
Sports Medicine and Injury Care Journal Category: Medical
Type: Case Report
Unilateral Spondylolysis and Contralateral Lamina Fracture in a Professional Soccer Player: Surgical Treatment without Arthrodesis- Case Report and Literature Review
*Corresponding Author(s):
Robert MevesDepartment Of Orthopedics And Trauma, Faculty Of Medical Sciences, Santa Casa De Misericórdia De São Paulo, Brazil
Tel:+55 1121761525,
Email:robertmeves@hotmail.com
Received Date: Sep 04, 2019
Accepted Date: Oct 18, 2019
Published Date: Oct 24, 2019
Abstract
Spondylolysis is a well-known disorder frequently causing lumbar pain in athletes. The unilateral defect of the pars interarticularis has rarely been reported in the literature and in most cases a contralateral defect was present. We present a case of a 21-year old male professional soccer player reporting persistent lumbar pain for three years. The Computed Tomography (CT) scan has showed the presence of right L5 spondylolysis associated with stress fracture of the left lamina of this vertebra. The pars interarticularis defect was stabilized with pedicle screw and laminar hook. The left lamina fracture was fixed with two interfragment screws. During postoperative follow-up (twenty-four month), the patient reported complete pain relief. Six months after the surgery the patient was able to resume sports activities as before.
Keywords
Athletes; Fractures; Humans; Lumbar vertebrae; Return to Sport; Spine; Spondylolysis/surgery; Stress/surgery
INTRODUCTION
Sports that require athletes to repeatedly place the spine in hyperextension may exacerbate both spondylolysis and spondylolisthesis with activity restrictions and a structured rehabilitation program can help in return to most sports. Surgical treatment may be required for patients who have symptoms that are unresponsive to nonsurgical treatment and patients who have grade III or grade IV spondylolisthesis [1].
Low back pain is a common symptom in athletes. Generally the painful events are caused by self-limited muscle sprains. Persistent lumbar pain is usually associated to degenerative disc disease, spondylolysis, stress fracture, facet syndrome or other spine disorders [2].
Spondylolysis is characterized by a defect of the pars interarticularis of the posterior vertebral arch and is often found in radiographs of asymptomatic individuals. Sports practice is an important triggering factor for developing defect in the pars interarticularis. Symptomatic spondylolysis has been a frequent cause of lumbar pain in athletes [3]. The most frequent site of spondylolysis is L5 and most cases are bilateral [4]. Unilateral spondylolysis is uncommon and most cases reported are associated with contralateral posterior arch defects, such as contralateral bone hypertrophy, bone sclerosis, and stress fractures of the pedicle [5-13].
Unilateral spondylolysis associated to fracture of the contralateral lamina is an extremely rare condition, which was reported in literature only twice to date [14,15].
This is a case report of a professional soccer player with persistent lumbar pain diagnosed as unilateral spondylolysis associated with contralateral lamina fracture. Unlike the individuals reported in medical literature, who were submitted to arthrodesis, our patient underwent surgical fixation of the lesions. We documented the medical and radiological follow-up for two years.
Low back pain is a common symptom in athletes. Generally the painful events are caused by self-limited muscle sprains. Persistent lumbar pain is usually associated to degenerative disc disease, spondylolysis, stress fracture, facet syndrome or other spine disorders [2].
Spondylolysis is characterized by a defect of the pars interarticularis of the posterior vertebral arch and is often found in radiographs of asymptomatic individuals. Sports practice is an important triggering factor for developing defect in the pars interarticularis. Symptomatic spondylolysis has been a frequent cause of lumbar pain in athletes [3]. The most frequent site of spondylolysis is L5 and most cases are bilateral [4]. Unilateral spondylolysis is uncommon and most cases reported are associated with contralateral posterior arch defects, such as contralateral bone hypertrophy, bone sclerosis, and stress fractures of the pedicle [5-13].
Unilateral spondylolysis associated to fracture of the contralateral lamina is an extremely rare condition, which was reported in literature only twice to date [14,15].
This is a case report of a professional soccer player with persistent lumbar pain diagnosed as unilateral spondylolysis associated with contralateral lamina fracture. Unlike the individuals reported in medical literature, who were submitted to arthrodesis, our patient underwent surgical fixation of the lesions. We documented the medical and radiological follow-up for two years.
CASE REPORT
A 21-year old male professional soccer player was admitted to our service reporting persistent lumbar pain for three years. Pain worsened with movement thus affecting his sports activities. There was little pain improvement with non-hormonal anti-inflammatory drugs; total rest was a factor for pain relief. No radicular symptoms were present. The patient denied previous trauma or comorbidities.
Physical exam revealed pain when palpating the left paravertebral muscles with worsening of the pain with hyperextension and rotation of the back. No neurological abnormalities were observed.
The postero-anterior and orthostatic lateral and oblique views of the lumbosacral spine suggested a right pars interarticularis defect at L5, but no other evident alterations (Figure 1). The Computed Tomography (CT) scan confirmed the presence of right L5 spondylolysis associated with stress fracture of the left lamina of this vertebra. The image suggested pseudoarthrosis (Figures 2 and 3).
Physical exam revealed pain when palpating the left paravertebral muscles with worsening of the pain with hyperextension and rotation of the back. No neurological abnormalities were observed.
The postero-anterior and orthostatic lateral and oblique views of the lumbosacral spine suggested a right pars interarticularis defect at L5, but no other evident alterations (Figure 1). The Computed Tomography (CT) scan confirmed the presence of right L5 spondylolysis associated with stress fracture of the left lamina of this vertebra. The image suggested pseudoarthrosis (Figures 2 and 3).
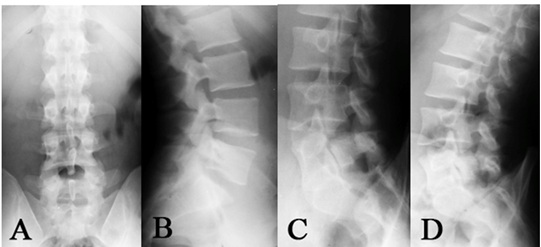
Figure 1: Radiographs: A, AP with no significant changes; B, Lateral view showing spondylolysis at L5 ; C and D, Oblique view confirming spondylolysis at L5.

Figure 2: Axial computed tomography showing spondylolysis at L5 with contralateral lamina fracture.
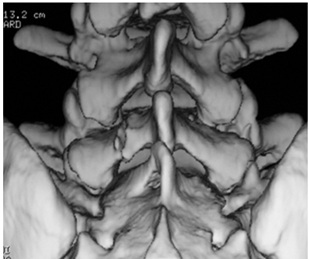
Figure 3: Three-dimensional reconstruction tomography demonstrating fracture of the L5 left lamina.
Surgical treatment of the lesions was performed. The pars interarticularis defect was stabilized with pedicle screw and laminar hook. The left lamina fracture was fixed with two 3.5 mm interfragment screws (Figure 4).
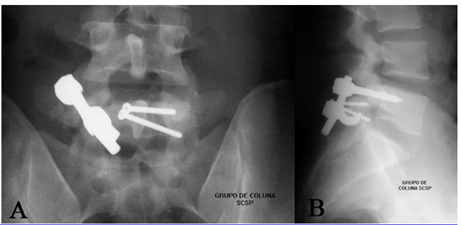 Figure 4: AP radiograph demonstrating fixation of left lamina fracture with 2 screws and stabilization of spondylolysis with screw-rod-hook. B, Lateral view better shows stabilization with screw-rod-hook of pars impairment.
Figure 4: AP radiograph demonstrating fixation of left lamina fracture with 2 screws and stabilization of spondylolysis with screw-rod-hook. B, Lateral view better shows stabilization with screw-rod-hook of pars impairment.Autologous bone graft of the iliac crest was placed in both lesions. Since the patient had no signs of lumbar instability or disc degeneration on the Magnetic Resonance Imaging (MRI) (Figure 5), arthrodesis was not performed.
 Figure 5: Magnetic resonance imaging (T2) shows normal aspect of intervertebral discs and absence of vertebral instability signs.
Figure 5: Magnetic resonance imaging (T2) shows normal aspect of intervertebral discs and absence of vertebral instability signs.During postoperative follow-up, the patient reported complete pain relief and no orthesis was prescribed. Physical therapy was performed for 3 months. Radiologic consolidation of the lesions was evident three months after surgery. Six month after the surgery the patient was able to resume sports activities as before. Osteosynthesis was removed one year after the procedure (Figures 6 to 8).
 Figure 6: A, AP radiograph after removal synthesis material (one year after surgery). B, Lateral view shows consolidation of spondylolysis.
Figure 6: A, AP radiograph after removal synthesis material (one year after surgery). B, Lateral view shows consolidation of spondylolysis. Figure 7: Axial computed tomography (one-year follow-up) demonstrating consolidation of spondylolysis and lamina fracture.
Figure 7: Axial computed tomography (one-year follow-up) demonstrating consolidation of spondylolysis and lamina fracture. Figure 8: Three-dimensional reconstruction tomography demonstrating consolidation of left lamina one year after surgery.
Figure 8: Three-dimensional reconstruction tomography demonstrating consolidation of left lamina one year after surgery.After twenty-four month follow-up the patient is still asymptomatic and plays soccer, participating in professional championships with no functional lumbosacral limitation and high competitive sport level.
DISCUSSION
Mechanical factors combined with rapid growth during adolescence place stress on the spine and can result in a stress fracture [1]. The prevalence of bilateral spondylolysis is approximately 6% in Caucasians [16]. The unilateral defect of the pars interarticularis has rarely been reported in the literature and in most cases a contralateral defect was present [6,7,9,12,15,17-19].
Spondylolysis is a well known disorder frequently causing lumbar pain in athletes. As professional athletes have to resume their sports activities sooner, treatment has to be carried out immediately in order to reduce the time length away from the competitions.
The reported case presents an extremely rare association of unilateral spondylolysis and fracture of the contralateral lamina. Only two similar cases are reported in the literature till this date [14,15] and one of them was also a professional soccer player [14]. For both cases, arthrodesis was performed by reason of signs in the image examinations compatible with degenerative discal disease.
Contralateral posterior arch hypertrophy was reported in association with unilateral spondylolysis by some authors [6,20-23]. In 1976, Maldague and Malghem [22] defined this finding as “vertebral ansiocoria”, representing a load distribution on the posterior arch exposed to tension in the presence of a unilateral defect of the pars interarticularis. In 1984, Amato et al.,[20] were the first authors to report lamina lesions associated with spondylolysis describing it as “lamina fragmentation”. They observed lamina fragmentation in eight out of 56 patients examined but did not mention which cases were associated to unilateral spondylolysis.
In our case we believe that the lamina lesion was due to a stress fracture developing to pseudoarthrosis, according to CT scan images (Figure 2).
In 2005, Pascal-Mousselard et al., [14] reported the case of a 26-year old male professional soccer player with a similar lesion. At first their patient was treated nonsurgical and did not practice sports for three months. Although he had complete pain relief, after eight months the symptoms recurred and consolidation failure of the lamina fracture was diagnosed. After another attempt of conservative treatment the lamina fracture consolidated but pain and pars interarticularis defect remained. Therefore the authors did L5-S1 arthrodesis with no instrumentation. The patient returned to sports one year later but with lower performance due to his age and time without training.
Spondylolysis treatment is controversial. Most patients are asymptomatic. Patients with pain and bilateral spondylolysis generally show good results with non-surgical treatment. However, chronic and untreatable pain may be an indication for surgical procedure.
There are few cases reported of successful non-surgical treatment of unilateral spondylolysis. According to the literature, surgery was needed in 15 of the 20 cases reported so far [6-9,11-14,17-19]. It seems that early surgical treatment leads to more effective outcomes in professional athletes reducing treatment and rehabilitation time.
In the case presented, stabilization of the area of the defect of pars interarticularis was performed with the use of a pedicle screw and a rod connected to a laminar hook. The lamina fracture was fixed with two 3.5 mm interfragment screws. Iliac crest autologous graft was added to both lesions.
Since the patient had no signs of instability on the segment and the intervertebral disc showed no degeneration (Figure 8), arthrodesis was not performed. This was a major factor to preserve motility and to allow patient’s early rehabilitation.
Several surgical techniques have been described for spondylolysis [24]. The procedures most often used are direct repair of the pars interarticularis with bone graft, use of screws, wiring, and combination of screw-rod-hook [24-26].
In 1968, Kimura [27] described the direct spondylolysis repair. Bone grafts with no internal fixation of the lesion were performed. In 1971, Buck [25] presented a new fixation approach using screws in the pars interarticularis, thus allowing the patient’s early mobility. Other surgeons reported direct repair of the lesion, such as Scott technique (wiring with steel wires around the transverse processes and stiffening below the spinous process); the modified Scott technique (wiring with steel wires around cortical screws placed in both pedicles and stiffened below the spinous process); the combined screw - rod - hook (Morscher technique with Harrington hook inserted under the lamina and fixated to the superior articulate process with a screw; or the conventional screw - rod - hook approach) [24,26].
Deguchi et al.,[28], in 1999, compared biomechanics of the different spondylolysis fixation approaches. Spondylolytic defects were created in nine fresh cadavers. Comparing the Scott, modified Scott, Buck, and the screw - rod - hook techniques, it was observed that the latter approach allowed less spine motility on the defect site in spinal flexion.
The treatment of competing athletes is still a challenge. Despite no consensus about the best treatment, surgery should be considered for these patients. Arthrodesis of the affected segment, although much used in the past, is not always necessary and should be avoided whenever there is no instability or degenerative disc disorder to preserve lumbar spine mobility [29,30]. Our patient was the only one subject reported in the literature submitted to fixation without arthrodesis. What enabled this management was the normal lumbar MRI without any sign of disc degeneration. In the case described, the patient presented fast relief of symptoms and resumed professional sports practice at the same level of performance than before surgery.
Spondylolysis is a well known disorder frequently causing lumbar pain in athletes. As professional athletes have to resume their sports activities sooner, treatment has to be carried out immediately in order to reduce the time length away from the competitions.
The reported case presents an extremely rare association of unilateral spondylolysis and fracture of the contralateral lamina. Only two similar cases are reported in the literature till this date [14,15] and one of them was also a professional soccer player [14]. For both cases, arthrodesis was performed by reason of signs in the image examinations compatible with degenerative discal disease.
Contralateral posterior arch hypertrophy was reported in association with unilateral spondylolysis by some authors [6,20-23]. In 1976, Maldague and Malghem [22] defined this finding as “vertebral ansiocoria”, representing a load distribution on the posterior arch exposed to tension in the presence of a unilateral defect of the pars interarticularis. In 1984, Amato et al.,[20] were the first authors to report lamina lesions associated with spondylolysis describing it as “lamina fragmentation”. They observed lamina fragmentation in eight out of 56 patients examined but did not mention which cases were associated to unilateral spondylolysis.
In our case we believe that the lamina lesion was due to a stress fracture developing to pseudoarthrosis, according to CT scan images (Figure 2).
In 2005, Pascal-Mousselard et al., [14] reported the case of a 26-year old male professional soccer player with a similar lesion. At first their patient was treated nonsurgical and did not practice sports for three months. Although he had complete pain relief, after eight months the symptoms recurred and consolidation failure of the lamina fracture was diagnosed. After another attempt of conservative treatment the lamina fracture consolidated but pain and pars interarticularis defect remained. Therefore the authors did L5-S1 arthrodesis with no instrumentation. The patient returned to sports one year later but with lower performance due to his age and time without training.
Spondylolysis treatment is controversial. Most patients are asymptomatic. Patients with pain and bilateral spondylolysis generally show good results with non-surgical treatment. However, chronic and untreatable pain may be an indication for surgical procedure.
There are few cases reported of successful non-surgical treatment of unilateral spondylolysis. According to the literature, surgery was needed in 15 of the 20 cases reported so far [6-9,11-14,17-19]. It seems that early surgical treatment leads to more effective outcomes in professional athletes reducing treatment and rehabilitation time.
In the case presented, stabilization of the area of the defect of pars interarticularis was performed with the use of a pedicle screw and a rod connected to a laminar hook. The lamina fracture was fixed with two 3.5 mm interfragment screws. Iliac crest autologous graft was added to both lesions.
Since the patient had no signs of instability on the segment and the intervertebral disc showed no degeneration (Figure 8), arthrodesis was not performed. This was a major factor to preserve motility and to allow patient’s early rehabilitation.
Several surgical techniques have been described for spondylolysis [24]. The procedures most often used are direct repair of the pars interarticularis with bone graft, use of screws, wiring, and combination of screw-rod-hook [24-26].
In 1968, Kimura [27] described the direct spondylolysis repair. Bone grafts with no internal fixation of the lesion were performed. In 1971, Buck [25] presented a new fixation approach using screws in the pars interarticularis, thus allowing the patient’s early mobility. Other surgeons reported direct repair of the lesion, such as Scott technique (wiring with steel wires around the transverse processes and stiffening below the spinous process); the modified Scott technique (wiring with steel wires around cortical screws placed in both pedicles and stiffened below the spinous process); the combined screw - rod - hook (Morscher technique with Harrington hook inserted under the lamina and fixated to the superior articulate process with a screw; or the conventional screw - rod - hook approach) [24,26].
Deguchi et al.,[28], in 1999, compared biomechanics of the different spondylolysis fixation approaches. Spondylolytic defects were created in nine fresh cadavers. Comparing the Scott, modified Scott, Buck, and the screw - rod - hook techniques, it was observed that the latter approach allowed less spine motility on the defect site in spinal flexion.
The treatment of competing athletes is still a challenge. Despite no consensus about the best treatment, surgery should be considered for these patients. Arthrodesis of the affected segment, although much used in the past, is not always necessary and should be avoided whenever there is no instability or degenerative disc disorder to preserve lumbar spine mobility [29,30]. Our patient was the only one subject reported in the literature submitted to fixation without arthrodesis. What enabled this management was the normal lumbar MRI without any sign of disc degeneration. In the case described, the patient presented fast relief of symptoms and resumed professional sports practice at the same level of performance than before surgery.
CONCLUSION
Spondylolysis is a common radiological finding that generally appears in childhood without any symptoms, but it may progress to persistent lumbar pain, especially in athletes.
Lesions of pars interarticularis are usually bilateral. Few cases of unilateral spondylolysis have been reported.
The association of unilateral spondylolysis and contralateral lamina fracture is rare and there are only two cases reported in literature. Our patient was the only one submitted to fixation without arthrodesis. It is believed that load distribution on the posterior arch causes the contralateral lesion. Most of these lesions are pedicle fractures.
Lamina fracture associated to spondylolysis generally consolidates spontaneously but pseudoarthrosis may occur, especially in athletes taking part in high level competitions. In these cases, surgical treatment seems to lead to early return to sports activities with better results. Treatment and return to competitive sports must be individualized based on the severity and symptoms of the disease in each patient.
Lesions of pars interarticularis are usually bilateral. Few cases of unilateral spondylolysis have been reported.
The association of unilateral spondylolysis and contralateral lamina fracture is rare and there are only two cases reported in literature. Our patient was the only one submitted to fixation without arthrodesis. It is believed that load distribution on the posterior arch causes the contralateral lesion. Most of these lesions are pedicle fractures.
Lamina fracture associated to spondylolysis generally consolidates spontaneously but pseudoarthrosis may occur, especially in athletes taking part in high level competitions. In these cases, surgical treatment seems to lead to early return to sports activities with better results. Treatment and return to competitive sports must be individualized based on the severity and symptoms of the disease in each patient.
REFERENCES
- Warner WC Jr, de Mendonça RGM (2017) Adolescent Spondylolysis: Management and Return to Play. Instr Course Lect 66: 409-413.
- Bono CM (2004) Low-back pain in athletes. J Bone Joint Surg Am 86: 382-396.
- Rossi F, Dragoni S (1990) Lumbar spondylolysis: occurrence in competitive athletes. Updated achievements in a series of 390 cases. J Sports Med Phys Fitness 30: 450-452.
- Standaert CJ, Herring SA (2000) Spondylolysis: a critical review. Br J Sports Med 34: 415-422.
- Porter RW, Park W (1982) Unilateral spondylolysis. J Bone Joint Surg Br 64: 344-348.
- Aland C, Rineberg BA, Malberg M, Fried SH (1986) Fracture of the pedicle of the fourth lumbar vertebra associated with contralateral spondylolysis. Report of a case. J Bone Joint Surg Am 68: 1454-1455.
- Araki T, Harata S, Nakano K, Satoh T (1992) Reactive sclerosis of the pedicle associated with contralateral spondylolysis. Spine (Phila Pa 1976)17: 1424-1426.
- Chong VF, Htoo MM (1997) Pedicular stress fracture in the lumbar spine. Australas Radiol 41: 306-307.
- Garber JE, Wright AM (1986) Unilateral spondylolysis and contralateral pedicle fracture. Spine (Phila Pa 1976) 11: 63-66.
- Gerrard DF, Doyle TC (1998) Lumbosacral pain in an athlete: an unusual site for stress fracture. Clin J Sports Med 8: 59 - 61.
- Guillodo Y, Botton E, Saraux A, Le Goff P (2000) Contralateral spondylolysis and fracture of the lumbar pedicle in an elite female gymnast: a case report. Spine (Phila Pa 1976)25: 2541-2543.
- Maurer SG, Wright KE, Bendo JA (2000) Iatrogenic spondylolysis leading to contralateral pedicular stress fracture and unstable spondylolisthesis: a case report. Spine (Phila Pa 1976) 25: 895-898.
- Weatherley CR, Mehdian H, Berghe LV (1991) Low back pain with fracture of the pedicle and contralateral spondylolysis. A technique of surgical management. J Bone Joint Surg Br 73: 990-993.
- Pascal-Moussellard H, Broizat M, Cursolles JC, Rouvillain JL, Catonné Y (2005) Association of unilateral isthmic spondylolysis with lamina fracture in an athlete: case report and literature review. Am J Sports Med 33: 591-595.
- O'Beirne JG, Horgan JG (1988) Stress fracture of the lamina associated with unilateral spondylolysis. Spine (Phila Pa 1976)13: 220-222.
- Hu SS, Tribus CB, Diab M, Ghanayem AJ (2008) Spondylolisthesis and spondylolysis. Instr Course Lect 90: 656-671.
- Ariyoshi M, Nagata K, Sonoda K, Hiraoka K, Kubo M, et al. (1999) Spondylolysis at three sites in the same lumbar vertebra. Int J Sports Med 20: 56-57.
- Gunzburg R, Fraser RD (1991) Stress fracture of the lumbar pedicle. Case reports of "pediculolysis" and review of the literature. Spine (Phila Pa 1976) 16: 185-189.
- Kalideen JM, Satyapal KS, Bayat F (1994) Case report: pedicular cleft associated with bilateral pars interarticularis defects and transverse process hypoplasia of a fifth lumbar vertebra. Br J Radiol 67: 1136-1138.
- Hadley LA (1955) Bony masses projecting into the spinal canal opposite a break in the neural arch of the fifth lumbar vertebra. J Bone Joint Surg Am 37: 787-97.
- Amato M, Totty WG, Gilula LA (1984) Spondylolysis of the lumbar spine: demonstration of defects and laminal fragmentation. Radiology 153: 627-629.
- Maldague BE, Malghem JJ (1976) Unilateral arch hypertrophy with spinous process tilt: a sign of arch deficiency. Radiology 121: 567- 574.
- Sherman FC, Wilkinson RH, Hall JE (1977) Reactive sclerosis of a pedicle and spondylolysis in the lumbar spine. J Bone Joint Surg Am 59: 49-54.
- Kakiuchi M (1997) Repair of the Defect in Spondylolysis. Durable Fixation with Pedicle Screws and Laminar Hooks. J Bone Joint Surg Am 79: 818-825.
- Buck JE (1970) Direct repair of the defect in spondylolisthesis : preliminary report. J Bone Joint Surg Br 52 : 432-437.
- Scott JHS (1987) The Edinburgh repair of isthmic (Group II) spondylolysis. J Bone Joint Surg Br 69: 491.
- Kimura M (1968) [My method of filing the lesion with spongy bone in spondylolysis and spondylolistesis]. Seikei Geka 19: 285-296.
- Deguchi M, Rapoff AJ, Zdeblick TA (1999) Biomechanical comparison of spondylolysis fixation techniques. Spine (Phila Pa 1976) 24: 328-333.
- Yamashita K, Sakai T, Takata Y, Tezuka F, Manabe H, et al. (2019) Low Back Pain in Adolescent Athletes: Comparison of Diagnoses Made by General Orthopedic Surgeons and Spine Surgeons. Int J Spine Surg 13: 178-185.
- Chan AK, Sharma V, Robinson LC, Mummaneni PV (2019) Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg Clin N Am 30: 353-364.
Citation: Meves R, Silber Caffaro MF, Pellegrino LN, de Mendonça RGM (2019) Unilateral Spondylolysis and Contralateral Lamina Fracture in a Professional Soccer Player: Surgical Treatment without Arthrodesis- Case Report and Literature Review. Sport Med Inj Care 1: 004.
Copyright: © 2019 Robert Meves, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Journal Highlights
© 2026, Copyrights Herald Scholarly Open Access. All Rights Reserved!
