
The Management of Adult Male Prisoners with Substance Use Disorders Presenting with Suspected Internal Concealment of Illicit Drugs: Challenges, Clinical Implications, and Best Practice Response
*Corresponding Author(s):
John Arianda Owiti, PhD, RMNAdvanced Clinical Practitioner, Independent Prescriber & Multi-Professional Approved Clinician Trainee, Oxleas NHs Foundation Trust, Lesney Ward, The Woodlands Unit, Queen Mary’s Hospital, Frognal Avenue, Sidcup, Kent DA14 6LT, United Kingdom
Email:john.owiti@nhs.net
Abstract
Purpose: Internal concealment as a means of trafficking illicit drugs into prison is common and exposes internal concealers to risk of intoxication and overdose death. The management of internal drug concealment is a medical emergency that remains a challenge to healthcare professionals and custodial officers in prison settings. Despite this, there is currently no structured, systematic approach to aid the process. The aim of this article is to review current processes, highlight deficits, and provide recommendations to aid effective clinical management of prisoners suspected of internally concealing illicit drugs.
Methodology: Three case studies are discussed to illustrate the areas where improvements are needed to maintain patient safety. These include intra-prison communication regarding potential concealment on prisoner transfer and appropriate clinical intervention.
Findings: Although no patients experienced adverse outcomes, several issues are highlighted, including lack of custodial staff awareness on the risks of internal drug concealment, lack of clinical monitoring for deterioration, provision of maintenance therapy to a patient known to be concealing drugs, and absence of a defined protocol to aid the clinical management of patients.
Originality: This study highlights key challenges faced by the prison service and proposes a clinically informed algorithm for the management of prisoners suspected to have internally concealed illicit drugs. Provision of training to healthcare and custodial staff, and collaborative multi-disciplinary working between healthcare staff and custodial officers is necessary to improve current practice.
Keywords
Body packing; Body stuffing; Illicit drugs; Internal concealment; Prison; Protocol
Introduction
Illicit drugs are those prohibited under international drug control treaties [1]. Internal Concealment of Illicit Drugs (ICIDs) for trafficking into prisons through arrivals has been a medical issue since 1973 [2]. This method of transportation is common, risky, and challenging to recognize and manage, especially when prisoners are alcohol and/or opiate dependent. Between 1997 and 2002, 16 out of 45 drug-related deaths in custody in England and Wales occurred in individuals known or believed to have concealed drugs by ingestion at point of police contact [3] and recent evidence points to an increase in drug-related deaths in prisons [4], with latest records showing that 88 of 1830 total deaths identified as being drug-related (mostly opiates) [5], were largely due to drug toxicity following delayed identification of deterioration, variable implementation of resuscitation, and the time taken to receive medical attention [3,6,7].
Despite the scale of the problem, data on the direct relationship between ICIDs and the risk of drug-related morbidity and mortality are sparse, and there is no broad consensus on best clinical practice management. The responses that have been developed [8,9] mainly apply to the emergency department setting and currently no protocol exists on the clinical management of prisoners suspected to have internally concealed illicit drugs in the prison setting. This clinical review was motivated by the death of a prisoner in custody from a drug overdose, just one day after being recalled to prison [10], and its focus is to present an algorithm designed to aid the management of individuals identified as having internally concealed illicit drugs within a prison setting.
- Categories of internal illicit drug concealers
There are three categories of internal illicit drug transporters: body packers, often referred to as “internal carriers”, “couriers”, or “mules” [9,11,12], body pushers, and body stuffers [12]. Each present with distinct risks and complications, making it important to determine the type of concealment, ideally while taking the patient’s history.
Body stuffers voluntarily but quickly swallow or insert relatively small amounts of poorly wrapped or unpackaged drugs into body cavities, typically to avoid detection or to destroy evidence [8,11-15,]. Common places for concealment include the oesophageal cavity/stomach, rectum, or female genitalia [16-19]. Because there was no initial plan to transport illicit drugs, they may be poorly packaged, leaving body stuffers at high risk of acute intoxication and overdose death [8,11,14,20-22]. With body stuffing being a common method for holding and transporting illicit drugs into prisons [23,24], cases of drug overdose or toxicity in custodial settings are likely to be among body stuffers.
Body packing and body pushing, also referred to as intracorporeal drug concealment, refers to either voluntary or coercive swallowing or inserting through the rectum or female genitalia securely wrapped drugs for transportation or storage [8,12,22,25-32]. The size and number of packets concealed varies, and each packet typically contains many times the toxic dose of the drug [12,33]. Due to the pre-planned nature of the internal concealment, the packaging is generally more sophisticated than that used by body stuffers, resulting in a lower risk of packets leaking, rupturing, or causing intestinal obstruction or visceral perforation [12,30,34].
- Identification and management of prisoners suspected of internal concealment of illicit drugs on prison entry
In prisons, the challenges of managing ICIDs are encountered mostly in Reception, Induction Wing and the Care and Separation Unit (CSU). In Reception, all prisoners are now screened using X-ray body scanners, and urine drug screens are commonly carried out as part of the first-night reception assessment process for those with substance use problems. However, a urine drug screen has limited value in identifying drug concealers because a positive result may be due to drug use, and a negative test may still occur if a concealed package is intact [12]. Ordinarily when internal concealment is suspected, the prisoner would be placed in a holding room, and offered use of a toilet, then re-scanned. If no item is found on second search no further action is taken, and the prisoner would go to an ordinary prison wing.
Prisoners suspected of internal concealment are transferred to the CSU, where healthcare staff use the Initial Segregation Health Screen (Supplementary Figure S1) to confirm that there are no risks or clinical reasons to contraindicate care in the CSU. The prisoner is then allocated a CSU cell to pass out the concealed package(s) and thereby restrict the flow of illicit drugs.
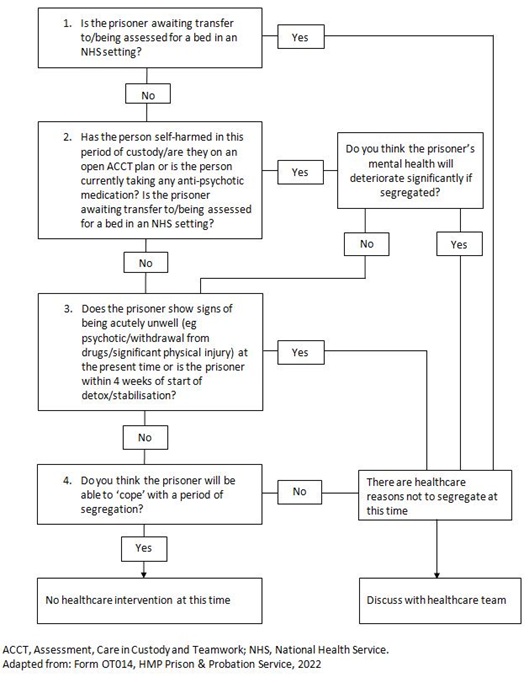 Figure S1: The initial segregation health screen.
Figure S1: The initial segregation health screen.
In our experience, being transferred to the CSU is often perceived as punitive by prisoners, and could lead to withholding of crucial information (e.g., drug type, quantity, packaging materials, and time of ingestion) that would be beneficial in guiding clinical management and optimizing outcomes. It is important to stress that, until signs of drug intoxication are noticed and reported to the healthcare team, prisoners in the CSU are not under close observation from trained healthcare personnel. In some cases, prisoners are suspected to have ICIDs when they are already on the Induction Wing. Such prisoners would have been commenced on clinical treatment for substance use disorder(s).
Methods
- Setting
A retrospective service evaluation was carried out in a Substance Misuse Service (SMS) provided by Oxleas NHS Foundation Trust within HMP Thameside, a local prison in South London that holds up to 1,232 male prisoners. The prison admits an average of 90 prisoners each month with substance use disorders requiring clinical interventions. The SMS provides clinical intervention for prisoners diagnosed with opiate, benzodiazepines, and alcohol addictions. Patients with substance use disorders suspected to have internally concealed illicit drugs were identified via a retrospective case-control audit of SystmOne, an electronic medical record system, between January and June 2021.
- Study population
The study population consisted of prisoners with a diagnosis of substance misuse disorder [35], who were suspected to have internally concealed illicit drugs at Reception on entry into prison or identified on the Induction Wing.
- Ethical considerations
The SMS is an NHS service provided by Oxleas NHS Foundation Trust as part of Public Health England’s commissioned service, and all the data obtained were for the purposes of audit aimed at care quality improvement. Although we did not require formal ethical approval to collect data for improvement of quality of care and safety of patients under our care, Oxleas NHS Foundation Trust granted approval. The prisoners’ identifiers have been anonymized to ensure confidentiality.
Results
Sixteen cases of suspected internal illicit drug concealment were detected (Appendix 1). Prisoners were mostly White and were aged between 29 and 49 years. Other details of the overall population are summarized in table 1.
|
Parameter |
Prisoners (n=16) |
|
Mean age, years (range) |
40 (29-49) |
|
Ethnicity, n White British Bangladeshi Indian Black |
10 4 1 1 |
|
Location of concealment notification, n Reception Induction Wing |
8 8 |
|
Sentence status, n Convicted Recalled On remand |
6 1 9 |
|
Marital status, n Married Single |
2 14 |
|
Employment status, n Unemployed Employed |
15 1 |
|
Housing status, n Homeless Tenant Homeowner Living with parent |
13 1 1 1 |
|
Education status, n None General Certificate of Secondary Education National Vocational Qualification City and Guilds Other |
9 1 2 3 1 |
|
Co-occurring disorders, n Mental and substance use Physical illness |
8 8 |
Table 1: Characteristics of sixteen prisoners suspected of internal illicit drug concealment.
Twelve prisoners had been in police custody before being taken to court, while three were directly remanded into prison by the court. Some prisoners reported internally concealing illicit drugs to avoid arrest (n=2) or help them get through the time in police custody (n=3), but others declined to volunteer reasons. Five prisoners concealed illicit drugs for personal use. No prisoners perceived the practice as posing a risk to their health and all were known to the criminal justice system. Though all prisoners had a history of opioid use disorder and had been on Opiate Substitution Treatment (OST) during previous incarcerations, only two were on OST with methadone in the community. None of the prisoners handed over any illicit substances they were suspected of concealing to the prison. Three patients who were already started on both alcohol detox and methadone had these stopped following reports that they were suspected of ICIDs. Fourteen prisoners were started on treatment following clearance. However, the cases demonstrate that the risk of acute narcotic intoxication, gastrointestinal obstruction, and emergency laparotomy remains high. This is evidenced by the fact that six prisoners located on Induction Wing had been started on treatment, while three had been prescribed medication in Reception and nursing staff were informed just as they were about to be medicated. The prisoners who had been started on treatment while having ICIDs were at high risk of intoxication. Fortunately, there were no cases of fatal intoxication.
To emphasize the scale of the problem and highlight the risks and complexities of managing prisoners suspected of ICIDs, as well as the inadequacy of the current clinical pathway to address their medical needs, we present the cases of three prisoners (Table 2). We have included a Prisons and Probation Ombudsman report of a prisoner (Mr Nathan Forrester) who died of drug toxicity who was suspected to have transported drugs with him into prison for context and to emphasize the risk of overdose death in prisoners who have been initiated into treatment but still have access to illicit drugs (Appendix 2).
|
Case 1: Mr A |
|
Mr A, a 47-year-old, married, unemployed, and homeless white British male, was remanded into prison after 3 days in police custody after being recalled and charged with possession of cannabis and theft. On admission, Mr A reported a history of polysubstance misuse: heroin, crack cocaine, buprenorphine, diazepam, and alcohol. He had a diagnosis of borderline personality disorder and fatty liver disease. Following assessment, he commenced on alcohol detox and OST. He was prescribed chlordiazepoxide, methadone, quetiapine, mirtazapine and thiamine. The following day, whilst on the Induction Wing, a substance wrapped in cling film was discovered in his cell. He reported this to be morphine and paracetamol that he was using to self-medicate for pain. The type of illicit drugs was never confirmed, and it was not known how he passed the X-ray scanner at Reception, though he confirmed that he concealed the drugs in his rectum. Mr A was taken to Reception for scanning and transferred to the CSU as the scan remained positive. He remained in the CSU for6 days. His methadone was stopped. Mr A was re-scanned and transferred back to the Induction Wing following a negative result, where he continued with his alcohol detoxification. Mr A was not started on OST as he did not present with opioid withdrawal symptoms. |
|
Case 2: Mr B |
|
Mr B, a 46-year-old, single, unemployed, homeless, white British male was recalled to prison following burglary. He had been in police custody for one day. On admission, Mr B reported use of heroin, crack cocaine, cannabis, and methadone. He had a diagnosis of personality disorder, depression, hypertension and psoriasis. It was noted on transfer paperwork from Police Custody that Mr B was captured on CCTV swallowing two packets of substances, but there was no recorded evidence of attempts to retrieve the swallowed package. When the nurse reviewed Mr B, he initially denied swallowing packages, but following a further interview he admitted having swallowed packages of illicit drugs. However, no package was detected through X-ray body scanner. Mr B declined a re-scan and a transfer to Accident and Emergency (A&E). Mr Bremained in the CSU for 3 days. On Day 3, he agreed to be taken to A&E, and once cleared, he was transferred to the Induction Wing, where he was reviewed by the addiction specialist GP. Mr B was started on OST with methadone. |
|
Case 3: Mr C |
|
Mr C, a 43-year-old white, homeless (sofa-surfing) man, was admitted on recall, having spent fewer than 3 hours in police custody. He was on mirtazapine, gabapentin and zopiclone, clenil modulate inhaler, and paracetamol. He had a history of asthma, anxiety, and depression. He told the police custody healthcare professional that he buys buprenorphine and methadone on the street and that he last took illicit methadone one day before. He asked for diazepam and dihydrocodeine. He refused physical examination, and declined intervention offered, threatening that he would continue to buy illicit drugs in prison.
He was known to the SMS, having been in and out prison for over 10 years. On arrival in prison, the Prison Custody Officer (PCO) reported that he had a positive body scan that identified him as having internally concealed a package in the rectum. On assessment, Mr C denied knowledge of the package and stated that he was constipated. He was asymptomatic. He denied thoughts of self-harm or suicide. He was located on the CSU. His urine was positive for opiates, cocaine, and cannabis. The GP recommended regular monitoring for signs of nausea, vomiting, abdominal pain, hypotension, and drowsiness as a low threshold for transfer to A&E.
On Day 2 he was reviewed by an addiction nurse. There were no symptoms of withdrawal, and he was alert and orientated. He again denied having ICIDs and demanded OST. When the risk was explained to him, he said he would swallow all the tablets (140 codeine tablets and 40 pregabalin capsules). The risks were explained to him, and a plan was put in place for him to be relocated to the In-Patient Unit (IPU) and to be transferred to A&E if he deteriorated.
On Day 4 during very early morning checks a nurse noticed a cling film wrapped package containing a white substance on the floor. The CSU PCO said that the package had been on the floor for over 2 hours and when the nurse called the prisoner, he did not respond. On opening the cell the prisoner complained of being woken up and refused to answer questions. A film-wrapped white substance, a brown substance, and white tablets were retrieved from his left hand. During the day he was rescanned, he remained positive, and he was transferred to the IPU. On arrival he said that he would continue to take illicit drugs as doctors had refused to prescribe dihydrocodeine and pregabalin. He admitted having dihydrocodeine packed in his rectum, stating he was using it to self-medicate for pain. He was seen by a GP in the IPU, and requested buprenorphine, zopiclone, and dihydrocodeine. He was reassured that once he was cleared, he would be started on OST. He was later rescanned but remained positive.
On Day 7, while still at the CSU, he told the nurse that he swallowed five capsules of pregabalin and five diazepam tablets, which he brought with him because he knew that he would not be given them in prison. He declined physical examinations. Later he was scanned and remained positive. During the night he told the nurse that he had snorted 2000mg of pregabalin. He had a small amount of powder on his hand. He said that he brought medication from outside and was taking it because he was withdrawing.
On Day 8, he was reviewed in the CSU by the addictions specialist GP who noted that the prisoner remained at high risk due to a possible intrarectal or abdominal blockage and use of illicit drugs in the CSU and IPU. He recommended close monitoring with transfer to A&E if indicated. OST was to be started only if objective evidence of no ICIDs and obvious opiate withdrawals. He was later rescanned and the PCO reported to the nurse that he was positive with what appeared to be a metal object, lighter, or pipe in the rectum. His cell was searched, and a powdered substance was found. He did not have withdrawal symptoms.
On Day 9, his scan was negative, and he was transferred to Induction Wing. The following day, during a clinical review, he reported that he last used pregabalin, codeine, and buprenorphine in prison a day ago. His urine tested positive for cocaine, opiates, cannabis and buprenorphine.
On Day 11, he was reviewed by an addiction specialist GP, and was started on OST with methadone. |
Table 2: Case presentations of prisoners suspected of ICIDs.
Findings: Highlights from the case studies
The three case studies highlight the risks and complexity presented by prisoners suspected of ICID and the changes required to optimize patient safety and clinical effectiveness of interventions.
Case 1 is of a prisoner suspected of concealing packages on Induction Wing. The prisoner had been started on both alcohol and OST with methadone. The package concealed in the prisoner’s rectum was missed by the X-ray body scanner at Reception. As crack cocaine was later found in his cell, it is possible that this led to drugs being introduced to the wing of the prison. As Mr A had been started on OST, this put him at a great risk of adverse outcomes including intoxication and overdose death. Due to risks, such cases often present the greatest challenge to SMS staff. Though Mr A was transferred to the CSU, where he remained for 6 days, monitoring by healthcare staff and PCOs was inadequate to minimize risk.
Case 2 is of a patient who was captured on CCTV swallowing packages in police custody prior to prison transfer. Despite this observation, and it being noted on his transfer records, documentation reveals no attempts had been made to retrieve the packages or arrange for referral to hospital. This case highlights limitations of the X-ray body scanner, the potential impact of a prisoner’s refusal to receive recommended care, and a lack of a joined-up approach to care with clear roles and responsibilities, particularly when patients decline treatment or transfer, combined with a lack of clinical monitoring.
Case 3 is principally documented to demonstrate the complex journey of a prisoner suspected of having ICIDs in the prison setting. The prisoner was particularly at risk of intoxication or overdose death due to continued use of illicit drugs while in the IPU and CSU.
The summary of the sixteen cases further highlights the various risks faced by prisoners who are suspected to have internally concealed illicit drugs. Although these prisoners did not experience adverse outcomes, several issues are highlighted. These include lack of custodial staff awareness on the risks of internal drug concealment and how it should be managed safely, lack of clinical monitoring for deterioration, provision of OST to prisoners who were later suspected of having ICIDs, and absence of a defined protocol to aid the clinical management of these prisoners. It is also obvious that better methods of screening prisoners are required and that reliance on body scanners is ineffective.
Discussion
We believe the current approach to the management of internal drug concealment has many risks. The audit highlights aspects of current practice that should change to ensure prisoners suspected of having ICIDs are adequately monitored by trained personnel, and the risk of adverse outcomes minimized through prompt escalation.
Guidance from His Majesty’s Prison and Probation Service (HMPPS) recognizes drug concealment as a potential medical emergency and indicates that healthcare staff should be contacted at the earliest opportunity and that clinical monitoring must be carried out in a location where immediate resuscitation equipment can be accessed and staff are trained to perform cardiopulmonary resuscitation [24]. Furthermore, where trained staff are not available, transfer to hospital should be immediate. In addition, basic observations including temperature, heart rate, respiratory rate, blood pressure, pupil size, and the Glasgow Coma Score, with the National Early Warning Score 2 (NEWS2 [36]) should be used to capture ongoing monitoring and should support clinical decision-making [24]. Although the guideline recommends that prison officers should use4R non-clinical monitoring (Rousability, Response to questions, Response to commands, Remember), we believe it would put lives at risk. In our opinion this monitoring should not be the responsibility of untrained custodial officers.
Our experience, as demonstrated in the case studies, shows that the recommendations in the HMPPS document are not being followed. Whilst working alongside PCOs, frequent themes regarding the management of prisoners suspected of concealing drugs have emerged such as:
- Poor communication between PCOs and the healthcare team
- Inadequate training on effective management of prisoners suspected of having ICIDs
- Lack of confidence among some PCOs in reading the results of newly introduced X-ray scanners
- Limited scope of X-ray scanners
- Lack of awareness among PCOs and prisoners of the dangers of drug concealment, the signs of acute overdose and the need for constant monitoring by trained personnel
- Lack of protocol (Figure S1 and HMPPS [37]) awareness, leading to prisoners being inappropriately segregated before discussion with the healthcare team
- Lack of a formal policy in the CSU for prisoners suspected of ICIDs
- Prisoners suspected of ICIDs being located to the CSU with little to no monitoring until they are free of the internal package
- No effort to ascertain whether the package has been safely evacuated and disposed of by the prisoner
- The prisoner remains at risk of overdose following consumption of illicit drugs whilst in the CSU
- There is a risk of evacuated illicit drugs finding their way into the larger prison estate
- Our recommendations
To mitigate the issues discussed above, we propose the process outlined in figure 1 for the management of suspected internal illicit drug concealers within the prison setting to safeguard health, well-being, and safety of prisoners. In this process, identifying those most at risk of adverse outcomes is key, and history taking is an important first step to differentiate body stuffers from body packers. Collaboration between healthcare staff and PCOs is needed to ensure appropriate monitoring is received, and escalation is timely when needed.
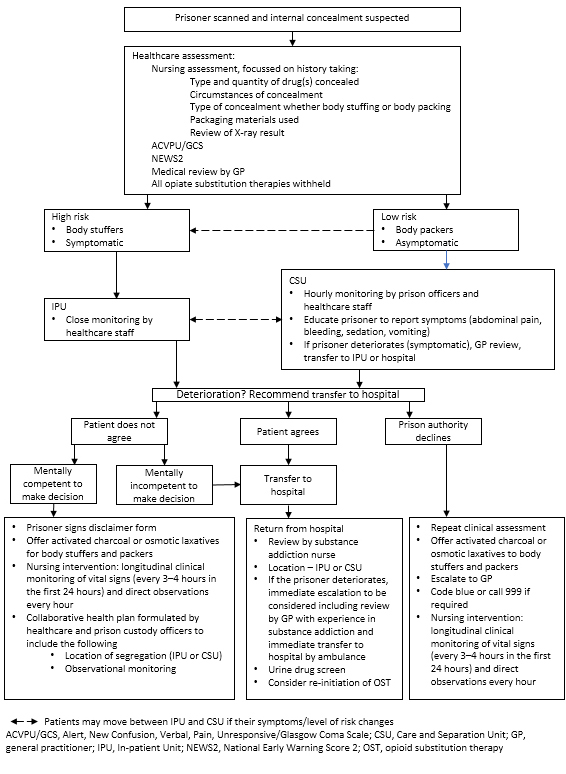 Figure 1: Healthcare management flowchart for suspected drug concealers within prison settings.
Figure 1: Healthcare management flowchart for suspected drug concealers within prison settings.
There are various outcomes arising from the concealment of drugs in a prison setting, ranging from complete evacuation and disposal of drugs, through to intoxication and even death due to internal leakage. The identification of prisoners suspected of carrying concealed packages is a key first step when optimizing care for internal drug traffickers. Though X-ray scanners are becoming commonplace in prisons, they can show false positives, particularly when the individual is constipated [38]. In addition, prisoners are good at creatively developing systems that circumvent security measures, especially when the likelihood of getting caught is low and the rewards are high [39]. Fundamentally, even when concealed packages are detected through scanners, the prisoner remains at risk of death unless an adequate management plan is in place.
The initial assessment is key in quantifying the risk to the prisoner. This should encompass checking for signs and symptoms of drug intoxication, sedation, or overdose, and a physical examination to identify gastrointestinal obstruction, respiratory depression, and the location of concealed packages [9,12,40-42]. Although narratives can be unreliable due to varying factors, a thorough patient history should be taken. This should cover the type of drug, time of ingestion (concealment), formulation, number of packets ingested, packaging material, whether other substances to help expel the packets have been ingested, gastrointestinal symptoms (pain, bloating, vomiting, obstipation and constipation), and whether drugs were for personal use [11,33,43,44]. Discussions must be carried out with caution and tact, and according to the principles of clinician–patient confidentiality [21].
We propose that every prison should have a suite located in the IPU for the management of prisoners suspected of internal drug concealment. This suite should be equipped with resuscitation equipment, including naloxone, and manned by healthcare staff trained in their use. It is also important that the prisoner is assessed for risk factors for adverse outcomes by a trained healthcare professional. After the assessment is complete, those deemed high risk should be monitored closely by healthcare staff in the IPU and the Alert, New Confusion, Verbal, Pain, Unresponsive/Glasgow Coma Scale (ACVPU/GCS) and NEWS2 should be used to identify those most at risk of adverse outcomes necessitating immediate transfer to hospital. Those deemed low risk can be monitored in the CSU and educated to inform staff of any signs of deterioration. Transfer to the IPU or hospital may be necessary as per escalation triggers influenced by ACVPU/NEWS2 and healthcare professionals’ clinical opinion.
A distinction should be made between body stuffers and body packers and pushers; the former are at greater risk of packages leaking and may require immediate intervention, while the latter are more likely to know the number and contents of the packages concealed [11,33]. Body stuffers (mostly swallowers) are at greater risk of perforation or blockage of the gastrointestinal tract and, if the X-ray scanner shows that the package is in the upper abdomen, the prisoner should be rated as high risk and transferred to the IPU. However, a low-dose Computed Tomography (CT) scan of the abdomen and pelvis is the investigation of choice in suspected internal drug traffickers [45] as it enables accurate and reliable detection of different densities. Such scans can assist with determining the location, density, number, and progression of packets, all of which aid clinical management [46,47]; however, they can only be performed at the hospital.
The Independent Report of the Chief Medical Officer’s Expert Group for the medical care of suspected internal drug traffickers calls for all suspected drug concealers to be transferred to hospital [6]. It also recommends the development of a defined clinical pathway and standardized protocol for managing concealers in custody, to be used together with an early Warning System (NEWS2) for use in the custodial environment - a Custodial Early Warning System (CEWS). However, in our experience, transferring all prisoners suspected of internal drug concealment to hospital is not always feasible due to a lack of PCOs for escort. We believe those who are not at high risk of adverse events can be managed effectively within the prison by fully trained healthcare staff. We do, however, concur with the recommendation that suspected internal drug concealers should only be managed in prison if the following can be provided [6]:
- 24-hour observations, with CEWS scoring
- Rapid access to A&E
- Suitably trained healthcare staff and PCOs
- Emergency resuscitation equipment
In addition, educating the prisoner on the risk of adverse outcomes is extremely important, especially when they are asymptomatic or declining hospital transfer. When hospital transfer is declined by the prison authority or the prisoner, it may be necessary to escalate and request a second opinion via GP or obtain paramedic review. If they too deem the prisoner to be in no immediate danger, close monitoring of the patient in the CSU is appropriate.
Prisoners who deteriorate and have mental capacity to decline hospital transfer should sign a disclaimer form and be cared for in the IPU. Activated charcoal or osmotic laxatives should be offered to body stuffers or packers to aid passing of packages, and a collaborative plan should be formulated between healthcare and custodial staff to ensure vital signs are checked every 3-4 hours, and direct observations made every hour. The NEWS2, which includes temperature, respiratory rate, blood pressure, pulse, and consciousness [36] should be used as a tool to signal deterioration. Prisoners who have been transferred to hospital are likely to be returned to prison once their condition has stabilized, even though they might not have passed/evacuated the packages. Upon return to prison, careful assessment should be made to determine whether the IPU or CSU would provide the most appropriate level of care.
Conclusion
The risk of overdose death remains high among prisoners with substance use disorders who have access to illicit drugs in prison. Most of these prisoners have co-occurring mental disorders with concomitant psychotropic medications that enhance the risk of overdose death. The SMS clinical team have remained vigilant to these risks, but also acknowledged that the same is ever present, and as demonstrated by the case of Mr Forrester, prisoners are at heightened risk on entry into prison due to illicit drugs they carry with them. SMS staff are aware that it is common practice for prisoners to conceal drugs to smuggle into prison if they are recalled for breaking bail conditions or missing a probation appointment.
Our audit and the case studies highlight the current deficits in care provided to prisoners suspected of internally concealing drugs in the prison environment. These include lack of awareness of the risks of internal drug concealment among custodial staff, lack of monitoring by trained clinical staff, and inadequate communication between PCOs and healthcare staff within the prison, which led to one of our case-study patients being prescribed maintenance therapy when it was known to custodial officers that he was suspected of internally concealing drugs. Inadequacies such as these greatly increase the risk of adverse outcomes.
The management of drug concealers in the prison setting requires joint working between custodial officers and healthcare personnel, together with the prisoner. If the prisoner refuses or is unable to evacuate the suspected item, the prison must consider the risks presented by that prisoner to themselves and/or others. In all cases, the prison must consider the location and observation requirements of the prisoner. This could include use of the CSU, IPU, or sending the prisoner to the local hospital. This decision should always be made in conjunction with healthcare professionals [24]. Our case studies illustrate instances where optimal care has not been achieved, largely due to a lack of clear guidance and management processes, or prisoner refusal, both of which increase the risk of adverse outcomes including death.
To ensure optimal outcomes, we call for healthcare staff and each prison authority to jointly create screening and management protocols for prisoners who are suspected of concealing drugs upon prison entry. The protocol proposed here is our contribution towards this effort. The emphasis of such protocols should be to ensure that patient safety always comes first [3,44] and, as such, must incorporate appropriate observations by trained staff in an appropriately equipped setting. To achieve this, the importance of multi-disciplinary working within the unique prison environment cannot be overstated.
Acknowledgement
The authors thank Meredith Jones, PhD (Alchemie Medical Education) for medical writing support, funded through the Opi Assist programme (https://www.opi-assist.com/).We thank Dominic Emebo for his support with data retrieval and Dr Yomi Salami for his advice on the management plan.
Competing Interests
None.
Funding
Medical writing support was funded through the Opi-Assist programme (https://www.opi-assist.com/). Opi-Assist is funded through a donation from Camurus. Camurus has no influence on the selection of the steering committee or the selection of applications awarded medical writing support by the Opi-Assist programme.
Authors’ contributions
CRediT authorship contribution statement: John Arianda Owiti: conceptualization, writing - original draft, review and editing. Molli Benson: conceptualization, data collection, writing - contributions to original draft, review and editing. Lasekan Oluseye: writing - contributions to original draft, review and editing.
References
- Babor T, Caulkins J, Fischer B, Foxcroft D, Humphreys K, et al. (2010) Drug Policy and the Public Good (2ndedn). Oxford University Press, Oxford, UK.
- Deitel M, Syed AK (1973) Intestinal obstruction by an unusual foreign body. Can Med Assoc J 109: 211-212.
- Havis S, Best D, Carter J (2005) Concealment of drugs by police detainees: lessons learned from adverse incidents and from 'routine' clinical practice. J Clin Forensic Med 12: 237-241.
- INQUEST (2020) Deaths in prison: A national scandal. INQUEST, London, UK.
- Office for National Statistics (2016) Deaths related to drug poisoning in England and Wales: 2016 registrations. Office for National Statistics, Cardiff Road, UK.
- Independent Report of the Chief Medical Officer’s Expert Group (2013) The medical care of suspected internal drug traffickers - Independent report of the Chief Medical Officer’s Expert Group.
- Duke K, Gleeson H, MacGregor S, Thom B (2023) The risk matrix: Drug-related deaths in prisons in England and Wales, 2015-2020. J Community Psychol.
- Heymann-Maier L, Trueb L, Schmidt S, Carron PN, Hugli O, et al. (2017) Emergency department management of body packers and body stuffers. Swiss Med Wkly 147: 14499.
- Hassanian-Moghaddam H, Amraei F, Zamani N (2019) Management recommendations for body stuffers at emergency units. Arh Hig Rada Toksikol 70: 90-96.
- Coroner (2023) Regulation 28 Reports to Prevention of Future Deaths. Coroner.
- Traub SJ, Hoffman RS, Nelson LS (2003) Body packing--the internal concealment of illicit drugs. N Engl J Med 349: 2519-2526.
- Booker RJ, Smith JE, Rodger MP (2009) Packers, pushers and stuffers--managing patients with concealed drugs in UK emergency departments: A clinical and medicolegal review. Emerg Med J 26: 316-320.
- Roberts JR, Price D, Goldfrank L, Hartnett L (1986) The bodystuffer syndrome: A clandestine form of drug overdose. Am J Emerg Med 4: 24-27.
- Bahrami-Motlagh H, Hassanian-Moghaddam H, Behnam B, Arab-Ahmadi M (2015) Failure of surgical treatment in methamphetamine body-stuffers. J Forensic Leg Med 32: 70-72.
- Bulakci M, Cengel F (2016) The role of radiology in diagnosis and management of drug mules: An update with new challenges and new diagnostic tools. Br J Radiol 89: 20150888.
- Sporer KA, Firestone J (1997) Clinical course of crack cocaine body stuffers. Ann Emerg Med 29: 596-601.
- Erfantalab P, Zamani N, Hashemi-Domeneh B, Hassanian-Moghaddam H, Akhgri M (2016) Abdominal computed tomography of a fatal amphetamine poisoning; pitfalls of diagnosis and treatment. Zahedan Journal of Research in Medical Sciences 18: 2853.
- Schaper A, Hofmann R, Bargain P, Desel H, Ebbecke M, et al. (2007) Surgical treatment in cocaine body packers and body pushers. Int J Colorectal Dis 22 : 1531-1535.
- Fineschi V, Centini F, Monciotti F, Turillazzi E (2002) The cocaine "body stuffer" syndrome: A fatal case. Forensic Sci Int 126: 7-10.
- June R, Aks SE, Keys N, Wahl M (2000) Medical outcome of cocaine bodystuffers. J Emerg Med 18: 221-224.
- Püschel K, Stein S, Stobbe S, Heinemann A (2004) Analysis of 683 drug packages seized from "body stuffers". Forensic Sci Int 140: 109-111.
- Schmidt U, Seibt J, Flössel U, Pietsch J, Erfurt C, et al. (2018) Tödliche Methamphetaminvergiftungen durch Bodystuffing. Rechtsmedizin 28: 398-404.
- George S, Clayton S, Namboodiri V, Boulay S (2009) "Up yours": smuggling illicit drugs into prison. BMJ Case Rep 2009: bcr0620091935.
- HM Prison & Probation Service (2021) Interim Guidance on managing people suspected of concealing illicit items internally in the secure environment (SECURITY). HM Prison & Probation Service.
- Wetli CV, Mittlemann RE (1981) The "body packer syndrome"-toxicity following ingestion of illicit drugs packaged for transportation. J Forensic Sci 26: 492-500.
- Beerman R, Nunez D Jr, Wetli CV (1986) Radiographic evaluation of the cocaine smuggler. Gastrointest Radiol 11: 351-354.
- Utecht MJ, Stone AF, McCarron MM (1993) Heroin body packers. J Emerg Med 11: 33-40.
- Horrocks AW (1992) Abdominal radiography in suspected ‘body packers’. Clin Radiol 45: 322-325.
- Krishnan A, Brown R (1999) Plain abdominal radiography in the diagnosis of the "body packer". J Accid Emerg Med 16: 381.
- Wilcher G (2011) Drug-related deaths with evidence of intracorporeal drug concealment at autopsy: Five case reports. Am J Forensic Med Pathol 32: 314-318.
- Tompkins CNE (2016) “There's that many people selling it”: Exploring the nature, organisation and maintenance of prison drug markets in England. Drugs: Education, Prevention and Policy 23: 144-153.
- Watson TM (2016) The elusive goal of drug-free prisons. Subst Use Misuse 51: 91-103.
- Hoffman RS, Nelson L (2015) Internal concealment of drugs of abuse (body packing). Up To Date, Massachusetts, USA.
- Guimarães VHA, Cassiano C, Queiroz DIB, Pastore R, Lenza R, et al. (2022) Clinical, diagnostic, and treatment features of body packing in Brazil: Drugs, cell phones, and beyond. Cureus 14: 27894.
- World Health Organization (2021). International Statistical Classification of Diseases and Related Health Problems (ICD). World Health Organization, Geneva, Switzerland.
- Royal College of Physicians (2017). National Early Warning Score (NEWS) 2 Standardising the assessment of acute-illness severity in the NHS. Royal College of Physicians, London, England, UK.
- HM Prison & Probation Service (2022) Renewing and authorising continuing segregation and temporary confinement in special accommodation. Amendment to policy set out on PSO 1700. HM Prison & Probation Service, London, UK.
- Karhunen PJ, Suoranta H, Penttilä A, Pitkäranta P (1991) Pitfalls in the diagnosis of drug smuggler’s abdomen. J Forensic Sci 36: 397-402.
- The Centre for Social Justice (2015) Drugs in Prison. The Centre for Social Justice, UK.
- de Beer SA, Spiessens G, Mol W, Fa-Si-Oen PR (2008) Surgery for body packing in the Caribbean: A retrospective study of 70 patients. World J Surg 32: 281-285.
- Silverberg D, Menes T, Kim U (2006) Surgery for "body packers"--a 15-year experience. World J Surg 30: 541-546.
- Heinemann A, Miyaishi S, Iwersen S, Schmoldt A, Püschel K (1998) Body-packing as cause of unexpected sudden death. Forensic Sci Int 92: 1-10.
- Jimenez N, Tran NT, Poletti PA, Platon A, Meach F, et al. (2019) Case report: don't chew the fufu: A case report of suspected drug body stuffing. F1000Res 8: 1156.
- Puntonet J, Gorgiard C, Soussy N, Soyer P, Dion E (2021) Body packing, body stuffing and body pushing: Characteristics and pitfalls on low-dose CT. Clin Imaging 79: 244-250.
- Royal College of Emergency Medicine (2020) Management of suspected internal drug trafficker (SIDT). Royal College of Emergency Medicine, London, England, UK.
- Flach PM, Ross SG, Ampanozi G, Ebert L, Germerott T, et al. (2012) "Drug mules" as a radiological challenge: sensitivity and specificity in identifying internal cocaine in body packers, body pushers and body stuffers by computed tomography, plain radiography and Lodox. Eur J Radiol 81: 2518-2526.
- Jalbert B, Tran NT, von Düring S, Poletti PA, Fournier I, et al. (2018) Apple, condom, and cocaine - body stuffing in prison: A case report. J Med Case Rep 12: 35.
Appendix
Appendix 1: Case studies - Cases of suspected internal concealment of illicit drugs.
|
Case |
Age |
Ethnicity |
Marital status |
Housing status |
Education |
Employment |
Substances of abuse |
Community engagement with treatment |
Injecting status |
Urine drug screen on admission |
Mental health diagnosis |
Physical health diagnosis |
Admission route |
Days in police custody |
Sentence status |
Location of concealment notification |
Resolution |
Treatment decision after CSU |
Reason provided |
|
|
|
1 |
46 |
White British |
Single |
NFA |
None |
No |
Heroin Crack cocaine Cannabis |
No |
Never |
MTD OPI COC THC |
Personality disorder, unspecified Depression |
Hypertension Psoriasis |
Police custody + court |
2 |
Recall |
Reception, medical records indicated that he had swallowed a package in police custody, declined A&E transfer, located in CSU |
2 days in CSU; rescanned, prison confirmed no foreign body |
Review by AS-GP and OST titration started |
Denied (but seen on CCTV whilst in police custody swallowing 2 wraps) |
|
|
|
2 |
41 |
Bangladeshi |
Single |
NFA |
GCSE |
No |
Heroin Crack cocaine Diazepam |
No |
Current |
OPI COC BZO |
Anxiety Depression |
No |
Police custody + court |
1 |
Remand and recall |
Induction Wing |
2 hours in CSU, nil X-ray, heroin found in cell |
Warning and continuation of OST, prolonged monitoring |
Help him whilst in police custody |
|
|
|
3 |
29 |
Bangladeshi |
Single |
NFA |
None |
No |
Heroin Crack cocaine |
No |
Never |
OPI COC |
No |
No |
Police custody |
2 |
Remand |
Induction Wing, on MTD titration |
6 days in CSU; reported he passed out the package, rescanned and cleared |
Promethazine 7 days, nil opiate withdrawal, discharged from SMS |
Swallowed crack cocaine on approach by police to avoid drug possession charge |
|
|
|
4 |
31 |
White British |
Single |
NFA |
NVQ-2 |
No |
Heroin Crack cocaine Alcohol |
No |
Never |
OPI COC |
Post-traumatic stress disorder Anxiety Depression |
Asthma Psoriasis |
Police custody |
2 |
Convicted |
Induction Wing, was on MTD |
6 days in CSU; disposed of phone and drugs in reception, rescan, cleared |
Review by AS-GP and OST titration restarted |
Denied concealing illicit drugs |
|
|
|
5 |
49 |
White British |
Married |
Renting |
None |
No |
Heroin Crack cocaine |
Yes MTD (70mL/mg daily) |
Never |
MTD OPI COC |
No |
Asthma Chronic obstructive pulmonary disease |
Police custody + court |
2 |
Convicted |
Reception, no OST. |
14 days in CSU; consumed drugs, rescan and cleared |
Review by AS-GP and OST initiated |
Reported phone and heroin plugged in rectum, for personal use. He got rid of drugs in Reception and phone in CSU. |
||
|
6 |
38 |
White British |
Single |
NFA |
None |
No |
Heroin Crack cocaine Diazepam Cannabis |
No |
Never |
OPI COC BZO THC |
Personality disorder, unspecified Depression |
Sexually transmitted disease |
Police custody + court |
1 |
Remand |
Reception |
3 hours in CSU; rescan and cleared |
AS-GP review and methadone titration |
Denied internal concealment of illicit drugs |
|
|
|
7 |
46 |
Indian |
Single |
Homeowner |
NVQ -3 |
Manual labour |
Heroin Crack cocaine Diazepam |
No |
Previous |
BUP OPI COC BZO |
No |
No |
Police custody + court |
1 |
Remand |
Reception, prescribed diazepam and MTD, but not administered |
4 days in CSU; consumed substance (heroin, BUP, clonazepamand diazepam) handed over tobacco. Rescanned and cleared |
Review by AS-GP; MTD and diazepam started |
Wrapped heroin, crack cocaine, diazepam, and tobacco. Help him whilst in police custody, prevent withdrawal symptoms |
|
|
|
8 |
47 |
Bangladeshi |
Single |
NFA |
None |
No |
Heroin Crack cocaine |
Yes, MTD |
Never |
MTD OPI COC |
Paranoid schizophrenia Personality disorder, unspecified |
Type 1 diabetes mellitus |
Police custody + court |
4 |
Remand |
Induction Wing, 3rd day, was on MTD and alcohol detox. Suspected of plugging unknown substance in his rectum. |
14 days in CSU; brought to Induction Wing, passed substance, rescanned, and cleared |
Review by AS-GP and MTD titration restarted |
Swallowed small quantity of heroin and crack cocaine package on arrest to avoid charge. He said that he passed some substances on the Induction Wing before he was taken to CSU |
|
|
|
9 |
39 |
White British |
Single |
NFA |
None |
No |
Heroin Crack cocaine Alcohol |
No |
Never |
BUP COC BZO THC |
No |
No |
Police custody + court |
Unknown |
Convicted |
Induction Wing, started on alcohol detox and MTD. Information from PCO on 3rd day that he is suspected of having internal concealment of package following a scan on arrival. To be rescanned. Medication stopped. |
29 days in CSU; reviewed by AS-GP, no treatment indicated following discharge from CSU |
Methadone and chlordiazepoxide stopped, symptomatic treatment given. Transferred to another prison from CSU |
Denied, but has a known history of drug concealment |
|
|
|
10 |
44 |
Black African |
Single |
NFA |
None |
No |
Heroin Alcohol Cannabis |
No |
Previous |
OPI BZO THC |
No |
Tuberculosis
|
Court |
N/A |
Recall |
Reception, alcohol detox |
2 days in CSU; rescan, cleared |
Review by AS-GP, alcohol treatment only |
Denied (but witnessed inserting package with drugs in rectum in Kinder Egg capsules) |
|
|
|
11 |
34 |
White British |
Single |
NFA |
None |
No |
Heroin Crack cocaine Cannabis |
No |
Never |
OPI COC THC |
No |
Tuberculosis |
Court |
N/A |
Remand |
Induction Wing, OST stopped 2nd day |
13 days in CSU; rescan, cleared |
Continuation of OST |
Only admitted to concealing and selling quetiapine |
|
|
|
12 |
31 |
White British |
Single |
NFA |
None |
No |
Heroin Crack cocaine Diazepam |
No |
Never |
MTD OPI COC BZO THC |
Paranoid schizophrenia |
Hodgkin lymphoma |
Court |
N/A |
Remand |
Reception, suspected to have a crack pipe and unknown substance in rectum, OST and BZO detox not started |
Declined rectal exam by GP. Declined A&E transfer. No bed in IPU. Handed over crack pipe, rescanned &cleared. Located on Induction Wing. |
Reviewed on the Induction Wing the following day, by AS-GP; OST and benzo detox started |
Denied internal concealment of illicit drugs but admitted to having crack pipe. Said he had little drugs but consumed in police custody |
|
|
|
13 |
47 |
White British |
Married |
NFA |
Entry Level 3 |
No |
Alcohol |
No |
Never |
Not given |
Borderline personality disorder Depression |
Fatty liver disease |
Police custody + court |
3 |
Convicted |
Induction Wing, had been in prison for 6 days |
6 days in CSU; Reception scan positive; later X-ray re-scanned negative &cleared |
Not for detox, referred to Mental health |
Admitted inserting package (paracetamol, and morphine) in rectum for pain management |
|
|
|
14 |
39 |
Bangladeshi |
Single |
Living with parent |
City and Guilds level 2and B-Tech Diploma |
No |
BUP Crack cocaine Cannabis |
No |
Previous |
BUP COC THC |
Depression |
Type 2 diabetes mellitus Chronic pancreatitis |
Police custody + court |
1 |
Remand |
Reception; started on BUP. Taken to the Induction Wing, then later brought back to Reception, suspected of having swallowed a package that was hidden in his shoes. Scan confirmed package in mid oesophageal region. Medications stopped. Low threshold or A&E transfer. |
10 days in CSU; Rescanned and cleared |
Review by AS-GP; alcohol treatment/benzo detoxand OST initiation |
For personal use, during first few days of active withdrawals |
|
|
|
15 |
44 |
White |
Single |
NFA |
City and guilds |
No |
Crack cocaine Heroin Cannabis |
No |
Previous |
COC |
Paranoid schizophrenia, EUPD |
No |
Police custody + Court |
1 |
Remand |
Induction Wing, was on OST, 3rd day |
7 days in CSU |
Review by AS-GP and re-restarted on OST |
Reported that he brought drugs pregabalin and codeine for pain |
|
|
|
16 |
43 |
White |
Single |
NFA |
City and Guilds |
No |
Crackcocaine Cannabis MTD and BUP |
No |
Previous |
COC |
Depression Anxiety |
Asthma |
Police custody |
1 |
Remand |
Reception had a positive X-ray body scan. |
7 days between IPU and CSU. |
Once cleared, reviewed by AS-GP, and started on OST, methadone |
Reported that he brought drugs pregabalin and codeine for pain |
|
|
|
Abbreviations A&E, Accident and Emergency; AS-GP, addiction specialist general practitioner; BUP, buprenorphine; BZO, benzodiazepine; CCTV, closed-circuit television; COC, cocaine; CSU, Care and Separation Unit; EUPD, Emotionally Unstable Personality Disorder; GCSE, General Certificate of Secondary Education; MTD, methadone; N/A, not applicable; NFA, no fixed abode/homeless; NVQ, National Vocational Qualification; OPI, opiate; OST, opioid substitution treatment; PCO, Prison Custody Officer; SMS, Substance Misuse Service; THC, tetrahydrocannabinol |
Appendix 2: A report by the Prisons and Probation Ombudsman [1]: An independent investigation into the death of Mr Nathan Forrester, a prisoner at HMP Thameside, on 2 July 2019.
Mr Forrester was recalled to prison. He had a history of substance misuse and appeared to be drowsy and withdrawing from drugs when he arrived. The escort documents indicated that Mr Forrester had previously concealed illicit drugs, so the reception manager instructed staff to carry out a full search and pay close attention when searching him. A nurse conducted an initial health screen. A urine test was positive for opiates, benzodiazepines, cocaine, cannabis, and methadone. A GP then assessed Mr Forester but decided not to prescribe methadone that evening as his pulse rate was low. After the reception procedures, Mr Forrester was allocated to a shared cell on the drug stabilisation wing. Mr Forrester’s cellmate said that he had brought drugs - “three whites and one brown” (slang for cocaine and heroin) - along with his own tin foil to the cell and used some that night. The next day, Mr Forrester had several health assessments, and his vital signs observations were taken. He received a dose of methadone, 10mg/mL, just before 11.45am and was then locked in his cell. He and his cellmate both fell asleep during the lunch period. When his cellmate woke up, he noticed that Mr Forrester did not appear to be breathing and his arm was blue. He shouted and banged on his cell door to attract the attention of staff. Wing officers attended and radioed a medical emergency code at 3.10pm. An ambulance was requested, and healthcare staff attempted resuscitation until the paramedics arrived. Mr Forrester did not regain consciousness and the paramedics confirmed his death at 4.01pm. The report of the post-mortem examination concluded that Mr Forrester died from acute toxic effects of heroin, cocaine, and methadone. The pathologist could not determine when or how Mr Forrester had taken the illicit substances, or the quantities involved. He found that the concentration of methadone in Mr Forrester’s blood sample was consistent with therapeutic levels.
Reference
Citation: Owiti JA, Benson M, Oluseye L (2023) The Management of Adult Male Prisoners with Substance Use Disorders Presenting with Suspected Internal Concealment of Illicit Drugs: Challenges, Clinical Implications, and Best Practice Response. J Addict Addictv Disord 10: 147.
Copyright: © 2023 John Arianda Owiti, PhD, RMN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

