
A New Corneal Remodeling Technique with Laser Asymmetric Keratectomy Using Semi-Cylindrical Ablation Pattern Reducing Regional Asymmetry of Corneal Thickness, Case Series
*Corresponding Author(s):
Byung Moo MinWoori Eye Clinic, Affiliated Clinical Professor To Department Of Ophthalmology, Yonsei University School Of Medicine, Seo Ku, Daejon 35229, Republic Of Korea
Tel:+82 424761675,
Fax:+82 424761670
Email:bmin8275@naver.com
Abstract
Laser asymmetric keratectomy using semi-cylindrical ablation pattern (LAK-SCAP) is a new customized corneal remodeling method reducing regional asymmetry of corneal thickness, so could be to avoid and treat conventional laser refractive surgery adverse effects. Three eyes (3 patients) had laser epithelial keratomileusis (LASEK) linked LAK-SCAP (L-LAK-SCAP) to reduce regional asymmetry of corneal thickness and correct refractive errors. On Orbscan map, the cones of the corneas were located in the peripheral side, the corneal thickness imbalance was severe due to the sum of 4 direction differences in corneal thickness >80µm. So, they had asymmetric cornea with irregular astigmatism. L-LAK-SCAP were performed in two stages of ablation. First, after ascertaining the deviations in central symmetry based on the Vision-Up program, the deviations were eliminated. The corneal curvature, which shows myopic shifts due to the corneal ablation procedure with LAK-SCAP, can be predicted by the Vision-Up program. Thus, additional ablation for a myopic shift and ablation for original refractive errors were performed simultaneously to ensure that the first procedure did not cause a myopic shift. On pre and postoperative one year, spherical equivalent (SE), sphere, cylinder, uncorrected distance visual acuity (UDVA), topographic changes, pupil size, angle kappa, CCT corneal irregularities, the sums of 4 direction corneal thickness deviation (SUM), and distance between the optic axis and the apex of the posterior cornea (DISTANCE) were compared. SE, sphere, CCT, SUM, DISTANCE was markedly decreased postoperatively. Cylinder, pupil size, angle kappa, corneal irregularities were similar between pre- and post-L-LAK-SCAP. The Thinnest point (cone) was located closely in the center of cornea. UDVA also markedly increased postoperatively. There were no complaints in blurring postoperatively LAK-SCAP reduces corneal thickness deviations and aligns the visual axis, improving vision, so makes a new corneal remodeling of symmetry.
Keywords
Corneal remodeling; Deviations in corneal thickness (µm) in four directions based on Orbscan maps; Laser asymmetric keratectomy using semi-cylindrical ablation pattern (LAK-SCAP); Regional asymmetry of corneal thickness
Introduction
Myopic regression or decrease in visual acuity and ocular discomfort has been reported following laser refractive surgery (LRS) [1-5].
Conventional corneal refractive correction methods that focus only on correcting refractive abnormalities are unable to prevent corneal deformation because of the interaction between the intraocular pressure and corneal thickness in patients with a large deviation in corneal thickness, showing asymmetric corneas. Therefore, it has been suggested that only new customization methods could prevent postoperative corneal deformation [6-14]. The corneal shape is determined by a complex interaction between its biomechanical properties, such as corneal thickness and stiffness and intraocular pressure [6,7,13,14]. In this regard, recent research [15-21] has focused on postoperative adverse effects in patients with a large sum of deviation in corneal thickness in 4 directions ≥80µm preoperatively. In the patients with large deviation in corneal thickness (≥80µm), corneal asymmetry, higher blurring scores, lower uncorrected distance visual acuity, and lower efficiency index were shown postoperatively [16,17,21] but in cases of a decreasing sum of total deviation in corneal thickness with asymmetric corneal ablation (from ≥80µm to <80µm), adverse effects were markedly decreased postoperatively [16-21]. Thus, corneal thickness deviation is considered an important factor of corneal asymmetry and a cause of visual abnormalities such as blurring of vision, visual aberrations, and dry eye [15-21].
Recent studies have suggested laser asymmetric keratectomy (LAK) [15-21] as a method for biomechanical customization. It helps achieve central corneal symmetry with a central point, and such improved corneal morphology is maintained long-term without deterioration of the cornea [15-21].
In these case reports, we aimed to present the results of a new corneal remodeling technique with LAK-SCAP reducing regional asymmetry of corneal thickness.
Case Report
This study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 1983 and was approved by the Korean National Institute for Bioethics Policy (approval number: P01-202101-21-009). All patients provided written informed consent.
Patients’ age was 19 to 38 years old, two male and one female. All were left eyes (Table 1). UDVA (LogMAR) were 0.3-1.0 refraction of the eyes (spherical equivalent, SE) and cylinder were from -0.75 to -3.50 diopters measured using an auto refractokeratometer and the intraocular pressure measured with a non-contact tonometer were 14-16 mmHg (Table 2). The other ocular findings including retina were fine. For pre and post operative corneal thickness deviation [15-17], the thickness (µm) was measured at 8 points corresponding to the direction angles (0º, 45º, 90º, 135º, 180º, 225º, 270º, and 315º) at a distance of 2.5 mm from the centre of the cornea. The differences in thickness between symmetrically opposed points (0–180º, 45–225º, 90–270º, and 135–315º) were calculated, and the sum of these differences in 4 directions (SUM) was used in the analysis (Figures 1 and 2). The distance [15-21] between the maximum posterior elevation (best-fit-sphere) and the visual axis (DISTANCE) was checked by conversion to the distance between the X and Y coordinates of the thinnest point and the centre of the cornea on an Orbscanmap (Figures 1 and 2). The cones of the left eye cornea were located in the peripheral side. The corneal thickness imbalance was severe in the left eyes due to SUM >80 µm (151µm in case 1, 167 µm in case 2, and 151µm in case 3) (Figure 1). The corneal irregularities (diopters) in the 3.0-mm and 5.0-mm zone on the Orbscan maps were 0.9, 1.2 diopters in case 1, 1.4, 1.8 diopters in case 2, and 1.6, 2.0 diopters in case 3 in the preoperative L-LAK-SCAP. The central corneal thickness was 582µm in case 1, 497 µm in case 2, and 507µm in case 3, the pupil diameter was3.9 to 5.1 mm, the Kappa angles were 3.73° in case 1, 8.84° in case 2, and 5.16° in case 3 (Table 2).
|
Item |
Case 1 |
Case 2 |
Case 3 |
|
Age (year) |
21 |
38 |
19 |
|
Sex |
M |
F |
M |
|
R/L |
L |
L |
L |
Table 1: Preoperative patient’s categories.
M: Male; F: Female; L: Left; R: Right
|
Item |
Pre-L-LAK-SCAP |
Post-L-LAK-SCAP |
||||
|
Case 1 |
Case 2 |
Case 3 |
Case 1 |
Case 2 |
Case 3 |
|
|
SE (diopters) |
-2.38 |
-1.75 |
-3.50 |
0.50 |
0.00 |
0.50 |
|
Sphere |
-2.00 |
-1.75 |
-3.50 |
+0.25 |
0.00 |
0.00 |
|
Cylinder |
-0.75 |
0.00 |
0.00 |
-0.50 |
0.00 |
0.00 |
|
UDVA (Log MAR) |
1 |
0.3 |
1 |
0 |
0.00 |
0.00 |
|
IOP (mmHg) |
14 |
16 |
15 |
15 |
14 |
15 |
|
Pupil size (mm) |
3.9 |
5.1 |
5.1 |
3.8 |
5.3 |
5.3 |
|
Angle kappa (degree) |
3.73 |
8.84 |
5.16 |
6.24 |
7.70 |
4.67 |
|
CCT (mm) |
582 |
497 |
507 |
462 |
392.00 |
424.00 |
|
Corneal irregularities (diopters) on Orbscan |
||||||
|
In 3.0mm-zone |
0.9 |
1.4 |
1.6 |
2.4 |
2.0 |
1.9 |
|
In 5.0mm-zone |
1.2 |
1.8 |
2.0 |
2.9 |
2.4 |
2.1 |
|
SUM (micron) |
151 |
167 |
151 |
29 |
59 |
49 |
|
DISTANCE (mm) |
0.4 |
0.4 |
0.3 |
0.1 |
0.3 |
0.1 |
Table 2: Pre and Postoperative findings.
SE: Spherical Equivalent; BFS: Best-Fit-Sphere; L- LAK-SCAP: Laser Epithelial Keratomileusis (LASEK) linked laser asymmetric keratectomy using Semi-Cylindrical Ablation Pattern; UDVA: Uncorrected Distance Visual Acuity; IOP: Intraocular Pressure; CCT: Central Corneal Thickness; LogMAR: Logarithm of the Minimum Angle of Resolution; Corneal irregularity: Corneal irregularity (diopters) in the 3.0 mm zone on Orbscan maps; SUM: Sum of deviations in corneal thickness in 4 directions (µm); DISTANCE: Distance (mm) between the maximum posterior elevation (BFS) and the visual axis.
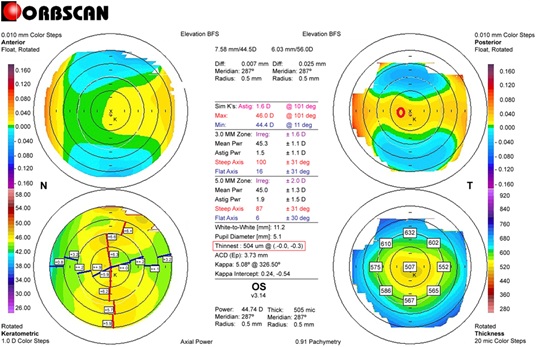 Figure 1: Preoperative Orbscan map in case 3. (The right bottom pachymetric map) An example of measuring the differences in thickness between symmetrically opposed points on pachymetricmap (0–180°, 45–225°, 90–270°, and 135–315°): 0-180°: 23µm; 45-225°: 16 µm; 90-270°: 65 µm; 135-315°: 45 µm; total: 149 µm. (The right upper map) Measuring the distance between the maximum posterior elevation (best-fit-sphere; BFS) and the visual axis. Corneal apex: temporally deviated (right upper red circle). The thinnest point (X, Y) is indicated by the lower red square.
Figure 1: Preoperative Orbscan map in case 3. (The right bottom pachymetric map) An example of measuring the differences in thickness between symmetrically opposed points on pachymetricmap (0–180°, 45–225°, 90–270°, and 135–315°): 0-180°: 23µm; 45-225°: 16 µm; 90-270°: 65 µm; 135-315°: 45 µm; total: 149 µm. (The right upper map) Measuring the distance between the maximum posterior elevation (best-fit-sphere; BFS) and the visual axis. Corneal apex: temporally deviated (right upper red circle). The thinnest point (X, Y) is indicated by the lower red square.
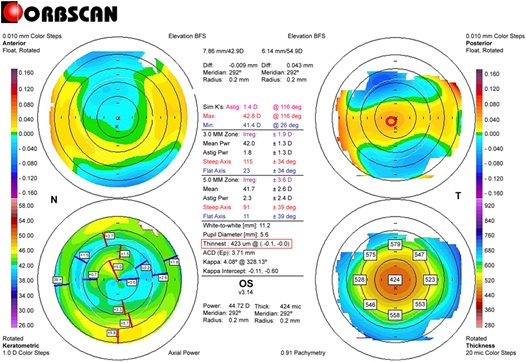 Figure 2: Postoperative Orbscan map in case 3. (The right bottom pachymetric map). An example of measuring the differences in thickness between symmetrically opposed points pachymetric map (0–180°, 45–225°, 90–270°, and 135–315°). 0–180°: 5µm, 45–225°: 1 µm, 90–270°: 21 µm, 135–315°: 22 µm, Total: 49 µm. (The right upper map) Measuring the distance between the maximum posterior elevation (best-fit-sphere; BFS) and the visual axis. Corneal apex: centrally located (right upper red circle). The thinnest point (X, Y) is indicated by the lower red square.
Figure 2: Postoperative Orbscan map in case 3. (The right bottom pachymetric map). An example of measuring the differences in thickness between symmetrically opposed points pachymetric map (0–180°, 45–225°, 90–270°, and 135–315°). 0–180°: 5µm, 45–225°: 1 µm, 90–270°: 21 µm, 135–315°: 22 µm, Total: 49 µm. (The right upper map) Measuring the distance between the maximum posterior elevation (best-fit-sphere; BFS) and the visual axis. Corneal apex: centrally located (right upper red circle). The thinnest point (X, Y) is indicated by the lower red square.
Therapeutic Intervention
Patients with refractive errors and SUM >80 µm underwent L-LAK-SCAP using a193-nm ISO-D200 laser (Kera Harvest Inc., Taiwan). Laser correction was performed by BM Min. Local anesthesia was induced by instillation of 0.50% propacaine hydrochloride (Alcaine, Alcon NV, Vilvoorde, Belgium); for LASEK, a 9.0–9.5-mm diameter patch of corneal epithelium was removed with a brush. For refractive correction, laser ablation was performed in the 6.0-6.2mm optic zone to correct refractive error (myopia and astigmatism).To perform L-LAK-SCAP [15-17]. we used Vision-Up software (WellC, South Korea) to analyze the corneal thickness deviations based on Orbscan II (Bausch & Lomb, Bridgewater, NJ, USA) corneal maps, and also to predict amounts of ablation on the thicker cornea, degree of axis(direction of regional ablation), number of SCAP and corneal myopic change (myopic shift) as a result of the removal of the thicker corneal regions as determined by LAK-SCAP. Figure 3 illustrates how LAK can be implemented with a cylindrical ablation pattern for conventional astigmatism correction. Figure 3a show examples of axial, symmetric images of two-partial ablation patterns. Figure 3b show examples of one-partial (semi-cylindrical) laser ablation patterns for LAK-SCAP; specifically, they show one-partial ablation for existing cylindrical ablation patterns. These patterns can be achieved by blocking laser corneal ablations at the thinner sections of the cornea. L-LAK-SCAP improved corneal symmetry by reducing the sum of corneal thickness deviations and corrected the refractive power and myopic shift due to LAK-SCAP simultaneously (Figures 2 and 4). Therefore, we were able to ablate the cornea to create central symmetry without changing the refractive errors (Figures 2, 4 and 5). In intraoperative findings, optic zones were 6.0-6.2mm, ablation depths were 39-69µm, myopic shift due to LAK-SCAP were -1.50 - -2.75 diopters, and residual stromal depth were 378-456 um (Table 3).
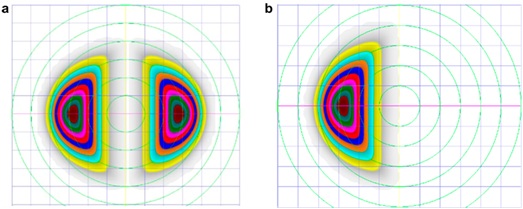 Figure 3: The schematic description of LAK-SCAP. (a) shows examples of axial, symmetric images of two-partial ablation patterns. (b) shows examples of laser ablation patterns for LAK-SCAP; specifically, it shows one partial ablation for existing cylindrical ablation patterns, as seen in (a). These patterns can be achieved by blocking laser corneal ablations at the thinner sections of the cornea.
Figure 3: The schematic description of LAK-SCAP. (a) shows examples of axial, symmetric images of two-partial ablation patterns. (b) shows examples of laser ablation patterns for LAK-SCAP; specifically, it shows one partial ablation for existing cylindrical ablation patterns, as seen in (a). These patterns can be achieved by blocking laser corneal ablations at the thinner sections of the cornea.
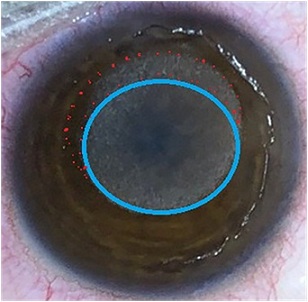 Figure 4: Ablation pattern in case 3. Purple circled round area indicated ablation pattern (totally -5.50 diopters) of both refractive error (-3.50 diopters) and myopic shift (-2.0 diopters) due to LAK-SCAP, and red dotted circled area indicated LAK-SCAP ablation of the thicker area of the cornea.
Figure 4: Ablation pattern in case 3. Purple circled round area indicated ablation pattern (totally -5.50 diopters) of both refractive error (-3.50 diopters) and myopic shift (-2.0 diopters) due to LAK-SCAP, and red dotted circled area indicated LAK-SCAP ablation of the thicker area of the cornea.
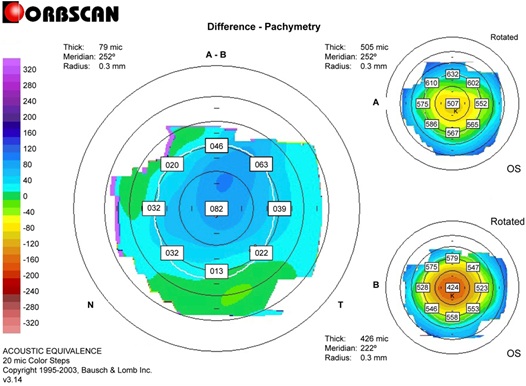 Figure 5: Differential pachymetric map between pre- and post-L-LAK-SCAP in case 3.
Figure 5: Differential pachymetric map between pre- and post-L-LAK-SCAP in case 3.
|
Item |
Case 1 |
Case 2 |
Case 3 |
|
Optic zone (mm) |
6.0 |
6.0 |
6.2 |
|
Ablation depth (µm) |
66 |
39 |
69 |
|
Myopic shift(diopters) due to LAK-SCAP |
-2.75 |
-1.50 |
-2.0 |
|
Residual stromal depth (µm) |
456 |
398 |
378 |
Table 3: Intraoperative findings.
LAK-SCAP: laser asymmetric keratectomy using semi-cylindrical ablation pattern
Follow-up and Outcome
After one year of L-LAK-SCAP in the left eyes (Table 2), UDVA in all patients were increased to 20/20 (0 in Log MAR) and refractions (SE and sphere) were within ±0.50 diopters, the axes of cylinder were not changed and similar to preoperative, and the intraocular pressure measured with a non-contact tonometer was 14-16mmHg.
According to the findings of Orbscanmap, SUM was markedly decreased to <80µm, DISTANCE also decreased postoperatively. The corneal center cone was located closely at the corneal center, and the corneal symmetry was so good (Figure 2, Table 2).
The corneal irregularities (diopters) in the 3.0-mm and 5.0-mm zone on the Orbscan maps were within 2.4 diopters and 2.9 diopters in the postoperative one year after L-LAK-SCAP. The central corneal thickness was 462µm, in case 1,392 µm, in case 2, and 424 µm, in case 3. The pupil diameter was 3.8-5.3 mm, the angle kappa was 4.67-7.70° (Table 2).There are no complaints in blurring post operatively.
Discussion
Conventional LRS methods, which only aim to correct refractive error, cannot prevent corneal changes such as myopic shift, distortion etc. as a result of postoperative changes postoperatively; as a result, the interactions between intraocular pressure, corneal stiffness, and corneal thickness are affected complications such as distorted cornea, blurring are reported in patients who have undergone PRK [6-10]. Due to the corneal thickness deviations, the thinner parts of the cornea are expected to undergo postoperative changes as a result of the intraocular pressure. For this reason, new customization methods are needed [15-21]. LAK-SCAP is a type of customization method in which the cornea is asymmetrically cut in order to eliminate deviations in the central symmetry of corneal thickness as a new corneal remodeling technique [15-21]. In the previous our study [16,17]; the 1-year postoperative spherical equivalent was similar between the LASIK (control) group and the LASIK linked LAK (comparison) group in over 80 um with SUM. However, compared to the LASIK linked LAK group, the LASIK group showed myopic regression over time after 1 postoperative year. On the other hand, because the LASIK linked LAK group showed improved corneal symmetry due to reducing peripheral asymmetry of corneal thickness, these patients are expected to show much lower rates of adverse effects due to corneal deformation in the long term. The LASIK linked LAK group showed better corneal thickness deviation and distribution as well as significantly reduced blurring compared to the LASIK group. Further, we found that the 1-year postoperative uncorrected far visual acuity was better in the LRS with LAK group than that in the LRS alone group despite similar spherical equivalents, which may be due to the effects of blur reduction, but further studies will be required. LAK-SCAP is a useful corrective method as a new corneal remodeling technique for patients who complain of adverse effects such as blurring due to corneal distortion after glaucoma or cataract surgery, as it can reduce the intraocular pressure and corneal stiffness postoperatively [8,11,15-21].
LAK-SCAP has only been reported recently [15-21]; moreover, unlike the previously reported wave front- and topography-guided LASIK or LASEK [22,23] LAK-SCAP reduces corneal thickness deviations by asymmetric corneal ablation. Further, it increases the corneal symmetry by decreasing the distance between the maximum posterior elevation (BFS) and the visual axis, and thereby, it is expected to prevent corneal changes postoperatively [15-21].
Moreover, it has been reported that LAK, which only cuts the thick parts of the cornea to create central symmetry, can be useful to reduce the effects of intraocular pressure pushing outwards on the thin parts of the cornea in keratoconus, as well as to lessen the asymmetric morphology of the cornea and to reduce the incidence of optical aberrations [9,11,12]. However, we believe that the indications for LAK-SCAP will include advanced customized refractive surgery, treatment of corneal distortions after intraocular surgery (e.g., cataract or glaucoma operations), and treatment of early keratoconus and posterior corneal ectasia.
If the cornea is symmetric, it will show good corneal refractive surgery result without long-term corneal morphologic changes, so SUM and DISTANCE are very important findings [15-21]. We used topography with Orbscan map, not current Sheimpflug techniques, Only Orbscan map can be calculated the distance between the maximum posterior elevation and visual axis, because there is a visual axis center map in Orbscan, so was very useful for measuring symmetry.
But if the cornea is asymmetric it is easy in corneal morphologic changes such as protrusion, or ectasia due to corneal thickness deviation, postoperatively the cornea were thinner, and due to the difference in thickness, the refractive power of the thinner corneal region was greater than that of the thicker region. The deviation in thickness caused refraction values to increase more than1.0diopterthroughoutthethin portions of the cornea, relative to other areas and make irregular astigmatism. As a result, the curvature of the posterior cornea became more negative. It is believed that the difference in curvature between the anterior and posterior cornea causes scattering of the incoming light through the pupil, leading to blurring. After one year of L-LAK-SCAP, in this case, SUM decreased to under 80µm, and the central corneal cone was located closely in the center of the cornea, coinciding with the visual axis. The corneal irregularities (diopters) in the 3.0-mm and 5.0-mm zone on the Orbscan maps were similar and, the central corneal thickness, and the angle kappa were decreased. So, there were no complaints in blurring and increased visual acuity.
Because LAK-SCAP is a recently developed technology, we were only able to follow up the patients for one year in only three patients; thus, more studies with longer follow up time, more than one year and with a large number of patients are warranted in the future. to investigate the outcomes including myopic regression over time.
In conclusion, LAK-SCAP is a new corneal remodeling technique to reduce regional asymmetry of corneal thickness and increase corneal symmetry and showed so good clinical outcomes.
Acknowledgment
We would like to thank Editage (www.editage.co.kr ) for English language editing.
Funding
The authors received no financial support for the research, authorship and/or publication of this article.
Conflicts of Interest
The authors declare that there is no conflict of interest.
References
- Kuo IC, Lee SM, Hwang DG (2004) Late-onset corneal haze and myopic regression after photorefractive keratectomy (PRK). Cornea 23: 350-355.
- Perez-Santonja JJ, Ayala MJ, Sakla HF, Ruíz-MorenoJ M, Alió JL (1994) Retreatment after laser in situ keratomileusis. Ophthalmology 106: 21-28.
- Holladay JT, Janes JA (2002) Topographic changes in corneal asphericity and effective optical zone size after laser in situ keratomileusis. J Cataract Refract Surg 28: 942-947.
- Pop M, Payete Y (2004) Risk factors for night vision complaints after LASIK for myopia. Ophthalmology 111: 3-10.
- Moshirfar M, Shah TJ, Skanchy DF, Linn SH, Durrie DS (2017) Meta-analysis of the FDA reported outcomes using the three latest platforms for LASIK. J Refract Surg 33: 362-368.
- Roberts S (2000) The Cornea is Not a Piece of Plastic. J Refractive Surg 16: 407-413.
- Roberts S (2005) Biomechanical customization: The next generation of laser refractive surgery. J Cataract Refractive Surg 31: 2-5.
- Roberts CJ, Dupps WJ Jr (2014) Biomechanics of corneal ectasia and biomechanical treatments. J Cataract Refract Surg 40: 991-998.
- Ortiz D, Pinero D, Shabayek MH, Arnalich-Montiel F, Alió JL (2007) Corneal biomechanical properties in normal, post-laser in situ keratomileusis and keratoconic eyes. J Cataract Refract Surg 33: 1371-1375.
- Ambrosio R Jr, Nogueira LP, Caldas DL, Fontes BM, Luz A, et al. (2011) Evaluation of corneal shape and biomechanics before LASIK. Inn Ophthalmol Clin 51: 11-38.
- Lee H, Roberts CJ, Kim TI, Ambrósio Jr R, Elsheikh A, et al. (2017) Change in biomechanically corrected intraocular pressure and dynamic corneal response parameters before and after transepithelial keratectomy and femtosecond laser-assisted laser in situ keratomileusis. J Cataract Refract Surg 43: 1495-1503.
- Osman IM, Halaly HY, Abdally M, Shousha MA (2016) Corneal biomechanical changes in eye with small incision lenticule extraction and laser assisted in situ keratomilliusis. BMC Ophthalmol 16: 123.
- Wang B, Zhang Z, Naidu RK (2016) Comparison of the change in posterior corneal elevation and corneal biomechanical parameters after small incision lenticule extraction and femtosecond laser-assisted LASIK for high myopia correction. Cont Lens Anterior Eye 39: 191-196.
- Wang D, Liu M, Chen Y, Zhang X, Xu Y, et al. (2014) Differences in the corneal biomechanical changes after SMILE and LASIK. J Refract Surg 30: 702-707.
- AgudoJAR, Park J, Park J, Lee S, Park K (2019) Laser asymmetric ablation method to improve corneal shape. Lasers Med Sci 34: 1763-1779.
- Min JS, Min BM (2021) Comparison of outcomes of laser refractive surgery (LRS) alone and LRS with laser asymmetric keratectomy in patients with myopia: A retrospective study. Medicine (Baltimore) 100: e25366.
- Min JS, Min BM (2020) Comparison between surgical outcomes of LASIK with and without laser asymmetric keratectomy to avoid conventional laser refractive surgery adverse effects. Sci Rep 10: 10446.
- Min JS, Jin LY, Min BM (2020) Early postoperative topographic changes after laser asymmetric keratectomy for the management of adverse effects after photorefractive keratectomy. J Ophthalmol Open Access 1: 1-7.
- Min JS, Min BM (2021) A novel approach to enhancement linked laser asymmetric keratectomy using semi-cylindrical ablation pattern in patients with myopic regression after laser refractive surgery. Clin Ophthalmol 15: 1751–1758.
- Min JS, Min BM (2021) Clinical outcomes of laser asymmetric keratectomy to management postoperative adverse effects-A retrospective clinical trial. The Open Opthalmol J 15: 171-177.
- Min JS, Min BM, Lee DC (2021) Laser asymmetric keratectomy using a semi-cylindrical ablation pattern to avoid adverse effects of laser refractive surgery. Austin J Clin Ophthalmol 8:1120.
- Chalita MR, Chavala S, Xu M, Krueger RR (2004) Wavefront analysis in post-LASIK eyes and its correlation with visual symptoms, refraction, and topography. Ophthalmology 111: 447-453.
- Jankov 2nd MR, Panagopoulou SI, Tsiklis NS, Hajitanasis GC, Aslanides IM, et al. (2006) Topography-guided treatment of irregular astigmatism with the wavelight excimer laser. J Refract Surg 22: 335-344.
Citation: Min JS, Min BM, Lee DC (2022) A New Corneal Remodeling Technique with Laser Asymmetric Keratectomy Using Semi-Cylindrical Ablation Pattern Reducing Regional Asymmetry of Corneal Thickness, Case Series. J Ophthalmic Clin Res 9: 091.
Copyright: © 2022 Ji Sang Min, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

