a 30-day stay [2-4]. This knowledge would allow physicians to better prognosticate clinical courses for patients and their families. It would also allow for economical use of resources for patients who would benefit most from them. We noted anecdotal evidence within our LTACH, a highly active LTACH in the Northeast United States, that sustained elevation of beta-natriuretic protein (BNP) during a patient’s stay was associated with failure to wean from prolonged mechanical ventilation. There is literature to support our observations [5,6]. We explored whether the inverse was true-if there is an association between a decrease in BNP levels during one’s stay at LTACH and successful weaning from prolonged mechanical ventilation. If such as association exits, it is possible that elevated BNP in a patient suffering from prolonged mechanical ventilation may serve as a prognostic indicator for successful liberation from mechanical ventilation with proper clinical support.
Methods
We performed a retrospective study of electronic medical records to record serial BNP measurements, supplemental oxygen/ventilator settings, and clinical outcomes. Gaylord patients who experienced prolonged mechanical ventilation, defined as requiring mechanical ventilation for 21 days or more from time of initial intubation (intubation not required to have been performed at Gaylord) or determination by outside hospital that patient is “unable to wean from vent,” were enrolled. These patients also needed to have at least two BNP measurements during stay at Gaylord separated by two or more days. We excluded patients: on dialysis, with stage III or greater chronic kidney disease (estimated GFR < 30 mL/min/1.73 m2), on non-invasive ventilation, and were transferred in-house (that is, patients transferred from within one section of Gaylord Hospital to another for more acute care; the hope is to apply the finding of this study to populations of individuals who are already suffering from prolonged mechanical ventilation at the time of their transfer to Gaylord). We reviewed the EMR of 216 patients that appeared to have two or more BNP’s measured during their stay at Gaylord. There was sufficient information to analyze 66 of these cases.
Results And Discussion
There does not appear to be any correlation between lowering BNP levels and the probability of liberating from prolonged mechanical ventilation. In cases where the BNP lowered from abnormally high level to a normal level, the chances of liberating from a vent was 82% (CI: 57-96%). In cases where the BNP remained or increased above the normal range the chances of liberating from a vent was 86% (CI: 73-94%). This means that changes in BNP levels have little association with liberation from prolonged mechanical ventilation. Additional analysis revealed that any decrease in BNP had an 87% (CI: 72-96%) probability of predicting liberation from prolonged mechanical ventilation. BNP elevation or stable levels had an 82% (CI: 63-94%) probability of predicting for vent liberation.
The ROC curve below generated from our data demonstrates that BNP measurements by itself is not a helpful tool in the likelihood of liberation from mechanical ventilation. The area under the curve (AUC) should be as close to 1.0 as possible to maximize utility of a test. Our AUC = 0.61 (CI: 0.48-0.72). AUC of 0.50 is the 45-degree line basically representing flipping a coin to guess whether a test value will help you predict your desired result. Our data is stepwise and follows the 45-degree line closely.
Conclusion
Of the 66 cases, only 10 were not liberated from the vent, equating to an 85% success rate of weaning from mechanical ventilation for these Gaylord patients. There are many factors involved with weaning patients from prolonged mechanical ventilation. Fluid status is likely one of them; however, BNP values by themselves are likely not helpful to the physician in changing the clinical course of the patient. We suspect BNP measurements are one of the many tools that an experienced Gaylord physician uses to gauge a patient’s volume status and liberate someone from prolonged mechanical ventilation but should not be a sole instrument to predict a patient’s chances of liberating from prolonged mechanical ventilation. These results may be very helpful to avoid unnecessary testing. In the hands of seasoned professional practitioners, there appears to be no need for trending BNP’s in attempts to liberate patients from prolonged mechanical ventilation in long-term acute care hospitals.
Acknowledgement
The research reported/outlined here was supported by the Department of Veterans Affairs, Veterans Health Administration, and VISN 1 Career Development Award to EPM. EPM is a Pepper Scholar with support from the Claude D. Pepper Older Americans Independence Center at Yale School of Medicine (P30AG021342), NIA R03AG074063-01A1, and Additional Ventures.
The authors have not had industry relationships in the past two years. The authors are grateful to Laurie Jano, RT, for her assistance in conducting this study. Approval of this study was made by the Gaylord Hospital Institutional Review Board (IRB). Informed consent was obtained from all individual participants included in the study.
References
- Bach JR (1995) Indications for tracheostomy and decannulation of tracheostomized ventilator users. Monaldi Arch Chest Dis 50: 223-227.
- Hernández G, Ortiz R, Pedrosa A, Cuena R, Vaquero Collado C, et al. (2012) The indication of tracheotomy conditions the predictors of time to decannulation in critical patients. Med Intensiva 36: 531-539.
- Enrichi C, Battel I, Zanetti C, Koch I, Ventura L, et al. (2017) Clinical Criteria for Tracheostomy Decannulation in Subjects with Acquired Brain Injury. Respir Care 62: 1255-1263.
- Winck JC, LeBlanc C, Soto JL, Plano F (2015) The value of cough peak flow measurements in the assessment of extubation or decannulation readiness. Rev Port Pneumol 1: 94-98.
- Mekontso Dessap A, Roche-Campo F, Kouatchet A, Tomicic V, Beduneau G, et al. (2012) Natriuretic peptide–driven fluid management during ventilator weaning: a randomized controlled trial. American journal of respiratory and critical care medicine 186: 1256-1263.
- Nawas ZY, Clardy N, Greene P, Shah N, Leeper KV (2010) Changes in B-Type Natriuretic Peptide During Ventilator Weaning in Cardiothoracic Surgical Patients Admitted to a Long-term Acute Care Facility. Chest 138: 582A.
Citation: Weil KA, Baumann V, Brown B, Nadeau R, Gerstenhaber B, et al. (2023) The association between beta-natriuretic peptide (BNP) serum levels and liberation from mechanical ventilation. J Pulm Med Respir Res 9: 075.
Copyright: © 2023 Kimberly A Weil, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

