
The Power of Annual Cost-of-Illness in Predicting COPD Survival at 3 Years
*Corresponding Author(s):
Negro RWDNational Centre For Respiratory Pharmacoeconomics And Pharmacoepidemiology, Verona, Italy
Tel:+39 3483168888,
Email:robertodalnegro@gmail.com
Abstract
Clinical signs and lung function are variably sensitive in predicting survival in COPD.
Aim: To assess the power of annual COPD cost-of-illness in predictive mortality at three years.
Methods: Gender, age, complete lung function and clinical data of 275 COPD patients aged >40 years were assessed in baseline (T0), while the annual cost was calculated over the preceding twelve months.
Statistics: t tests to compare means±SD; regression analysis to determine the relationship between all variables and the survival (in days) (p<0.05).
Results: Mortality was 40.4% over the three years (12; 47 and 52 subjects deceased yearly, respectively). Independently of gender, the profile of survivors (n=164) was significantly different from that (n=111) of subjects who will decease by mean age, FEV1 (in L), RV, DLco, 6’ walking test and Charlson Comorbidity index (all p<0.001), but not by FEV1% pred. or FEV1/FVC% (all p=ns). At T0, mean total cost was €1,161.0 [95% CI: 968.4; 1,353.6] in survivors and €6,158.9 [95% CI: 5,508.0; 6,809.8] in those patients who will decease over the following three years (p<0.001). The hospitalization cost accounted for 78.2% of total annual cost in subjects who will decrease and the absolute value was 6-fold higher than that of survivors. Regression between cost and survival showed the highest power and significance (r=0.58; p<0.0001).
Conclusion: 1) Specific and appropriate lung function indices contribute to predicting mortality in COPD effectively. 2) Total annual cost confirms the most sensitive predictor of mortality at three years. 3) Present data support the high predictive power of the careful functional and economic phenotyping in COPD.
Keywords
Annual cost; COPD; COPD phenotypes; Mortality; Predictive value
ABBREVIATIONS
FEV1: Forced Expiratory Volume in 1 second
FEV1/FVC: Forced Expiratory Volume in 1 second/Forced Vital Capacity
RV: Residual Volume
DLco: Lung Diffusion Capacity for CO
BMI: Body Mass Index
INTRODUCTION
Chronic Obstructive Pulmonary Disease (COPD) is a complex and progressive condition which is characterized by a dramatic, ever increasing socio-economic impact [1-4]. Identifying the mortality risk in COPD patients still represents a crucial issue in the strategic management of this condition and the assessment of accurate predictors would support more effective interventions aimed at improving outcomes.
Actually, the sensitivity of clinical signs and of usual parameters of lung function (mostly, FEV1 and FEV1/FVC) in predicting death still is variable, even if they prove able to better define COPD long-term outcomes when integrated into multidimensional scores [5-13].
The role of the annual economic impact was absolutely neglected from this point of view and only in one study the annual cost was included in a composite score [14].
Aim of the present study was to assess the power of COPD annual cost-of-illness in predictive survival at three years. The relationships existing between all the parameters collected and survival were also investigated.
MATERIALS AND METHODS
The patients’ sample was automatically extracted from the Institutional Data Base. Criteria for selection were:
- • Subjects of both genders aged ≥ 40 years;
- • Diagnosis of COPD;
- • Yearly availability of at least one complete electronic clinical record for four consecutive years, such as: During the twelve months preceding the visit T0 and also for the three following years;
The variables to collect at T0 were: Age; gender; BMI; smoking habit; clinical data (namely: BODE Index; MRC Dyspnea score; Charlson Comorbidity Index; n. hospitalizations and their duration; n. exacerbations requiring antibiotic and/or systemic steroids assumption; complete lung function (namely: FEV1 in L and in % predicted; FEV1/FVC %; RV % predicted; DLco % predicted; FEV1 short-term reversibility after salbutamol 400mcg; 6’ walking test (in metres) and the annual cost calculated over the previous twelve months.
All-cause mortality and the length of survival were assessed by careful review of the death certificate delivered by the registry office of the Institution.
STATISTICS
Parametrical, non-parametrical tests and anova were used for comparing means±SD; 95% CI was also calculated. Linear regression was used in order to assess the total annual cost calculated at T0 and the length of survival over the following three years. The power of each variable considered at T0 in predicting mortality at three years (such as: Patients who will survive and patient who will decease during the study period) was also calculated and represented by web diagrams including the means value for each variable together to the corresponding statistical significance. The lower accepted limit of significance was p<0.05.
Selected subjects were included only after their informed consent to the study, which was approved by the Institutional Human Review Board of the Institution.
The present study was a spontaneous research, without any founding. Authors declare no conflict of interest.
RESULTS
The total sample consisted of 275 COPD patients who satisfied the selection criteria over the period 2008-2012. General characteristics of the whole sample are reported in table 1.
|
Age (y) |
70.9±8.4 |
|
BMI |
26.8±4.6 |
|
Smoking habit Active Ex Ever smoker |
65 (23.6%) 184 (66.9%) 26 (9.5%) |
|
FEV1 (L) |
1.5±0.5 |
|
FEV1% pred. |
55.9±18.8 |
|
FEV1/FVC % |
55.9±10.3 |
|
RV % pred. |
156.9±46.2 |
|
DLco % pred. |
70.9±26.2 |
|
FEV1 % reversibility |
6.7±7.9 |
|
6' walking test (mt) |
233.3±92.7 |
|
MRC dyspnea score |
2.3±1.2 |
|
BODE index |
4.4±2.6 |
|
Charlson Comorb. Index |
3.3±1.8 |
Table 1: Means±SD calculated for each variable at T0 in the whole sample (n=275).
The overall mortality rate was 40.4% over three years (n=111; n=12, 47 and 52 subjects deceased yearly). The three-year survival ranged 1024-755 days in patients deceased, respectively.
At T0, the lung function profile of subjects still surviving after three years (n=164) proved significantly different from that of patients who will decease in the same period. The two clusters of patients were different in terms of mean age; FEV1(L); RV% predicted; DLco % predicted; 6’ walking test; and Charlson comorbidity index (all p<0.001), but not in terms of FEV1% predicted and FEV1/FVC% (all p=ns) (Figure 1). In particular, patients who will die showed a more relevant emphysema component and were characterized by the highest annual cost, despite their shorter survival.
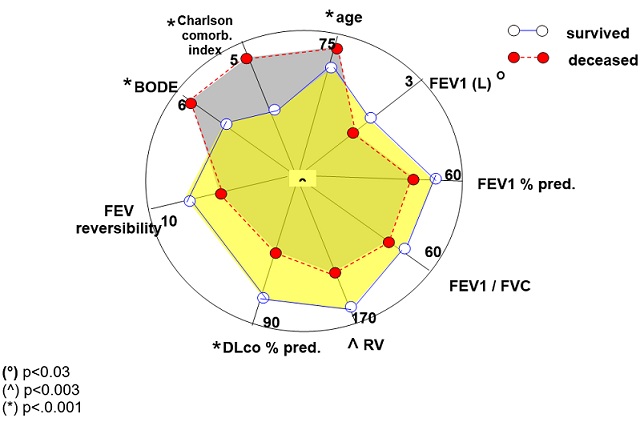 Figure 1: The web diagram summarizing the power of each lung function variables assessed at T0 in discriminating patients who will survive from those who will decrease over the three following years of the survey. Values reported correspond to the mean value calculated for each variable.
Figure 1: The web diagram summarizing the power of each lung function variables assessed at T0 in discriminating patients who will survive from those who will decrease over the three following years of the survey. Values reported correspond to the mean value calculated for each variable.
All economic components of cost were highly discriminant, independently of gender (Figure 2). Mean total COPD cost was 3,290.7 [95% CI: 2539.9; 4051.2], while it was € 1,161.0 [95% CI: 968.4; 1,353.6] in survivors and 6,158.9 [95% CI: 5,508.0; 6,809.8] in those who will die over the same period, respectively (p<0.001). The hospitalization cost impacted for 78.2% of the total annual cost in the latter subjects and their absolute cost proved 6-fold higher than that of survivors. Moreover, total annual cost showed the highest regression with survival (r = -0.63).
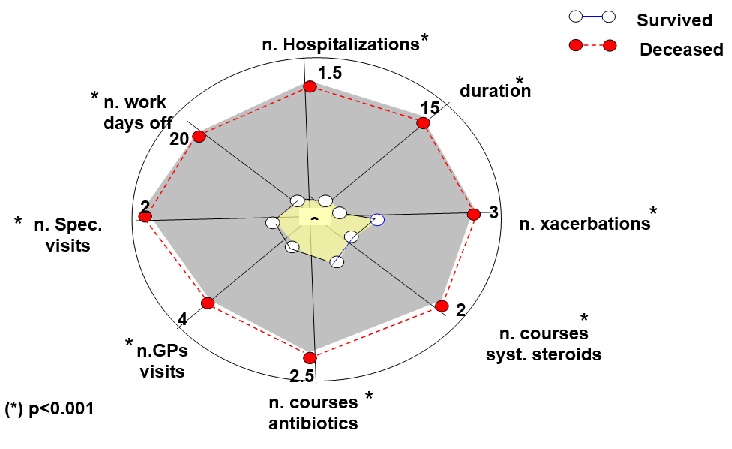 Figure 2: The web diagram summarizing the power of each determinant of the annual cost assessed over the twelve months before T0 in discriminating patients who will survive from those who will decrease over the three following years of the survey. Values reported correspond to the mean value calculated for each variable.
Figure 2: The web diagram summarizing the power of each determinant of the annual cost assessed over the twelve months before T0 in discriminating patients who will survive from those who will decrease over the three following years of the survey. Values reported correspond to the mean value calculated for each variable.
DISCUSSION
The mortality risk in COPD patients had been investigated in several studies in the last decades by means of a single parameter [15-19], by complex and composite clinical assessments [5-13] and by the recent multidimensional scores [20-23].
The different approaches to the prediction of COPD survival progressively improved the overall accuracy. Nevertheless, a wide variability still persists, mainly due to the variables originally chosen for the studies and frequently affected by the primary aim of these studies (i.e. pharmacological, epidemiological, etc).
FEV1 represented the simplest and then the first and the best accepted variable used to predict COPD mortality since long ago, even if it cannot reflect exhaustively the huge complexity of changes related to COPD survival [6].
Multidimensional scores improved the sensitivity of the assessment of mortality risk in COPD patients as, though with different specificity, these instruments valued several factors affecting COPD clinical severity and prognosis [6,9,12].
Differently from symptoms subjectively claimed by patients (directly reported or reported via generic and specific questionnaires) and from usual simple lung function indices, the annual cost-of-illness represents an objective and comprehensive parameter which is able to summarize dynamically all the critical issues and the real-life severity and progression of COPD. The major components of the cost depend on the exacerbation and the hospitalization rates and duration and on the extent of drug utilization: These three components account for > 80% of total annual cost. As a consequence, it is absolutely obvious that higher the annual cost, higher the severity and the progression of the disease should be, because characterized by frequent exacerbations, more frequent hospitalizations and requiring a larger use of drugs.
Data of the present study are confirming that the annual cost-of-illness should be regarded as the comprehensive parameter most strictly related to the length of survival over a three-year temporal horizon in COPD: Much more related than any other multidimensional score. Only one paper published a few years ago suggested the challenging concept of the convenience of including the economic impact in a multidimensional score with the aim to assess the severity of COPD [14].
Moreover, data of the present study are also emphasizing the crucial role of proper lung function indices in order to assess the mortality risk. In fact, when the investigation of different aspects of lung function is based on more suitable and specific lung function tests (i.e. RV, DLco), the relationship with the length of survival immediately becomes clear, because emphysema components can be basally assessed. Not by chance, these patients are the same that induce the highest annual cost despite their shorter survival.
Limitations and strengths of the study
The sample consisted of COPD patients referring to a single Lung Unit, even if the majority of patients were belonging to different Italian regions.
The careful characterization of patients in clinical and physiological terms and the careful assessment of primary outcomes (annual cost and mortality) provide strength to the study, prospective in nature.
Despite the costs here considered may be regarded as corresponding to those of the Veneto Region, the costs were uniquely derived from the national DRG tariffs and prices [24] and the basic methodology adopted for the present survey might be adopted in all Countries, independently of the model of their health system. On the other hand, these costs result absolutely comparable to those of other developed Countries and have the advantage of having been based on real-life recent costs of health care.
When compared to the mean duration of COPD, the length of the survey (3 years) might appear relatively short, even if several big studies have the same duration. Anyhow, health care providers and public decision makers ask for and need data at medium term in order to modulate dynamically their interventional plans of chronicity containment and management.
CONCLUSION
The present study confirms that, even if easy to obtain, the most used indices of lung function (namely, FEV1% predicted and FEV1/FVC%) show the lowest power in predicting survival at 3 years, because characterized by a low sensitivity and specificity.
RV% predicted; DLco% predicted proved much more strictly related because more specific in defining the overall lung function pattern and much more appropriate for discriminating emphysema components in COPD (such as, a particular phenotype).
Finally, the total annual cost-of-illness confirms the most sensitive global predictor of mortality in COPD.
In other words, data are supporting the high predicting value of the “functional and economic phenotyping” in terms of COPD patients’ survival.
REFERENCES
- Global Initiative for Chronic Obstructive Lung Disease (2013) Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. Global Initiative for Chronic Obstructive Lung Disease, Wisconsin, United States.
- Mannino DM, Higuchi K, Yu TC, Zhou H, Li Y, et al. (2015) Economic burden of COPD in the presence of comorbidities. Chest 47: 1199-1201.
- Mathers CD, Loncar D (2006) Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 3: 442.
- Negro RWD, Bonadiman L, Turco P, Tognella S, Iannazzo S (2015) Costs of illness analysis in Italian patients with chronic obstructive pulmonary disease (COPD): An update. Clin Econ Outcomes Res 7: 153-159.
- Traver GA, Cline MG, Burrows B (1979) Predictors of mortality in chronic obstructive pulmonary disease. A 15-year follow-up study. Am Rev Respir Dis 119: 895-902.
- Celli BR, Cote CG, Marin JM, Casanova C, Oca MM, et al. (2004) The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 50: 1005-1012.
- Briggs A, Spencer M, Wang H, Mannino D, Sin DD (2008) Development and validation of a prognostic index for health outcomes in chronic obstructive pulmonary disease. Arch Intern Med 168: 71-79.
- Halpin DM, Peterson S, Larsson TP, Calverly PM (2008) Identifying COPD patients at increased risk of mortality: Predictive value of clinical study baseline data. Respir Med 102: 1615-1624.
- Celli BR, Cote CG, Lareau SC, Meek PM (2008) Predictors of survival in COPD: More than just the FEV1. Respir Med 102: 27-35.
- Ko FW, Tam W, Tung AH, Ngai J, Ng SS, et al. (2011) A longitudinal study of serial BODE indices in predicting mortality and readmissions for COPD, Respir Med 105: 266-273.
- Boutou AK, Shrikrishna D, Tanner RJ, Kelly JLSC, Ward SP, et al. (2013) Lung function indices for predicting mortality in COPD. Eur Respir J 42: 616-625.
- Motegi T, Jones RC, Ishii T, Hattori K, Kusonoki Y, et al. (2013) A comparison of three multidimensional indices of COPD severity as predictors of future exacerbations. Intern J COPD 8: 259-271.
- Hurst JR, Vestbo J, Anzueto A, Locantore N, Müllerova H, et al. (2010) Evaluation of COPD longitudinally to identify predictive surrogate end-points (ECLIPSE) investigators. N Engl J Med 363: 1128-1138.
- Negro RWD, Celli RB (2017) Patient Related Outcomes-BODE (PRO-BODE): A composite index incorporating health utilization resources predicts mortality and economic cost of COPD in real life. Respiratory Medicine 131: 175-178.
- Siafakas NM, Vermeire P, Pride NB (1995) Optimal assessment and management of chronic obstructive pulmonary disease (COPD). The european respiratory society task force. Eur Respir J 8: 1398-1420.
- Pauwels RA, Buist AS, Calverly PM, Jenkins CR, Hurd SS (2001) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global initiative for Chronic Obstructive Lung disease (GOLD) Workshop summary. Am J Respire Crit Care Med 631: 1256-1276.
- Nocturnal Oxygen Therapy Trial Group (1980) Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: A clinical trial. Nocturnal oxygen therapy trial group. Ann Intern Med 93: 391-398.
- Gerardi DA, Lovett L, Benoit-Connors ML, Reardon JZ, ZuWallach RL (1996) Variables related to increased mortality following out-patient pulmonary rehabilitation. Eur Respir J 9: 431-435.
- Nishimura K, Izumi T, Tsukino M, Oga T (2002) Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest 121: 1434-1440.
- Goossens LMA, Leimer I, Metzdorf N, Becker K, Molken MPMHR (2014) Does the 2013 GOLD classification improve the ability to predict lung function decline, exacerbations and mortality: A post-hoc analysis of the 4-year UPLIFT trial. BMC Pulm Med 14: 163.
- Cote CG (2006) Surrogates of mortality in chronic obstructive pulmonary disease. Am J Med 119: 54-62.
- Celli BR (2010) Predictors of mortality in COPD. Respir Med 104: 773-779.
- Oga T, Tsukino M, Hajiro T, Ikea A, Nishimura K (2011) Predictive properties of different multidimensional staging systems in patients with chronic obstructive pulmonary disease, Int J Chron Obstruct Pulmon Dis 6: 521-526.
- Italian Ministry of Health (2013) Tariffe delle prestazioni di assistenza ospedaliera per acuti. [DRG tariffs], Gazzetta Ufficiale della Repubblica Italiana. Serie N.23; Supplemento N.8 del 28 gennaio.
Citation: Negro RWD, Bonadiman L, Turco P (2020) The Power of Annual Cost-of-Illness in Predicting COPD Survival at 3 Years. J Pulm Med Respir Res 6: 039.
Copyright: © 2020 Negro RWD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

