
Cataract Surgery in Ocular Mucous Membrane Pemphigoid: A Risk, a Benefit or Both?
*Corresponding Author(s):
Filippo ConfalonieriIRCCS Humanitas Research Hospital, Via Manzoni 56, 20089 Rozzano, Milan, Italy
Email:filippo.confalonieri01@gmail.com
#Equal Contribution and should both be considered first author
Abstract
Ocular Mucous Membrane Pemphigoid (OcMMP) is a systemic autoimmune disease characterized by scarring of orificial mucous membranes. Cataract is common because OcMMP primarily affects the elderly and drug-induced cataract may result from topical and systemic steroids. The aim of this study is to evaluate the effectiveness of phacoemulsification and Intraocular Lens (IOL) implantation in OcMMP patients. Data from 15 eyes of 10 patients affected by OcMMP that underwent phaco+IOL have been evaluated. Each patient was examined a week before surgery and at day 1, day 3, day 7 and 30 days after surgery. Visual acuity, ocular inflammation and infection signs were recorded. No eyes showed OcMMP reactivation or progression after one year of follow-up during a maintenance immunosuppressive regimen. In conclusion, performing phacoemulsification in a stable OcMMP does not expose the patient to disease progression nor reactivation.
Abbreviations
OcMMP: Ocular Mucous Membrane Pemphigoid
IOL: Intraocular Lens
Phaco+IOL: Phacoemulsification and Intraocular Lens Implant
OCP: Ocular Cicatricial Pemphigoid
MMP: Mucous Membrane Pemphigoid
OSDI: Ocular Surface Disease Index Questionnaire
IVIg: Intravenous Immunoglobulins
ECCE: Extracapsular Cataract Extraction
ICCE: Intracapsular Cataract Extraction
Introduction
Mucous Membrane Pemphigoid (MMP) is a systemic autoimmune disease characterized by scarring of orificial mucous membranes such as the conjunctiva, nasal cavity, oropharynx, and genitalia. Ocular involvement occurs in about 70% of all MMP cases and when this happens the condition takes the name of Ocular Mucous Membrane Pemphigoid (OcMMP). The progressive inflammatory and scarring nature of MMP leads to severe visual impairment in 30% of affected eyes and bilateral blindness in 20% [1]. The older term Ocular Cicatricial Pemphigoid (OCP) has now been replaced by ocular MMP (OcMMP) after publication of the 2002 international consensus document [1-4].
Damage in OcMMP is caused by a type II hypersensitivity reaction against the epithelial basement membrane of the conjunctiva. Although distinct subgroups of MMP have been identified by use of advanced immunopathologic and immunochemical techniques, diagnosis should still be made based on clinical presentation combined with pathological, immunohistological, and serum antibody analysis [5,6].
The ocular manifestations can be classified in different severity stages ranging from a chronic conjunctivitis without corneal damage or visual involvement to blindness due to corneal scarring, vascularization, and keratinization.
All the stages may be assessed using one of the two classifications system widely used: Mondino’s Classification System [7] and Foster’s Classification System [8].
Immunosuppression is the treatment of choice to control OcMMP. Topical administration is effective only as an adjunct, while the mainstay of treatment is an aggressive systemic immunosuppression [9].
Cataract is common in this kind of patients because OcMMP primarily affects the elderly and drug-induced cataract may result from topical and systemic steroids used to treat the ocular inflammation.
Cataract surgery in these patients may be challenging because of systemic and local factors:
Corneal involvement: OcMMP may cause corneal opacity, with consequent difficult access and visualization during cataract extraction.
Conjunctival fornices involvement: OcMMP may cause shortening of the fornices, symblepharon and ankyloblepharon. Some of these fornix or ciliary alterations may need a previous surgery to stabilize the palpebral function.
Reactivation: It is still debated and unclear if surgery procedures may represent a trigger to OcMMP’s reactivation. Previous studies have demonstrated that surgery performed on patients with OcMMp may be followed by increased conjunctival inflammation, rapid progression of keratopathy and conjunctival scarring, if the disease is not medically controlled [10-12].
Immunosuppressed patients: OcMMP patients are often immunosuppressed, which is a risk factor for ocular infection and endophthalmitis after cataract surgery [13].
Patients’ expectation: OcMMP is an extremely dramatic pathology. Usually, patients are already experiencing ocular discomfort lasting from several months to years and when also decreased vision becomes symptomatic, thefear of sight loss affects the patient psychologically.
Objectives
The aim of this study is to evaluate the effectiveness of cataract surgery with phacoemulsification and Intraocular Lens (IOL) implantation in OcMMP patients. To evaluate the impact of the surgical procedure on ocular surface inflammation, all patients underwent a conjunctival ultrastructure study with confocal microscopy. In addition, patients were asked to complete an ocular discomfort and pain questionnaire, the Ocular Surface Disease Index (OSDI) questionnaire, before, one month, and six months after surgery.
Materials And Methods
In this retrospective study, data from 15 eyes of 10 OcMMP patients undergoing phacoemulsification and IOL implantation at the Department of Neuroscience, Reproductive Sciences and Odontostomatology, University of Naples “Federico II” were evaluated. Patient demographics and reference data are shown in table 1. The mean age at presentation was 68.5 ± 10.5 years.
|
Case Number |
Age/Sex |
Age of onset |
Serum Investigation (IIF) |
Ocular Biopsy (DIF) |
BCVA (Decimal) |
Foster Stage |
Extraocular localization of pemphigoid |
Diagnostic Delay Time (months) |
Systemic Diseases |
|
1 |
83yo/ F |
79 |
Negative |
Positive |
RE 0.6 |
RE III |
None |
12 |
AH |
|
|
|
|
|
|
LE 0.3 |
LE III |
|
|
|
|
2 |
64yo/ M |
60 |
Positive |
Negative |
RE 1.0 |
RE II |
None |
2 |
AH |
|
|
|
|
|
|
LE 0.8 |
LE III |
|
|
|
|
3 |
59yo/ F |
58 |
Positive |
Negative |
RE 1.0 |
RE I |
Oral/Esophageal |
7 |
None |
|
|
|
|
|
|
LE 1.0 |
LE I |
|
|
|
|
4 |
65yo/ F |
62 |
Negative |
Positive |
RE 0.5 |
RE III |
None |
7 |
DM Type 2 |
|
|
|
|
|
|
LE 0.8 |
LE III |
|
|
|
|
5 |
76yo/ F |
56 |
Negative |
Positive |
RE 0.5 |
RE III |
None |
2 |
None |
|
|
|
|
|
|
LE 0.05 |
LE IV |
|
|
|
|
6 |
43yo/ F |
43 |
Negative |
Positive |
RE 0.8 |
RE III |
None |
18 |
AH |
|
|
|
|
|
|
LE 0.8 |
LE III |
|
|
|
|
7 |
72yo/ F |
64 |
Negative |
Positive |
RE 0.7 |
RE III |
Genital/Oral |
1 |
AH/ DM type 2 |
|
|
|
|
|
|
LE 0.7 |
LE III |
|
|
|
|
8 |
64yo/ F |
60 |
positive |
Negative |
RE 0.9 |
RE I |
Oral |
12 |
AH |
|
|
|
|
|
|
LE 0.9 |
LE I |
|
|
|
|
9 |
66yo/F |
55 |
Negative |
Positive |
RE 0.05 |
RE IV |
Cutaneous |
10 |
None |
|
|
|
|
|
|
LE O.O5 |
LE IV |
|
|
|
|
10 |
60yo/F |
50 |
Negative |
Positive |
RE 0.5 |
RE III |
None |
14 |
DM type 2 |
|
|
|
|
|
|
LE 0.6 |
LE III |
|
|
|
|
11 |
68yo/M |
40 |
Negative |
Negative |
RE 0.7 |
RE III |
Cutaneous |
48 |
DM type 1 |
|
|
|
|
|
|
LE 0.05 |
LE IV |
|
|
|
|
12 |
62yo/M |
55 |
Negative |
Positive |
RE 0.6 |
RE III |
Oral, skin, esophageal |
10 |
AH |
|
|
|
|
|
|
LE 0.6 |
LE III |
|
|
|
|
13 |
60yo/M |
57 |
Negative |
Positive |
RE 0.7 |
RE III |
Nose, oral |
6 |
AH |
|
|
|
|
|
|
LE 0.7 |
LE III |
|
|
|
|
14 |
72yo/F |
66 |
Negative |
Positive |
RE 0.9 |
RE I |
Oral |
4 |
AH |
|
|
|
|
|
|
LE 0.9 |
LE I |
|
|
|
|
15 |
60yo/F |
58 |
Negative |
Positive |
RE 0.7 |
RE I |
None |
20 |
None |
|
|
|
|
|
|
LE 0.7 |
LE II |
|
|
|
Table 1: Demographical data.
The diagnosis of OcMMP was made according to the diagnostic criteria of the International Consensus on Mucous Membrane Pemphigoid [4]. Each patient underwent a series of multidisciplinary examinations consisting of haematological, ophthalmological, odontostomatological and dermatological evaluations for the entire follow-up period, to evaluate systemic immunomodulation therapy, clinical response, and disease-related complications. This was done weekly, every 15 days or monthly, based on their clinical condition.
The exclusion criteria included the coexistence of other ophthalmological diseases such as glaucoma or maculopathy, to better evaluate the efficacy of phacoemulsification on visual rehabilitation. Cataract surgery was only proposed after disease remission was achieved. Ocular and perioperative data are shown in table 2.
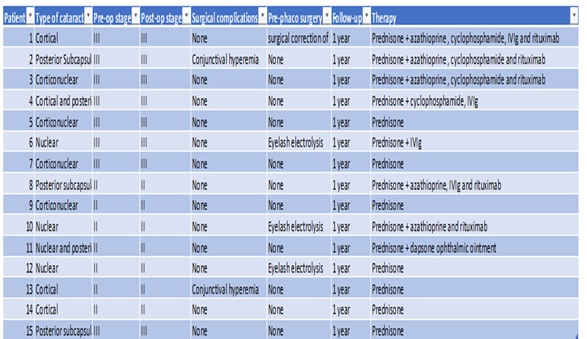 Table 2: Ocular and perioperative data.
Table 2: Ocular and perioperative data.
Stable OcMMP was defined as absence of signs of new conjunctival or corneal inflammation lasting for at least one year, stability of at least one year of clinical signs of OcMMP (shortening of the fornix and symblepharon) demonstrated with serial slit-lamp photos, absence of trichiasis or malposition of the eyelids.
For those patients who had a reduction in fornix depth that made placement of an eyelid speculum difficult, a 2/0 intratarsal silk suture was used to stabilize the eyelid during the surgical procedure.
Each patient was examined one week before surgery and on day 1, day 3, day 7 and 30 days after surgery. Subsequently, they were checked monthly. Visual acuity, eye inflammation and signs of infection were recorded.
In vivo confocal scanning laser microscopy was performed on all subjects with a new generation confocal microscope, the Rostock Corneal Software Version 1.2 of the Heidelberg RetinaTomographII (RCM/HRT II; Heidelberg Engineering GmbH, Heidelberg, Germany). The objective of the microscope was an immersion lens covered by a polymethylmethacrylate cap (Tomo-Cap; Heidelberg Engineering GmbH). Comfort gel (Bausch&; LombGmbH, Berlin, Germany) was used as a coupling agent between the applanating lens cap and theconjunctiva.
Conjunctival image analysis was taken from the three best focused images from the conjunctival epithelium. These were selected for inflammatory cell counting: the cells were manually marked inside the frame, and the inflammatory cell densities were calculated automatically by the software installed in the machine.
Phacoemulsification was performed as routine with a clear corneal multiplanar incision of 2.8 mm and a hydrophobic acrylic foldable IOL inserted in the bag.
The first line treatment for all “high-risk” patients was a “conventional” approach using steroids (prednisone 1-1,5 mg/kg/day tapered to 0.5-1 mg/kg/day after clinical remission was obtained) plus a steroid-sparing agent (Figure 1). Cyclophosphamide (from 50 mg to 200 mg daily) was the best association choice followed by azathioprine (from 100 mg to 150 mg/day) according to the patients’ systemic condition. When conventional therapy had no efficacy, or in patients with contraindications or with related side effects, patients were treated with intravenous immunoglobulins (IVIgs) and/or monoclonal anti B cell CD20+ antibodies (Rituximab) [14-16].
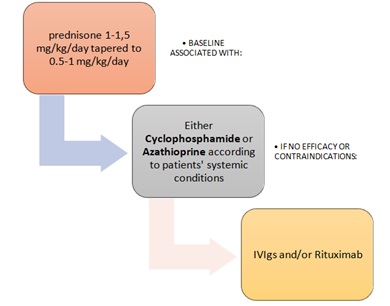 Figure 1: Flowchart immunomodulation.
Figure 1: Flowchart immunomodulation.
No preoperative modifications in systemic therapy were implemented.
Postoperatively all patients continued their systemic medication and in addition used a topical antibiotic (chloramphenicol) and steroid (dexamethasone 0.1%) four times daily for seven days.
After surgery, all patients continued systemic therapy and used a topical antibiotic (chloramphenicol) and a steroid (0.1% dexamethasone) four times a day for seven days.
Results
No intraoperative complications were reported.
For two patients (number 4 and 6) in which the inferior fornix was obliterated, a previous inferior eyelid surgery (buccal autologous mucous transplantation with inferior fornix reconstruction and ciliary electrolysis) was necessary to facilitate the positioning of eyelid retractors during cataract extraction.
At 1 month follow up, mean best corrected visual acuity (BCVA) improvement was 0.32 ± 0.17 logMAR. This value remained the same after a follow up of 18 months (Table 3).
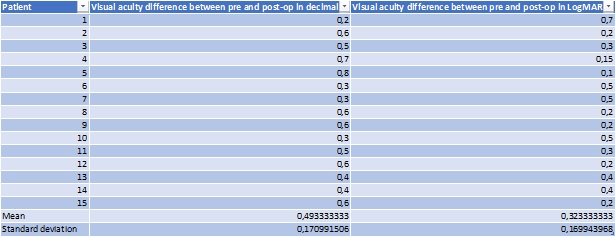 Table 3: Vision in logMar.
Table 3: Vision in logMar.
Two patients underwent YAG laser capsulotomy for posterior capsular opacification.
No eye showed reactivation or progression of OcMMP after one year follow up while on a maintenance immunosuppressive regime.
In two patients out of 10 (cases n. 1 and 2) therapy was modified: patient 1 experienced pain in the fellow (not operated) eye after one year and rituximab was added. Patient 2 started on her own cyclosporine eyedrops because of conjunctival redness. In both patients neither reduction of visual acuity nor disease progression was recorded in the operated eye. The other patients maintained the current therapeutic regimen.
The mean inflammatory cell densities in the confocal scan of normal subjects were 256. The meaninflammatory cell densities in the confocal scan of patients with OcMMP were 1,037 cells/mm2.
The mean OSDI questionnaire showed a mild mean increase in subjective ocular discomfort symptoms (mean score went from 23 to 27). These symptoms though got better after six months, reaching the pre-operative score (mean score from 27 to 21).
Discussion
A chronic, recurrent conjunctivitis accompanied by subepithelial scarring may be the first clinical sign of OcMMP. Nevertheless, the mean duration of symptoms prior to diagnosis is 2.8 years, so that the patients are often diagnosed at an advanced stage of disease [11].
Today many new therapies have been successfully tested in OcMMP with some effectiveness, so that life expectation has improved. Moreover, the quality of life improved and such patients often required a better vision quality as they develop senile or drug induced cataract.
For this reason, cataract in OcMMP patients represents an increasing management challenge for ophthalmologists.
Reports dealing with the management of cataract extraction are scarce and only three previous studies reported outcome data in OcMMP patients.
One study, published by Foster et al., [11], reported data of cataract surgery in 20 OcMMP patients (26 eyes) with biopsy-proven cicatricial pemphigoid. Preoperative medical regimens included dapsone alone (8 patients), azathioprine alone (5 patients), cyclophosphamide alone (2 patients), or a combination of drugs (5 patients). 24 of the 26 eyes had conjunctival inflammation indices of 0. Two eyes had mild inflammation. Surgery was performed using standard techniques of extracapsular cataract extraction. The disease stage did not change in any patient. Chemotherapeutic regimens remained unchanged in 15 patients. The conjunctival inflammation and conjunctival cicatrization indices were stable as compared with preoperative values in all but one patient. Keratopathy index worsened in three patients. A corneal ulcer developed in two patients. Visual acuity improved an average of 3 Snellen lines (range, -1 to 9). Two patients had unchanged vision compared with preoperatively because of retinal disease or severe keratopathy.
Another study (Geerling, Dart et al., [10]) reported outcomes of cataract surgery in 15 eyes of 13 patients, using different techniques of cataract extraction: intracapsular (ICCE) in 1, extracapsular (ECCE) in 4 and phacoemulsification in 10 eyes. In most patients, disease control required continuous treatment with one, and often two, systemic immunosuppressives with or without additional topical steroids. The aim of the preoperative treatment was to reduce and control inflammation as much as possible. Postoperatively all patients continued their systemic medication and in addition used a topical. In the first 3 months after operation no progression of the cicatricial process as assessed by the Foster staging occurred. However, during the further follow-up three operated and two unoperated eyes progressed by one stage. The progression of the disease did not depend on the type of cataract operation.
Another study again (Charuta et al. [12]) reported encouraging results in 8 patients (4 ECCEs and 4 phacoemulsifications) with disease progression in 2 of 9 eyes, both eyes were from the same patient which underwent Extracapsular Cataract Extraction (ECCE) procedure and progressed 3 months after surgery, despite maximum conventional systemic therapy. The authors found no statistical association between type of surgery and OcMMP reactivation and did not find correlation between neither preoperative OcMMP activity nor OcMMP stage with the eventual increased risk of disease progression. In this study a common use of preoperative immunosuprression lacked for the patients enrolled and systemic immunosuppressive was recommended on the base of OcMMP severity and rate of disease progression. We do agree with the author that the larger incision used for ICCE or ECCE usually requires suturing, resulting in irritation or precipitation of conjunctival inflammation.
In our cases, the surgical procedure was exclusively phacoemulsification with a clear corneal incision. It is emphasized that in two patients it was necessary to perform a previous conjunctival surgery to correct entropion or cicatricial trichiasis. In both cases the surgery was performed before cataract extraction and in both cases no progression of the disease was recorded even afterphacoemulsification (both were studied for one year of follow up from eyelid surgery to cataract).
Our pre-intervention strategy was based on OcMMP activity. In all enrolled patients, disease remission was first achieved with induction immunosuppressive therapy. Then the lowest effective dose was reached to perform surgery in a condition of minimal immunosuppression.
Enrolled patients were in an inactive phase of disease, defined as the absence of conjunctival inflammation or fornix changes for at least one year. This may explain why ours is the first study in which there is no reactivation of OcMMP after phacoemulsification.
This is the first study using IVIg and/or Rituximab therapy to achieve disease remission prior to phacoemulsification. It can be speculated that this is the reason for the high success rate. With the introduction of IVIg and/or Rituximab a better control of the pathology is possible in refractory patients, so we consider them mandatory prior to surgery if a good control of the disease is not achieved.
Immunomodulation balance is a crucial point in OcMMP cataract surgery. We think that one year of absence of disease activity is a reasonable time to consider the OcMMP as stable [13].
No operated patient showed disease progression after one year of follow-up; moreover, very few changes were made to the previously set postoperative immunosuppressive therapy.
Confocal microscopy is a useful tool for in vivo assessment of the histopathology of many ocular surface diseases and has been reported as an efficient tool for quantitative assessment of conjunctival inflammation. The density of inflammatory cells assessed by confocal microscopy is significantly correlated with the degree of inflammation of the conjunctiva.
In all operated eyes there was an initial increase in mean inflammatory cell density of 456 at the first postoperative checkup one week after surgery. In all cases this parameter returned to the preoperative baseline value, in accordance with the assessment of the conjunctival OcMMP stage at one month, as reported in the figure 2 histogram chart.
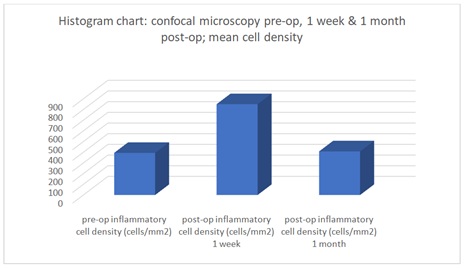 Figure 2: Histogram Chart.
Figure 2: Histogram Chart.
To the best of our knowledge, this is the most complete case series using phacoemulsification in cataract surgery and this study differs from the previous ones for the systemic treatments used (rituximab and / or IVIg).
The limitations of this study are that no data are available on the efficacy of phacoemulsification in patients with active OcMMP. Since OcMMP is a rare disease, a larger sample of patients may be needed to corroborate the current findings. This study was carried out with a retrospective design with multiple recorders of data andrandomized clinical trials (cohort study) are recommended to support current findings.
Conclusion
In conclusion, our study has found no contraindications to phacoemulsification for cataract surgery in patients with OcMMP if first stabilized by immunosuppression as clinically determined. We found no evidence of disease reactivation or progression after surgery.
Declarations
Ethics approval and consent to participate: Not applicable.
Consent for publication: Not applicable.
Availability of data and material: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Disclosure: The authors have no relevant financial or nonfinancial relationships to disclose.
Funding: None.
Author’s contribution: FC and RP equally contributed to data collection, revision, writing and data analysis so both should be considered fist author. SL contributed to patient care, data collection and revision. PV supervised the entire work. All authors read and approved the final manuscript.
Acknowledgements: None
References
- Dart JK (2017) The 2016 Bowman Lecture Conjunctival curses: scarring conjunctivitis 30 years on. Eye 31: 301-332.
- Williams GP, Radford C, Nightingale P, Dart JK, Rauz S (2011) Evaluation of early and late presentation of patients with ocular mucous membrane pemphigoid to two major tertiary referral hospitals in the United Kingdom. Eye 25:1207-1218.
- Georgoudis P, Sabatino F, Szentmary N, Palioura S, Fodor E, et al. (2019) Ocular Mucous Membrane Pemphigoid: Current State of Pathophysiology, Diagnostics and Treatment. Ophthalmol Ther 8: 5-17.
- Chan LS, Ahmed AR, Anhalt GJ, Bernauer W, Cooper KD, et al. (2002) The first international consensus on mucous membrane pemphigoid: definition, diagnostic criteria, pathogenic factors, medical treatment, and prognostic indicators. Arch Dermatol 138: 370-379.
- Xu HH, Werth VP, Parisi E, Sollecito TP (2013) Mucous membrane pemphigoid. Dent Clin North Am 57: 611-630.
- Bose T (2019) Role of immune cells in the ocular manifestations of pemphigoid diseases. Ther Adv Ophthalmol 11: 2515841419868128.
- Mondino BJ, Brown SI (1981) Ocular cicatricial pemphigoid. Ophthalmology 88: 95-100.
- Foster CS, Wilson LA, Ekins MB (1982) Immunosuppressive therapy for progressive ocular cicatricial pemphigoid. Ophthalmology 89: 340-353.
- Santi CG, Gripp AC, Roselino AM, Mello DS, Gordilho JO, et al. (2019) Consensus on the treatment of autoimmune bullous dermatoses: bullous pemphigoid, mucous membrane pemphigoid and epidermolysis bullosa acquisita - Brazilian Society of Dermatology. An Bras Dermato l94: 33-47.
- Geerling G, Dart JK (2000) Management and outcome of cataract surgery in ocular cicatricial pemphigoid. Graefes Arch Clin Exp Ophthalmol 238: 112-118.
- Sainz de la Maza M, Tauber J, Foster CS (1988) Cataract surgery in ocular cicatricial pemphigoid. Ophthalmology 95: 481-486.
- Puranik CJ, Murthy SI, Taneja M, Sangwan VS (2013) Outcomes of Cataract Surgery in Ocular Cicatricial Pemphigoid. Ocular Immunology and Inflammation 21: 449-454.
- Georgoudis P, Sabatino F, Szentmary N, Palioura S, Fodor E, et al. (2019) Ocular Mucous Membrane Pemphigoid: Current State of Pathophysiology, Diagnostics and Treatment. Ophthalmol Ther 8: 5-17.
- Ahmed AR (2004) Treatment of autoimmune mucocutaneous blistering diseases with intravenous immunoglobulin therapy. Expert Opin Investig Drugs 13: 1019-1032.
- Sami N, Letko E, Androudi S, Daoud Y, Foster CS, et al. (2004) Intravenous immunoglobulin therapy in patients with ocular-cicatricial pemphigoid: a long-term follow-up. Ophthalmology 111: 1380-1382.
- Schmidt E, Seitz CS, Benoit S, Bröcker EB, Goebeler M (2007) Rituximab in autoimmune bullous diseases: mixed responses and adverse effects. Br J Dermatol 156: 352-356.
Citation: Confalonieri F, Piscopo R, Leuci S, Vinciguerra P (2021) Cataract Surgery in Ocular Mucous Membrane Pemphigoid: A Risk, a Benefit or Both? J Ophthalmic Clin Res 8: 089.
Copyright: © 2021 Filippo Confalonieri, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

