Thrombocytopenia and Bleeding in Dengue Fever: A Cross-Sectional Study during a Dengue Outbreak in Burkina Faso
*Corresponding Author(s):
Sawadogo SalamUniversity Of Joseph KI-ZERBO, 03 BP 7021 Ouagadougou 03, Burkina Faso
Tel:+226 70032776,
Email:salemserein@hotmail.com
Abstract
Background and objectives: Dengue virus infection is generally asymptomatic or mild. Thrombocytopenia is a common biological sign and in some severe cases, bleeding can occurs. Our study aimed to assess thrombocytopenia and bleeding in dengue virus infection in Burkina Faso.
Materials and methods: We conducted a cross-sectional study that included cases of dengue fever admitted in seven health facilities during the dengue fever outbreak in 2016 and 2017.All statistic tests were performed at a significance level of 5%.
Results: A total of 296 patients were included, comprising 154 males (52%). The frequency of bleeding was 25%, with no gender difference (p=0.347). Elderly patients (over 55 years) were less likely to bleed (OR = 0.10, CI 95% [0.02-0.63]; p = 0.014), but were more transfused (OR = 8.96, CI 95% [1.07-74.90]; p = 0.043) than younger ones. There was more bleeding patients with moderate thrombocytopenia (OR = 6.84, CI 95% [2.72-17.25]; p = 0.001) and severe thrombocytopenia (OR = 6.66, CI 95% [2.36-18.86]; p = 0.008). The median in-hospital LOS was significantly long (median = 5 [IQR: 4 – 6.5]) days in transfused patients compared to non-transfused ones (median = 4 [IQR: 2 – 5]) days (p = 0.0001).
Conclusion: There was no significant increase in platelet count in transfused and not transfused patients, meaning that platelet transfusion had no longer benefit in reduction of clinical or severe bleeding or improvement in platelet count recovery. Further studies are expected to better explore this issue.
Introduction
The recent emergence and spread of dengue virus (DENV) throughout the world represent a global pandemic threat with an enormous burden on populations, health systems and economies in most tropical countries [1]. Indeed, its incidence increased 30-fold during the five last decades. Around 3.9 billion people in 128 countries are at risk of infection and about 390 million of cases occur annually worldwide [2]. Since 2012, dengue fever emerge as the most important mosquito-borne viral disease in the world because of the widely distribution of its vectors in tropical and subtropical regions. Indeed, Aedes aegypti (the primary vector) and Aedes albopictus (the secondary one) spread globally in recent years, facilitated by multiple phenomena like globalization of trade, fast urbanization in developing countries associated with high population growth rate, inadequate water supply, poor waste management system [3,4]. In Sub-Saharan Africa, reliable epidemiological data on DENV infections are poorly established due to the strong tendency to attribute fevers to malaria [5].
DENV infection is generally asymptomatic in the vast majority of cases (up to 50% or more) or mild with symptoms similar like flu-like illness or other endemic fever diseases (malaria and chikungunya fever) in Africa. However, around 500,000 people are hospitalized each year for severe dengue fever, a potentially fatal complication due to plasma leakage, fluid accumulation, respiratory distress, profuse haemorrhages or organ failure [6]. The mortality rate is reported to be around 2.5% [7]. The pathogenesis and pathophysiology of severe DENV infection are not well-understood. But, some possible contributory factors like age, sex, race, co-morbidities and viral-specific features are described to play a role in disease outcomes [8,9].
Haematological abnormalities are common in severe forms and could be associated to fatal cases in DENV infection [10,11]. Thrombocytopenia due mainly to immunological destruction of platelets, decreased platelet production in bone marrow and attenuation of megakaryocyte maturation is a prominent feature in DENV infection. In conjunction with platelet dysfunction, thrombocytopenia contributes to disturb haemostasis in dengue fever [12-15]. However, haemorrhages is not necessarily correlated with coagulation abnormalities [16]. Especially, the severity of thrombocytopenia does not closely relate to the risk and severity of bleeding [17,18]. Thus, the use of blood component transfusion, mainly platelet concentrate remains polemic. There is no consensus in the guidelines to correct thrombocytopenia or disturbed coagulation parameters [19]. Some authors arguing that the thrombocytopenia, the most striking abnormality, is significant contributor to haemorrhage, use platelet transfusion in bleeding as well in non-bleeding patients.
Burkina Faso regularly experienced dengue outbreaks. The first epidemic known occurred in 1925. From 2013 to 2016, at least three outbreaks were noted. During the 2016 outbreaks, the majority of cases (82.3%) were recorded in Ouagadougou [20]. Our study aimed to assess thrombocytopenia and bleeding risk factors in DENV infection in Burkina Faso.
Materials and Methods
Study settings and design
The study was conducted in seven general public hospitals and private clinics that reported to the Ministry of Health, DENV cases in Ouagadougou, the capital of Burkina Faso. It is a part of the Soudano-Sahelian climate area with a rainy season running from May to October and a dry season from December to May [21]. It counted around 2.6 million inhabitants in 2016 and has been urbanised rapidly during the last quarter of a century with spectacular spatial growth [22-24]. It is characterized by parcelled neighbourhoods close to non-parcelled ones (‘non-lotis’) that lack water supply, sanitation and waste management systems [25].
We carried out a cross-sectional study that included the patients with dengue fever hospitalized in health facilities in Ouagadougou during the dengue fever outbreak in 2016 - 2017. A case of DENV infection was defined as a patient admitted with clinical signs consistent with DENV infection and a positive rapid diagnose test for AgNS1 and/or anti-DENV IgM. Nomolecular biology confirmatory test has been done. Patients with unusable medical records were not included.
Study variables
We considered bleeding signs at admission and platelet transfusions as dependent variables. The independent variables comprised of gender (male or female) age and age group (< 15; 15-24; 25-34; 35-44; 45-54; 55-64 and ≥ 65 years), DENV infection severity according to WHO 2009 classification [19], platelet count and severity of thrombocytopenia (≥ 150,000 or normal, 100,000 -149,999 or mild, 99,999-50,000 or moderate, 49,999-20,000 or severe and < 20,000 or very severe) at admission and exit, in-hospital length of stay and evolution. The data were collected from the patient medical records and blood prescription forms.
Statistical analyses
Data were analyzed using STATA 15 software. We described quantitative and qualitative variables using proportions, means ± 2SD, median with Interquartile Range (IQR) as appropriated. The Chi-square test (or the Fischer's exact test if applicable) and student t test were used to determine association between variables in univariate analysis. Multivariate logistic regression analyses were performed to identify risk factors associated to haemorrhage and platelet transfusion. Non-parametric tests were used to compare haemorrhagic versus non-haemorrhagic and transfused versus non-transfused patients. All tests were performed at a significance level of 5%.
Ethical considerations
The approbation of internal scientific review committee of National blood transfusion center was obtained before study starts. The patients’ anonymity and confidentiality of collected data were preserved.
Results
A total of 296 patients were included, comprising 154 males (52%). The both groups, male and female, are almost similar in their age (p = 0.05), platelet count (p = 0.4), risk of bleeding (0.57), severity of dengue (p = 0.3) in-hospital length of stay (LOS) (p = 0.24) and mortality (p = 0.61). The baseline characteristics of the studied population are summarized on table 1.
|
Parameters |
Overall |
Male |
Female |
p-value |
|
Mean age (years) |
34.2 ± 16.2 |
33.5 ± 14.4 |
35.0 ± 18.1 |
0.44 |
|
Age range < 15 15 – 24 25 – 34 35 – 44 45 – 54 55 – 64 ≥ 65 |
23 (7.8) 64 (21.8) 81 (27.6) 56 (19.1) 31 (10.6) 19 (6.5) 19 (6.5) |
10 (6.5) 37 (24.2) 39 (25.5) 36 (23.5) 19 (12.4) 6 (3.9) 6 (3.9) |
13 (9.3) 27 (19.3) 42 (30.0) 20 (14.3) 12 (8.6) 13 (9.3) 13 (9.3) |
0.05 |
|
Bleeding |
74 (25.0) |
42 (27.3) |
32 (22.5) |
0.347 |
|
Median of pre-transfusion platelet count |
106; [55.5 – 174.5] |
99; [55 – 160] |
113; [56 – 178] |
0.488 |
|
Degree of thrombocytopenia Normal |
95 (33.4) 50 (17.6) 80 (28.2) 52 (18.3) 7 (2.5) |
44 (29.5) 30 (20.1) 45 (30.2) 25 (16.8) 5 (3.4) |
51 (37.8) 20 (14.8) 35 (25.9) 27 (20.0) 2 (1.5) |
0.349 |
|
Bleeding risk None Low Moderate Severe |
145 (51.1) 80 (28.2) 52 (18.3) 7 (2.5) |
74 (49.7) 45 (30.2) 25 (16.9) 5 (3.4) |
71 (52.6) 35 (25.9) 27 (20.0) 2 (1.5) |
0.575 |
|
WHO classification No warning signs Warning signs Severe |
123 (41.5) 162 (54.7) 11 (3.7) |
70 (45.4) 78 (50.6) 6 (3.9) |
53 (37.3) 84 (59.1) 5 (3.5) |
0.336 |
|
Platelet transfusion |
51 (17.2) |
33 (21.4) |
18 (12.7) |
0.05 |
|
Median of post-transfusion platelet count |
120; [79 - 164] |
119; [85 - 167] |
120; [80 - 166] |
0.782 |
|
Median in-hospital LOS |
4; [3 - 5] |
4; [3 - 6] |
4; [3 - 5] |
0.527 |
|
Death |
3 (1.0) |
2 (1.3) |
1 (0.7) |
0.61 |
|
WHO = World health organization; LOS = Length of stay |
||||
Table 1: Baseline characteristics of the patients hospitalized with dengue in Burkina Faso.
Frequencies of thrombocytopenia and bleeding were 66.6% and 25% respectively, with no gender-related differences (table 1). As shown on table 2 and table 3, elderly patients (over 55 years) have less bled (OR = 0.10,CI 95% [0.02-0.63]; p = 0.014) and more transfused (OR = 8.96, CI 95% [1.07-74.90]; p = 0.043) than younger ones. There was more bleeding patients with moderate thrombocytopenia (OR = 6.84, CI95% [2.72-17.25]; p = 0.001) and severe thrombocytopenia (OR = 6.66, CI95% [2.36-18.86]; p = 0.008) than other forms of thrombocytopenia (table 2). Patients with moderate thrombocytopenia (OR = 3.42, CI95% [1.26-9.30]; p = 0.016), severe thrombocytopenia (OR = 6.59, CI95% [2.39-18.19]; p < 0.001) and very severe thrombocytopenia (OR = 19.78, CI95% [3.58-109.35]; p = 0.001) were the most transfused (Table 3).
|
Parameters |
Total |
Bleeding |
Univariate analysis |
Multivariate analysis |
|||||||
|
Yes |
No |
||||||||||
|
N |
n |
% (Row) |
n |
% (Row) |
OR |
CI 95% |
p-value |
OR |
CI 95% |
p-value |
|
|
Sex Male Female |
154 142 |
42 32 |
27.8 22.5 |
112 110 |
72.7 77.5 |
Ref 0.77 |
- 0.45 - 1.32 |
0.348 |
- |
- |
- |
|
Age <15 15-24 25-34 35-44 45-54 ≥ 55 |
23 64 81 56 31 38 |
6 24 22 10 8 3 |
26.1 37.5 27.2 17.9 25.8 7.9 |
17 40 59 46 23 35 |
73.9 62.5 72.8 82.1 74.2 92.1 |
Ref 1.7 1.06 0.61 0.24 |
- 0.59 - 4.90 0.37 - 3.02 0.19 - 1.95 0.29 - 3.37 0.05 - 1.09 |
- 0.326 |
- 0.84 0.46 0.22 0.48 0.10 |
- 0.23 - 3.11 0.12 - 1.73 0.05 - 1.01 0.09 - 2.45 0.02 - 0.63 |
- 0.796 0.249 |
|
Thrombocytopenia Normal Mild Moderate Severe Very severe |
95 50 80 52 7 |
13 9 29 17 1 |
13.7 18.0 36.5 32.7 14.3 |
82 41 51 35 6 |
86.3 82.0 63.7 67.3 85.7 |
Ref 1.38 3.59 3.06 1.05 |
- 0.55 - 3.50 1.71 - 7.53 1.34 - 6.98 0.12 - 9.45 |
- 0.492 0.001 0.008 0.964 |
- 2.19 |
- 0.75 - 6.42 2.72 - 17.25 2.36 - 18.86 0.14 - 22.56 |
- 0.153 |
|
WHO 2009 classification Severe With warning signs No warning signs |
11 162 123 |
2 68 4 |
18.9 42.0 3.3 |
9 94 119 |
81.8 58.0 96.7 |
Ref 3.25 0.15 |
- 0.68 - 15.55 0.02 - 0.94 |
- 0.139 0.043 |
- 3.17 |
- 0.60 - 16.63 0.02 - 0.87 |
- 0.172 0.035 |
|
Rehydration No yes |
34 262 |
12 62 |
35.3 23.7 |
22 200 |
64.7 76.3 |
Ref 0.57 |
- 0.27 - 1.21 |
- 0.144 |
- 0.38 |
- 0.14 - 1.06 |
- 0.065 |
Table 2: Univariate and multivariate analyses of predictors associated to bleeding in patients hospitalized with dengue fever in Burkina Faso.
Goodness-of-fit test of multiple logistic regression: Chi2 = 69.72; 68 df; p = 0.4193
|
Parameters |
Total |
Platelets transfusion |
Univariate analysis |
Multivariate analysis |
|||||||
|
Yes |
No |
||||||||||
|
N |
n |
% (Row) |
n |
% (Row) |
OR |
CI 95% |
p-value |
OR |
CI 95% |
p-value |
|
|
Sex Male Female |
154 142 |
33 18 |
21.4 12.7 |
121 124 |
78.6 87.3 |
Ref 0.53 |
- 0.28 – 0.99 |
0.050 |
- 0.47 |
- 0.22 – 0.98 |
- 0.044 |
|
Age <15 15-24 25-34 35-44 45-54 ≥ 55 |
23 64 81 56 31 38 |
1 11 13 8 7 11 |
4.3 17.2 16.0 14.3 22.6 28.9 |
22 53 68 48 24 27 |
95.7 82.8 84.0 85.7 77.4 71.1 |
Ref 4.57 4.20 3.67 6.42 8.96 |
- 0.55 – 37.53 0.52 – 34.00 0.43 – 31.14 0.73 – 56.41 1.07 – 74.90 |
- 0.158 0.178 0.234 0.094 0.043 |
- 2.40 2.11 1.23 2.20 4.47 |
- 0.26 – 21.93 0.23 – 19.40 0.12 – 12.43 0.21 – 23.20 0.46 – 43.79 |
- 0.439 0.510 |
|
Thrombocytopenia Normal Mild Moderate Severe Very severe |
95 50 80 52 7 |
6 8 15 16 4 |
6.3 16.0 18.8 30.8 57.1 |
89 42 65 36 3 |
93.7 84.0 81.2 69.2 42.9 |
Ref 2.82 3.42 6.59 19.78 |
- 0.92 – 8.66 1.26 – 9.30 2.39 – 18.19 3.58 – 109.35 |
- 0.069 0.016 0.000 0.001 |
- 2.12 |
- 0.65 - 6.86 0.79 – 6.68 1.55 – 14.27 2.07 – 78.69 |
- 0.211 |
|
WHO 2009 classification Severe With warning signs No warning signs |
11 162 123 |
4 29 18 |
36.4 17.9 14.6 |
7 133 105 |
2.9 54.3 42.9 |
Ref 0.38 0.30 |
- 0.10 – 1.39 0.08 – 1.13 |
- 0.144 0.075 |
- 0.32 |
- 0.07 – 1.34 0.06 – 1.08 |
- 0.118 0.063 |
|
Anti-haemorrhage No yes |
194 102 |
21 30 |
10.8 29.4 |
173 72 |
89.9 70.6 |
Ref 3.43 |
- 1.84 – 6.39 |
- 0.000 |
- 2.85 |
- 1.42 - 5.73 |
- 0.003 |
Table 3: Univariate and multivariate analyses of predictors associated to platelet transfusion in patients hospitalized with dengue fever in Burkina Faso.
Goodness-of-fit test of multiple logistic regression: Chi2 = 152.34; 125 df; p = 0.05
The overall median in-hospital LOS was 4 days (IQR [3 - 5]); it was significantly long in transfused patients compared to non-transfused ones (5 [IQR: 4 - 6.5] days versus 4 [IQR: 2 - 5] days; p = 0.0001) (Figure 1-A). At exit, the median increase in platelet count of overall population was 8,000/mm3 (IQR [-48,000 – 60,000]) (Figure 1-B). In platelet-transfused patients, the median increase in platelet count was 27,000/mm3 versus 0/mm3 in non-transfused patients, but the difference was not significant (p = 0.220) (Figure 1-C). Bleeding patients had a median increase in platelet count of 61,000/mm3 compared to a median decrease of 11,000/mm3 in those who did not bleed (p = 0.0001) (Figure 1-D).
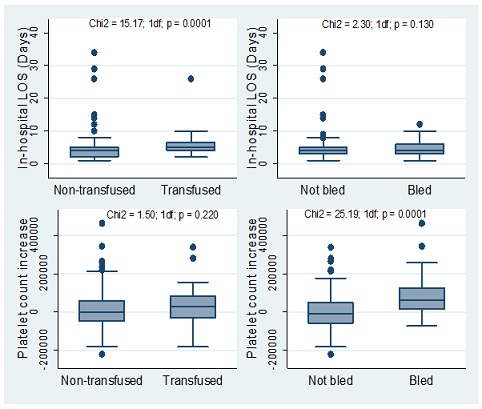
Figure 1: Comparison of in-hospital length of stay and platelet count between transfused and non-transfused patients (A and C respectively) and bled and non-bled patients (B and D respectively) during dengue fever outbreak in Burkina Faso. LOS = Length of stay
The overall mortality rate was 1%. There were no differences in mortality rates between transfused and non-transfused patients (0% versus 1.2%; p = 0.42) as well as between those who bled and those who did not (0% versus 1.3%; p = 0.56).
Discussion
Our study aimed to evaluate the prevalence of thrombocytopenia and bleeding risk factors among dengue fever patients during DENV infection outbreak in Burkina Faso. We found that 66.6% of patients had thrombocytopenia, 25% have bled and 17.2% received platelet transfusion. Moderate (OR = 6.84, p < 0.001) and severe (OR = 6.66, p < 0.001) thrombocytopenia were positively associated to bleeding while platelet transfusion was instead determined by severe and very severe thrombocytopenia. Platelet transfusion appears to prolong in-hospital LOS without improving platelet count significantly.
During the current decade, Burkina Faso has experienced regular DENV infection outbreaks [20]. All the four DENV serotypes have been listed as circulating in Burkina Faso [5,26].Different aspects have been addressed by several authors in previous studies [5,20,27-31], but thrombocytopenia, bleeding risk factors and platelet transfusions, not yet. Also, our study makes it possible to fill this gap. But some limitations needed to be addressed. Indeed, the data used in our study are dependent on the thoroughness of clinician’s documentation. In addition, the decision to transfuse platelets dependedon the physician willing only, due to the absence of national guidelines. Also, it was difficult to determine whether the transfusions were appropriate or not. Furthermore, we did not determined the different serotypes involved in our patients. However, some arguments tend to show that the severity of the infection, the thrombocytopenia and the importance of the bleeding are associated with the viral serotypes, whether it is a mono-infection or co-infection [32]. Finally, patients were not followed up to assess full recovery.
Thrombocytopenia and bleeding are relative common problems in dengue fever. In our study, thrombocytopenia and bleeding were found in 66.6% and 25%. From 2013 to 2014, Diallo, et al. in their study found bleeding forms in 18.4% and thrombocytopenia in 57.1% of cases [27]. In a population of pregnant women, Sondo, et al. have noted bleeding in 16% and thrombocytopenia in 48% [30]. Other authors in different context found higher rate of thrombocytopenia (over 80%) [33]. Thrombocytopenia is a stressful situation for patients and their families, but also for treating physicians, due to its spectacular depth. In some patients, platelet count decrease under 20,000 /mm3. In our study, these cases represented 2.5%.
The dreaded complication in case of thrombocytopenia is haemorrhage. This leads sometimes to transfuse platelet concentrate. Indeed, in many countries, management of thrombocytopenia and haemorrhage in DENV infection uses platelet transfusion. This decision is most often made by the clinician on the basis of the dramatic drop in platelets and in order to anticipate bleeding diathesis, leading sometimes to misuse. In our study, platelet transfusion were made in 17.2% of overall patients. This is consistent with many other studies [34]. In our study, the decision to transfuse platelets is associated to patients’ platelets count and not haemorrhage (Table 3). This allows us to say that in our study, the clinicians had “proactive attitude”; they seemed to be in a bleeding prevention posture.
But as already reported [17,35,36], there was poor correlation between thrombocytopenia and bleeding occurrence in our study. Moderate thrombocytopenia and severe thrombocytopenia had respectively odds ratios of 6.8 (CI 95% [2.72 - 17.25]; p < 0.001) and 6.7 (CI 95% [2.36 - 18.86]; p < 0.001) for bleeding risk versus 2.7 (CI 95% [0.14 – 22.56]; p = 0.664) for very severe thrombocytopenia. This suggests distinct pathophysiologic processes between thrombocytopenia and bleeding in dengue fever. The mechanisms of thrombocytopenia include bone marrow suppression, peripheral immunologic destruction of platelets and increased platelet activation due to vascular injury. Thus, the bleeding could mainly result from the vascular alteration which promotes the thrombocytopenia and the coagulation disorders, in association with the cytokines secreted due to the infection [16,35]. In these conditions, platelet transfusion cannot be the only way to manage the haemorrhagic risk in dengue fever.
Moreover, platelet transfusion seems to be of no benefit to patients. On the contrary, in addition to not bringing any gain in platelets count, it lengthens the duration of hospitalization (median of 5 days in transfused patients versus 4 days in non-transfused ones). The consequence is an increased economic burden for the patient and society. In addition, platelet transfusion does not influence mortality either. Also, these findings question the well-founded and the need of platelet transfusion in dengue fever. Further studies are needed to elucidate this. In the meantime, we say that inappropriate platelet transfusions will lead to shortages of platelet concentrates for patients with blood disorders whose survival depends on platelet transfusions. They will also expose recipients to risks of bacterial, HIV and hepatitis contaminations, allo-immunizations, acute lung injuries, pulmonary oedema, since they are far from being controlled in Sub-Saharan Africa [37-40].
Thrombocytopenia and bleeding are common complication of dengue infection. The mechanisms of these disorders are multifactorial. In view of the scarcity and the safety concerns of blood products in resource-limited settings, prophylactic platelet transfusion is not recommended, since no benefit in reduction of severe bleeding or improvement in platelet count recovery was demonstrated. Further studies are expected to better explore this issue.
Acknowledgments
The authors would like to acknowledge the health facilities’ officials who authorized data collection.
References
- WHO (2020) Global strategy for dengue prevention and control, 2012-2020. WHO, Geneva, Switzerland.
- Simo FBN, Bigna JJ, Kenmoe S, Ndangang MS, Temfack E, et al.(2019) Dengue virus infection in people residing in Africa: a systematic review and meta-analysis of prevalence studies. Sci Rep 9:13626.
- Amarasinghe A, Kuritsky JN, Letson W, Margolis HS (2011) Dengue Virus Infection in Africa Emerg Infect Dis 17: 1349-1354.
- Messina JP, Brady OJ, Scott TW, Zou C, Pigott GM, et al (2014) Global spread of dengue virus types: mapping the 70 year history Trends Microbiol 22: 138-146.
- Tarnagda Z, Cissé A, Bicaba BW, Diagbouga S, Sagna T, et al (2018) Dengue Fever in Burkina Faso, 2016. Emerg Infect Dis 24: 170-172.
- WHO (2020) Dengue and severe dengue. Geneva, Switzerland.
- Chaurasia R, Zaman S, Chatterjee K, Das B (2015) Retrospective Review of Platelet Transfusion Practices during 2013 Dengue Epidemic of Delhi, India. Transfus Med Hemotherapy 42: 227-231.
- Guo C, Zhou Z, Wen Z, Liu Y, Zeng C, et al. (2017) Global Epidemiology of Dengue Outbreaks in 1990–2015: A Systematic Review and Meta-Analysis. Front Cell Infect Microbiol 7: 317.
- Mallhi TH, Khan AH, Adnan AS, Sarriff AB, Khan YH, et al (2015) Clinico-laboratory spectrum of dengue viral infection and risk factors associated with dengue hemorrhagic fever: a retrospective study. BMC Infect Dis 15: 399.
- Pinto RC, de Castro DB, de Albuquerque BC, Sampaio V, dos Passos RA, et al. (2016) Mortality Predictors in Patients with Severe Dengue in the State of Amazonas, Brazil. PLOS ONE 11: 0161884.
- Sam S-S, Omar SFS, Teoh B-T, Abd-Jamil J, AbuBakar S (2013) Review of Dengue Hemorrhagic Fever Fatal Cases Seen Among Adults: A Retrospective Study. PLoS Negl Trop Dis 7: 2194.
- Azeredo EL de, Monteiro RQ, Pinto LM de-O (2015) Thrombocytopenia in Dengue: Interrelationship between Virus and the Imbalance between Coagulation and Fibrinolysis and Inflammatory Mediators. Mediators Inflamm 2015;2015:313842 .
- Machado AAV, Negrão FJ, Croda J, Medeiros ESD, Pires MPDS (2019) Safety and costs of blood transfusion practices in dengue cases in Brazil. PLOS ONE 14: 0219287.
- Chuansumrit A, Chaiyaratana W (2014) Hemostatic derangement in dengue hemorrhagic fever. Thromb Res 133: 10-16.
- Wills BA, Oragui EE, Stephens AC, Daramola OA, Dung NM, et al (2002) Coagulation Abnormalities in Dengue Hemorrhagic Fever: Serial Investigations in 167 Vietnamese Children with Dengue Shock Syndrome. Clin Infect Dis 35: 277-285.
- Krishnamurti C, Kalayanarooj S, Cutting MA, Peat RA, Rothwell SW, et al (2001) Mechanisms of hemorrhage in dengue without circulatory collapse. Am J Trop Med Hyg 65: 840-847.
- Lum LCS, Goh AYT, Chan PWK, El-Amin, El-Amin, A-LM, Lam SK (2002) Risk factors for hemorrhage in severe dengue infections. J Pediatr 140: 629-631.
- Lye DC, Lee VJ, Sun Y, Leo YS (2009) Lack of Efficacy of Prophylactic Platelet Transfusion for Severe Thrombocytopenia in Adults with Acute Uncomplicated Dengue Infection. Clin Infect Dis 48: 1262-1265.
- 19. WHO (2009) Dengue: guidelines for diagnosis, treatment, prevention, and control. WHO, Geneva, Switzerland.
- Sawadogo S, Baguiya A, Yougbare F, Bicaba BW, Nebie K, et al (2020) Seroprevalence and factors associated with IgG anti-DENV positivity in blood donors in Burkina Faso during the 2016 dengue outbreak and implications for blood supply. Transfus Med 30: 37-45.
- Lim JK, Carabali M, Lee J-S, Lee K-S, Namkung S, et al (2018) Evaluating dengue burden in Africa in passive fever surveillance and seroprevalence studies: protocol of field studies of the Dengue Vaccine Initiative. BMJ Open 28: 1-14.
- INSD I national de la statistique et de la démographie. Projections demographiques de 2007-2020.
- United Nations D of SA Population Division. World Urbanization Prospects The 2014 Revision (ST/ESA/SER.A/366), https://esa.un.org/unpd/wup/publications/files/wup2014-report.pdf (2015, accessed 8 February 2019)
- Fournet F, Rican S, Vaillant Z, Roudot A, Anna R, et al (2016) The Influence of Urbanization Modes on the Spatial Circulation of Flaviviruses within Ouagadougou (Burkina Faso) Int J Environ Res Public Health 13: 1-14.
- INSD I national de la statistique et de la démographie. Enquête multisectorielle continue (EMC) 2014: Habitat, assainissement et accès à l’eau potable. Ouagadougou: INSD.
- Ridde V, Agier I, Bonnet E, Carabali M, Dabiré KR, et al (2016) Presence of three dengue serotypes in Ouagadougou (Burkina Faso): research and public health implications. Infect Dis Poverty 5:1–13.
- Diallo I, Sondo KA, Tieno H, Tamelokpo EY, Zoungrana Y, et al. (2017) À propos de 98 cas de dengue hospitalisés dans une clinique privée de Ouagadougou? aspects épidémiologiques, diagnostiques et évolutifs. Bull Société Pathol Exot 110: 291-296.
- Coulibaly G, Lengani HYA, Sondo KA, Konvolbo HP (2020) Épidémiologie de l’insuffisance rénale aiguë au cours de la dengue dans la ville de Ouagadougou. Néphrologie Thérapeutique 16: 27-32.
- Sondo KA (2017) Facteurs associés à la dengue sévère à Ouagadougou (Burkina Faso). In: Financement de la santé dans les pays à ressources limitées & arboviroses: un autre regard. Marseille: GISPE 59.
- Sondo KA, Ouattara A, Diendéré EA, Diallo I, Zoungrana J, et al (2019) Dengue infection during pregnancy in Burkina Faso: a cross-sectional study. BMC Infect Dis 19:997.
- Tarnagda Z, Congo M, Sagna T, Ouédraogo C, Sagna T, et al (2014) Outbreak of dengue fever in Ouagadougou, Burkina Faso, 2013. Int J Microbiol Immunol Res 2: 101-108.
- Dhanoa A, Hassan SS, Ngim CF, Lau CF, Chan TS, et al (2016) Impact of dengue virus (DENV) co-infection on clinical manifestations, disease severity and laboratory parameters. BMC Infect Dis 16: 406.
- Chairulfatah A, Setiabudi D, Agoes R, Colebunders R, Colebunders R (2003) Thrombocytopenia and Platelet Transfusions in Dengue Haemorrhagic Fever and Dengue Shock Syndrome 27: 7.
- Chaudhary R, Khetan D, Sinha S, Sinha P, Sonker A, et al (2006) Transfusion support to Dengue patients in a hospital based blood transfusion service in north India. Transfus Apher Sci 35:239–244.
- Chuansumrit A, Tangnararatchakit K (2006) Pathophysiology and management of dengue hemorrhagic fever. Transfus Altern Transfus Med 8: 3-11.
- Lye DC, Archuleta S, Syed-Omar SF, Low JG, Oh HM, et al (2017) Prophylactic platelet transfusion plus supportive care versus supportive care alone in adults with dengue and thrombocytopenia a multicentre, open-label, randomised, superiority trial. The Lancet 389: 1611-1618.
- Yooda AP, Sawadogo S, Soubeiga ST, Obiri-Yeboah D, et al (2019) Residual risk of HIV, HCV, and HBV transmission by blood transfusion between 2015 and 2017 at the Regional Blood Transfusion Center of Ouagadougou, Burkina Faso. J Blood Med Volume 10: 53-58.
- Bloch EM, Vermeulen M, Murphy E (2012) Blood Transfusion Safety in Africa: A Literature Review of Infectious Disease and Organizational Challenges. Transfus Med Rev 26: 164-180.
- Dhingra N (2020) Making safe blood available in Africa. WHO Comm Int Relat Subcomm Afr Glob Hum Rights Int Oper US House Represent Genève OMS.
- Barro L, Drew VJ, Poda GG, Tagny CT, Tagny CT, et al (2018) Blood transfusion in sub-Saharan Africa: understanding the missing gap and responding to present and future challenges. Vox Sang 113: 726-736.
Citation: Sawadogo S, Nebie K, Koulidiati J, Zoehinga O, Donatien K, et al. (2021) Thrombocytopenia and bleeding in dengue fever: a cross-sectional study during a dengue outbreak in Burkina Faso. J Hematol Blood Transfus Disord 8: 26
Copyright: © 2021 Sawadogo Salam, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.