
The Effectiveness of a 12-week Exercise Programme in Hip OsteoArthritis: A Randomised Controlled Trial
*Corresponding Author(s):
Anabel ScirihaDepartment Of Physiotherapy, Faculty Of Health Sciences, Room 32 Mater Dei Hospital Msida, Malta
Email:anabel.sciriha@um.edu.mt
Abstract
Purpose: Osteoarthritis (OA) is a common disease caused by the destruction of the joint cartilage. Pain, stiffness and dysfunction during activities of daily living are common reasons leading to a hip arthroplasty. Programmes based on quadriceps strengthening are now evidence-based. Therefore, this study aims to explore and investigate the effects of a 12-week hip exercise programme on pain and functional levels.
Methods: This study reports outcomes of a randomised controlled trial. 40 participants were randomly allocated into 2 groups: control group and an intervention group. All participants were asked general demographic data at baseline, followed by assessment using the NPRS, WOMAC Scale, 6 MWT and muscle testing. Participants in the control group received no intervention, whereas the others performed hip exercises. A 12-week exercise programme resulted in highly statistically significant improvements for participants in the intervention group and minimal changes for the control group.
Results: Data is presented for both groups respectively as follows: 6MWD P<0.001, P=0.928; NPRS P=0.035, P=0.325; WOMAC P < 0.001, P=0.032.
Conclusion: A 12-week exercise programme resulted in clinical and statistically significant improvements for the intervention group.
Keywords
Arthritis; Management; Physiotherapy; Rehabilitation
Introduction
Osteoarthritis (OA) is one of the most common joint disorders worldwide [1,2], a condition which is responsible for pain, stiffness, and dysfunction during activities of daily living. One of the functional capacities affected by OA is deterioration in muscle strength mainly of the quadriceps, hamstrings, and other musculature around the hip [3-5].
An overwhelming amount of literature is available supporting the use of exercise to help manage or decrease joint pain as a result of knee OA, programmes which including muscle strengthening, aerobic/cardiovascular exercise and more [6-12]. Evidence based research about management through exercise of Hip OA is though limited. So as to counteract the limited information, guidance through recommendations for the non-pharmacological management of Hip OA were issued by the European League Against Rheumatism (EULAR) Osteoarthritis Task Force stating these patients should receive tailored programmes which include both long and short-term goals or action plans, regular evaluation by healthcare professionals and follow-up with the possibility of adjusting the programme accordingly [13]. These recommendation have been further supported by more recent guidelines issued by the American Physical Therapy Association 2017 [14]. the Ottawa Panel Clinical Practice Guidelines [15-17]. which although specific to knee OA, make reference to the hip, and the Osteoarthritis Research Society International (OARSI) guidelines, 2019 [18]. The latter set recommendations for flexibility, strengthening and endurance exercises aimed at addressing impairments in hip ROM, muscle weaknesses and reduced flexibility. These guidelines also recommend that for the dosage and duration to be effective, the exercises should be carried out 1-5 times per week over a 6-12 week period but this is still inconclusive and the duration still varies from as little as 6 weeks to up to 4 months.
Results from studies offer varied outcomes. In a randomised trial by Bieler et al [10], 4 months of either physiotherapist-supervised, moderate, progressive, strength training (n = 50), physiotherapist-supervised Nordic Walking (n = 50), or unsupervised Home-Based Exercises (n = 52) showed no differences in muscle strength and active hip ROM with the authors suggesting that the patients recruited might not have been able to achieve the target load prescribed and that muscle strength and functional performance might not be correlated.
Svege et al [18] evaluated the effects of exercise therapy and patient education in a 12-week exercise programme, one which resulted in no beneficial long-term effects except for the significantly reduced pain levels reported during the 6-minute walk test at the 10th and 29th month. Svege et at [18] claimed that their participants had mild functional limitations at baseline, adherence to the programme was reported in 53% of the participants only and that the exercise programme may have been ineffective in dosage progression and execution of the exercises.
In contrast to the above, a 10-week programme of progressive explosive-type resistance training resulted in significant improvements in self-reported outcomes and increased lower limb muscle power [19]. This study reported significant improvements in self-reported ADL function, as well as leg muscle power.
Despite the vast amount of literature available on exercise in the management of most knee OA, research on the management of Hip OA is limited and no consensus regarding the optimal time-frame and dosage has yet been established. Therefore the authors aimed at investigating outcomes of a 12-week exercise programme in patients with Hip OA.
Methodology
- Experimental approach
This paper reports a randomised controlled trial. Data obtained from both groups were recorded at the start of week 0 and the end of week 12. By adopting this design, a pre and post test method of data collection was implemented with all participants undergoing a series of outcome measures at the start of the study as described below and retested on all the participants upon completion of a 12-week intervention.
- Subjects
All 340 participants who were waiting for a total hip replacement at the local hospital were eligible to participate. A total of 40 patients accepted to participate. In order to be recruited, participants had to be aged 40 years or over. Participants whom on assessments were found to have unstable cardiovascular or respiratory disorders, had recent lower limb surgery, had a condition affecting lower limb function, were unable to mobilise or were not able to commit to the exercise programme were excluded from the study. Procedures of recruited are outlines in Figure 1.
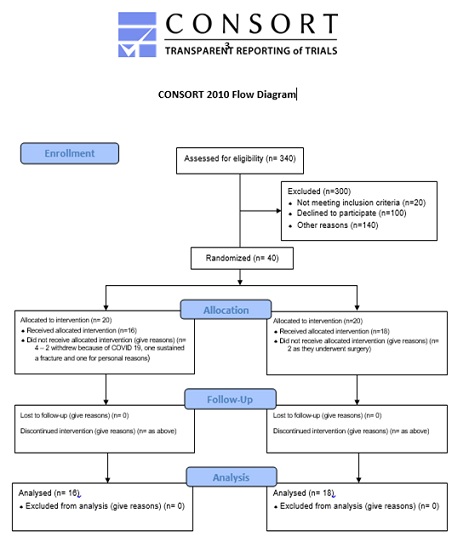 Figure 1. Caption: Consort 2010 flow diagram.
Figure 1. Caption: Consort 2010 flow diagram.
- Procedures
At baseline, all participants were asked general demographic data including age, weight, height, body mass index (BMI), gender and drug history. The following outcome measures were then carried out on every subject at baseline (Week 0) and repeated at week 12.
- Numerical pain rating scale (NPRS)
The NPRS is a widely used in the clinical setting aswell as in research [20]. It is a simple and valid tool to use with acceptable construct validity for this tool (P < 0.001).
- Western Ontario and McMaster universities scale and the 6 minute walking test
Functional Levels were assessed using the Western Ontario and McMaster Universities (WOMAC) Scale and a 6 MWT. The WOMAC is a widely used instrument which is specific to assessing patients with hip and knee OA [21]. This assessment tool was self-administered. It consists of 33 items which evaluate the health and function of the patient from various aspects including clinical symptoms (5 questions), severity of joint stiffness (2 questions), degree of pain (9 questions), and activity of daily living (17 questions).
The six-minute walk test (6MWT) measures the distance an individual is able to walk over a total of 6minutes on a hard, flat surface. The individual was allowed to self-pace and rest as needed as they traverse back and forth along a marked walkway. Such a test has been reported to be a valid and reliable indicator of aerobic fitness [22]. The subjects were instructed that they could stop and rest during the test, but the time kept running. At the end of the test, the distance covered was recorded.
- Muscle torque testing
All subjects also underwent peak isometric lower limb muscle torque testing for the following muscle groups: Quadriceps, Hamstrings, Adductors and Abductors using the Lafayette Hand held dynamometer. A maximum of three attempts were performed with the average result taken. Participants were instructed to exert maximal effort and were verbally coached to push as hard as they could for each recorded trial.
All patients were randomly assigned using a random computer generator to one of 2 groups by the intermediary: the control group who were awaiting surgery and were not receiving any regular physiotherapy and the Intervention group, who were subject to a set of hip exercises based on a protocol described by Deyle et al [23]. These exercises were carried out 3 times weekly for a period of 3 months. During the first 4weeks, all sessions were supervised by a physiotherapist, independent to this study who monitored and increased the duration or difficulty of exercises according to patients’ progression. From the 5th to the 8th week, patients were requested to attend 2 supervised sessions and complete the third one at home. Between the 9th and the 12th week, patients attended one supervised intervention and completed 2 exercise sessions at home. All patients were given a copy of the exercise sheet with instructions for use at home.
- Statistical analysis
Data was analysed using the statistical package for social science (SPSS) software version 27 to determine any significant changes over time between both groups using the ANOVA test. Comparision of outcomes at the 12th week between both groups was carried out using the Independent Sample’s T-test. Effect sizes were calculated to identify the extent of the experimental effect using an online calculator:
https://www.socscistatistics.com/effectsize/default3.aspx.
Ethical approval was also obtained from the University Faculty Research Ethics Committee and registered with clinicaltrials.gov, having identifier number NCT04771936.
Results
The intervention lasted 12 weeks, with 34 patients completing the study. In the control group 2 participants were excluded from the study as they underwent a hip arthroplasty. In the intervention group, 4 participants withdrew for the following reasons: one participant sustained a fracture of her ribs, two participants quit attending because of an increase in Covid-19 cases and one participant dropped for personal reasons. Table 1 outlines the baseline characteristics of all the participants of both groups.
|
Baseline characteristics n= 51 |
Mean Value (SD) |
|
|
|
|
Gender |
Males - 28 Females - 23 |
|
Age (years) |
60 years or less – 16 61-69 years – 21 70 years or more - 14 |
|
Affected hip |
Right hip – 25 Left hip -21 Bilateral hips affected - 5 |
|
Weight (kg) |
83.65 (+16.55) |
|
Height (cm) |
161.79 (+ 9.92) |
|
BMI (kg/cm2) |
31.96 (+5.89) |
|
6MWT (m) |
267.82 (+ 108.34) |
|
NPRS |
5.31 (+ 2.59) |
|
WOMAC |
49.63 (+ 19.69) |
|
Core Stability |
Good - 18 Poor - 33 |
Table 1 : Baseline characteristics of all participants enrolled in the study.
N= number of participants; SD= standard Deviation; kg= kilograms; cm= centimetres; BMI= Body Mass Index; 6MWT= 6 Minute Walk Test; NPRS= Numerical Pain Rating Scale; WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index
Outcome measures
Six Minute walk distance (6MWD)
As can be noted in Figure 2, significant improvements in the 6 minute walking distance were recorded for participants in the intervention group. After 12 weeks of rehabilitation, a statistically significant increase in walking distance of 43m from a mean baseline value of 262.63m (SD 118.27) to 305.69m (SD 131.42), P< 0.001 (ES d=0.34) was obtained. Such improvements were not noted in participants of the control group. These participants registered no difference in walking distance from a mean baseline value of 257.94m (SD 127.80) at week 0 to a mean walking distance of 256.94m (SD 137.81) at week 12, p=0.928 (ES d=0.01).
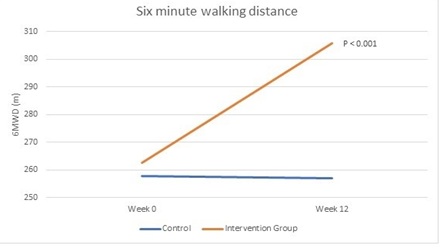 Figure 2. Caption: A graphical representation of changes in the 6MWD from baseline to week 12. Statistically significant changes are noted in the graph, through the representation of the p-value. N.B. 6MWD (m)= Six-minute walk distance measured in metres.
Figure 2. Caption: A graphical representation of changes in the 6MWD from baseline to week 12. Statistically significant changes are noted in the graph, through the representation of the p-value. N.B. 6MWD (m)= Six-minute walk distance measured in metres.
Numerical pain rating scale (NPRS)
As is demonstrated in Figure 3, participants of the intervention group registered a significant decrease in pain levels of P= 0.035, ES d=0.49 (mean baseline NPRS score of 5.88 [SD 2.68] at week 0 to 4.56 [SD 2.71] at week 12). Once again, such positive changes were not observed in participants of the control group, who registered an increase in pain values of 11% from their baseline (NPRS at week 0 4.67 [SD 2.87] to 5.17 [SD 2.92] at week 12), P=0.325, ES d= 0.17.
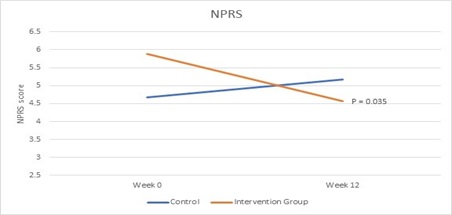 Figure 3, Caption: A graphical representation of changes in the NPRS from baseline to week 12. Statistically significant changes are noted in the graph, through the representation of the p-value. N.B. NPRS= Numerical Pain Rating Scale.
Figure 3, Caption: A graphical representation of changes in the NPRS from baseline to week 12. Statistically significant changes are noted in the graph, through the representation of the p-value. N.B. NPRS= Numerical Pain Rating Scale.
Western ontario McMaster universities osteoarthritis index (WOMAC)
Following a 12-week exercise intervention, a significant improvement in the impact of OA in participants forming part of the intervention group of 11%, P<0.001, ES d=0.32 resulted. This group scored a value of 57.31 (SD 18.39) at week 0 to 51.25 (SD 19.04) at week 12. As per the previous two outcomes the control group registered worsening of their score by 5% over 12 week (45.94 [SD 21.36] at week 0 to 48.44 [SD 22.70] at week 12), P= 0.032, ES d= 0.11. These changes are graphically represented in Figure 4.
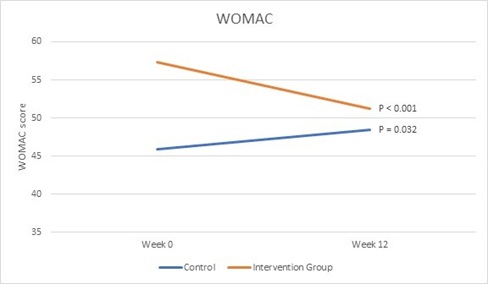 Figure 4, Caption: A graphical representation of changes in the WOMAC score from baseline to week 12 per individual group. Statistically significant changes are noted in the graph, through the representation of the p-value.
Figure 4, Caption: A graphical representation of changes in the WOMAC score from baseline to week 12 per individual group. Statistically significant changes are noted in the graph, through the representation of the p-value.
N.B WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
Muscle strength
Hip Abductors: Muscle strength of the hip abductors for the control group improved slightly on both sides, but did not reach statistical significance (Right hip mean baseline value= 5.98 [SD 2.67] to 6.20 [SD 2.74] after 12 weeks, P=0.606, ES d=0.08; Left hip mean baseline value= 5.85 [SD 3.11] to 6.23 [SD 3.30], P=0.210, ES d=0.12). The intervention group had significant improvements in muscle strength of the left side and despite not statistically significant, a marked improvement on the right (Right hip mean baseline value= 7.23 [SD 3.64] to 7.71 [SD 3.04] after 12 weeks, P=0.381, ES d= 0.14; Left hip mean baseline value= 6.02 [SD 2.99] to 7.33 [SD 2.94] after 12 weeks, P=0.014, ES d= 0.44).
Hip Adductors: A statistically signifcant decline in hip adductor muscle strength on both the right and left side (Right hip mean baseline value= 5.22 [SD 1.99] to 4.41 [SD 0.93], P=0.038, ES d= 0.53; Left hip mean baseline value= 4.39 [SD 1.67] to 3.74 [SD 1.21] after 12 weeks, P=0.014, ES d= 0.45) was noted for the control group. Statistically significant improvements were then obtained for participants in the intervention group (Right hip mean baseline value= 4.31 [SD 1.84] to 5.62 [SD 2.57], P=0.024, ES d= 0.59; Left hip mean baseline value= 4.12 [SD 2.83] to 5.73 [SD 2.83] after 12 weeks, P=0.010, ES d= 0.57).
Hip Extension: Participants in the control group registered a non statistically significant decline in muscle strength of the hip extenstors (Right hip mean baseline value= 4.09 [SD 2.84] to 3.78 [SD 2.45], P=0.376, ES d= 0.12; Left hip mean baseline value= 4.54 [SD 2.69] to 4.17 [SD 2.39], P=0.323, ES d= 0.46). A highly statistically significant increase in hip extensor muscle strength was registered for the intervention group (Right hip mean baseline value= 3.27 [SD 2.10] to 5.91 [SD 2.41], P<0.001, ES d= 1.17; Left hip mean baseline value= 3.69 [SD 2.54] to 5.88 [SD 2.84], P=0.003, ES d= 0.81).
Hip Lateral Rotators: Muscle strength for the hip lateral rotators in participants of the control group resulted in a deterioration, with the right side having a statistically significant decline in muscle strength as opposed to the left side (Right hip mean baseline value= 5.01 [SD 1.93] to 4.46 [SD 1.52] after 12 weeks, P=0.035, ES d= 0.32; Left hip mean baseline value= 4.76 [SD 2.05] to 4.32 [SD 1.53] after 12 weeks, P=0.233, ES d= 0.24). The intervention group, registered a statistically significant improvement recorded on the right side but not on the left despite an improvement in strength too (Right hip mean baseline value= 4.84 [SD 1.42] to 6.01 [SD 2.37] after 12 weeks, P=0.014, ES d= 0.6; Left hip mean baseline value= 4.91 [SD 1.36] to 5.71 [SD 2.06] after 12 weeks, P=0.107, ES d= 0.46).
Discussion
A 12 week exercise programme for patients with hip OA resulted in statistically significant improvements in most outcome measures with participants enrolled into the control group showing minimal improvements.
A statistically significant, 22% decline in pain scores for participants in the intervention group was noted (P=0.035, ES d=0.49) whereas participants enrolled into the control group had a slight increase in their pain levels by 0.5 (50% increase). 12weeks of exercises therefore resulted in an ideal period to lead to improvements in pain, to the contrary of what Uusi-Rasi et al [24] reported. These authors stated that 12 weeks might be a short time for effective progression in training, since this might lead to a rapid increase in exercise intensity which could have adverse effects on pain levels, one which might dishearten participants to continue with treatment. Patients enrolled in the intervention group were being constantly monitored along the course for intensity progression which might have been one of the factors leading to such an improvement. Results obtained through this study are supported by Hernandez et al [25] who reported a significant reduction in pain behaviour in their participants, an intervention based on a three-times weekly sessions for 12 weeks, a protocol which was similar to what was carried out in this research study. A 12-week exercise intervention also matches recommendations issued by the American College of Sports Medicine (ACSM) pertaining to strength training. Hernandez et al (25) noted a marked reduction in the use of NSAIDs with these authors stating that despite this effect being a short-lasting one, the exercises might help in reducing or delaying the need of surgical intervention. Although not yet conclusive as to whether 12 or more supervised sessions are superior, it is reported that pain and physical function appear to improve further when this time frame is taken into consideration [26,27].
With a reduction in pain levels, the other outcomes also showed positive outcomes. A 12 week rehabilitation programme resulted in a relatively marked improvement in lower limb muscle strength for participants in the intervention group, but not for the control group. These benefits can be linked to the exercise progamme composition and also the duration of the programme. The revised 2017 clinical practice guidelines of the American Physical Therapy Association, highly consider with a grade A, the use of flexibility, strengthening and endurance exercises. Since muscle strength and pain levels improved, it is expected that the impact of OA on the individual will be ameliorated and also functionality. This could be seen from the 10.6% decline in WOMAC scores for the intervention group, ES d=0.32. The control group, on the otherhand had an increase of 5.4% in the WOMAC score.
A change in WOMAC score of 7.9 has been reported to be a minimal clinical important improvement in patients with hip OA as reported by Tubach [28] a value which was obtained in participants of the intervention group. The degree of short-term improvements in ADLs, physical performance and quality of life has been related by Hoglund et al [29] to the volume of supervised exercise received by the participants. Patients in the intervention group also reported a gain of 43m in the 6MWD, having a small magnitude ES of d=0.34. The control group on the other hand scored 1m less in distance from baseline in their 6-minute walking distance. Similar findings were reported by Widmer et al [30].
This study had some limitations one of which was the lack of proper monitoring of the HEP compliance using a diary/telephone communication, aspects which would have helped assess continuity of the exercises prescribed. The sample size for this study was also a small one and large sample groups will provide a better outline to outcomes from such an intervention
Conclusion
This 12-week exercise intervention on a group of participants suffering from symptoms related to hip OA, resulted in clinical and statistically significant improvement in pain levels, functionality and lower limb strength. Such benefits follow the 2017 clinical practice guidelines for the use of flexibility, strengthening and endurance exercises in the rehabilitation for patients with hip arthritis.
Conflicts of interest
The authors declare that there are no conflicts of interest
Funding
The authors declare that there was no funding received to conduct this study.
Acknowledgements
The authors would like to thank all the participants who participated in this study
References
- Vos PAJM, Mastbergen SC, Huisman AM, Boer TND, Groot JD, et al. (2012) In end stage osteoarthritis, cartilage tissue pentosidine levels are inversely related to parameters of cartilage damage. Osteoarthritis and Cartilage 20: 233-240.
- Cross M, Smith E, Hoy D, Nolte S, Ackerman I, et al. (2014) The global burden of hip and knee osteoarthritis: Estimates from the global burden of disease 2010 study. Annals of the rheumatic diseases 73: 1323-1330.
- O'Reilly SC, Jones A, Muir KR, Doherty M (1998) Quadriceps weakness in knee osteoarthritis: The effect on pain and disability. Ann Rheum Dis 57: 588-594.
- Costa RA, Oliveria LMD, Watanabe SH, Jones A, Natour J (2010) Isokinectic assessment of the hip muscles in patients with osteoarthritis of the knee. Clinics 65: 1253-1259.
- Hinman RS, Hunt MA, Creaby MW, Wrigley TV, McManus FJ, et al. (2010) Hip Muscle Weakness in Individuals with Medial Knee Osteoarthritis 62: 1190-1193.
- Wellsandt E, Golightly Y (2018) Exercise in the management of knee and hip osteoarthritis. Current Opinion Rheumatology 30: 151-159.
- Bartholdy C, Klokker L, Bandak E, Bliddal H, Henriksen M (2016) A standardized “rescue” exercise program for symptomatic flare-up of knee osteoarthritis: description and safety considerations. Journal of orthopaedic & sports physical therapy 46: 942-946.
- Bartholdy C, Juhl C, Christensen R, Lund H, Zhang W, et al. (2017) The role of muscle strengthening in exercise therapy for knee osteoarthritis: A systematic review and meta-regression analysis of randomized trials. Seminars in arthritis and rheumatism 47: 9-21.
- Bennell KL, Nelligan RK, Kimp AJ, Wrigley TV, Metcalf B, et al. (2019) Comparison of weight bearing functional exercise and non-weight bearing quadriceps strengthening exercise on pain and function for people with knee osteoarthritis and obesity: Protocol for the TARGET randomised controlled trial. BMC Musculoskeletal Disorders 20: 291.
- Bieler T, Siersma V, Magnusson SP, Kjaer M, Beyer N (2018) Exercise induced effects on muscle function and range of motion in patients with hip osteoarthritis. Physiotherapy Research International 23: 1697.
- Aguiar GC, Rocha SG, Rezende GADS, Nascimento MR, Scalzo PL (2016) Effects of resistance training in individuals with knee osteoarthritis. Fisioterapia Em Movimento 29: 589-596.
- Rooij MD, Leeden MVD, Cheung J, Esch MVD, Häkkinen A, et al. (2017) Efficacy of Tailored Eexercise Therapy on Physical Functioning in patients With Knee Osteoarthritis and Comorbidity: A Randomized Controlled Trial. Arthritis Care Research (Hoboken) 69: 807-816.
- Zhang W, Doherty M, Arden N, Bannwarth B, Bijlsma J, et al. (2005) EULAR evidence-based recommendations for the management of hip osteoarthritis: report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Annals of the rheumatic diseases 64: 669-681.
- Cibulka MT, Bloom NJ, Enseki KR, Camero WMD, Judith Woehrle PT, et al. (2017) Hip Pain and Mobility Deficits - Hip Osteoarthritis: Revision 2017. Journal of Orthopaedic & Sports Physical Therapy 47: 1-37.
- Brosseau L, Taki J, Desjardins B, Odette T, Marlene F, et al. (2017) The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part three: Aerobic exercise programs. Clinical Rehabilitation 31: 612-624.
- Brosseau L, Taki J, Desjardins B, Odette T, Marlene F, et al. (2017) The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part two: strengthening exercise programs. Clinical Rehabilitation 31: 596-611.
- Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, et al. (2019) OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis and Cartilage 27: 1578-1589.
- Svege I, Fernandes L, Nordsletten L, Inger H, May AR, et al. (2016) Long-Term Effect of Exercise Therapy and Patient Education on Impairments and Activity Limitations in People With Hip Osteoarthritis: Secondary Outcome Analysis of a Randomized Clnical Trial. American Physical Therapy Association 96: 818-827.
- Hermann A, Holsgaard-Larsen A, Zerahn B, Mejdahl S, Overgaard S, et al. (2016) Preoperative progressive explosive-type resistance training is feasible and effective in patients with hip osteoarthritis scheduled for total hip arthroplasty - a randomiszed controlled trial. Osteoarthritis and Cartilage 24: 91-98.
- The British Pain Society(2019) Outcome Measures.
- Ebrahimzadeh M, Makhmalbaf H, Birjandineja A, Farideh G K, Hosein AH, et al. (2014) The Western Ontario and MCMaster Universities Osteoarthritis Index (WOMAC) in Persian Speaking Patients with Knee Osteoarthritis. The Archives of Bone and Joint Surgery 2: 57-62.
- Enright PL (2003) The six-minute walk test. Respiratory care 48: 783-785.
- Deyle GD, Henderson NE, Matekel RL, Ryder RL, Garber MB, et al. (2000) Effectiveness of Manual Physical Therapy and Exercise in Osteoarthritis of the Knee. Annals of Internal Medicine 132: 173-181.
- Uusi-Rasi K, Patil R, Karinkanta S, Kari T, Pekka K, et al. (2017) Exercise Training in Treatment and Rehabilitation of Hip Osteoarthritis: A 12-Week Pilot Trial. Journal of Osteoporosis.
- Hernandez D, Dimaro M, Navarro E, Javier D, Matías A , et al. (2019) Efficacy of core exercises in patients with osteoarthritis of the knee: A randomized contolled clinical trial. Joutnal of Bodywork & Movement Therapies 23: 881-887.
- Skou ST, Roos EM (2019) Physical therapy for patients with knee and hip osteoarthritis: Supervised, active treatment is current best practice. Clinical and Experimental Rheumatology 37: 112-117.
- Moseng T, Dagfinrud H, Smedslund G, Østerås N (2017) The importance of dose in land-based supervised exercise for people with hip osteoarthritis. A systematic review and meta-analysis Osteoarthritis and Cartilage 25: 1563-1567.
- Tubach F, Baron G, Falissard B, Logeart I, Dougados M, et al. (2005) Using patients’ and rheumatologists’ opinions to specify a short form of the WOMAC function subscale. Annals of the rheumatic diseases 64: 75-79.
- Hoglund LT, Pontiggia L, Kelly JD (2008) A 6-week hip muscle strengthening and lumbopelvic-hip core stabilization program to improve pain, function, and quality of life in persons with patellofemoral osteoarthritis: A feasibility pilot study. BioMed Central 4: 1-14.
- Widmer P, Oesch P, Bachmann S (2022) Effect of Prehabilitation in Form of Exercise and/or Education in Patients Undergoing Total Hip Arthroplasty on Postoperative Outcomes-A Systematic Review. Medicina 58: 742.
Citation: Dalmas I, Sciriha A, Agius TP (2023) The Effectiveness of a 12-week Exercise Programme in Hip OsteoArthritis: A Randomised Controlled Trial. J Orthop Res Physiother 9: 060.
Copyright: © 2023 Ilona Dalmas, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

