Factors Associated with Non-Adherence to Antiretroviral Treatment in Adults at Keetmanshoop District State Hospital in Namibia
*Corresponding Author(s):
Bethabile Lovely DolamoDepartment Of Health Studies, University Of South Africa, Theo Van Wijk Building, Preller Street, UNISA, South Africa
Tel:+27 8849553218,
Email:dolamobethabilelovely@gmail.com
Abstract
Methods: Quantitative and qualitative approaches were employed, study sample of 112 adults aged 21 years and older at Keetmanshoop District State Hospital participated. Adherence to ART was assessed using the pill count and self-report methods. A questionnaire with a Cronbach value of 0.8 was used. Census and multi-stage sampling was applied. Data was collected from August to September 2016 through structured interviews and patients records review. Correlation of variables was done to remove multicollinearity. Stata version 12 was used for logistic regression to do univariate and multivariate analysis to determine factors associated with missing five or more doses.
Results: In the univariate analysis the following factors were associated with missing five or more doses: Viral load OR: 5.6, 95%CI: 2.0-16.0, Employment OR: 3.3, 95%CI: 1.5-7.2, Taking active substance OR: 2.5, 95%CI: 1.3-4.7 and Emotional status OR: 1.6, 95%CI: 1.02-2.6. The ART stocks seemed adequate as the OR for out of stock did not lead to missed doses (OR: 0.6, 95%CI: 0.4-0.9). Factors such as gender, education, religion and marital status were not associated with missing five or more doses. After multivariate logistic regression the following factors were associated with missing five or more doses; Taking substance adjusted OR: 3.3, 95%CI: 1.4-7.6; WHO clinical stages 2 and 3 adjusted ORs and 95%CIs: 4.1 (1.2-13.8) and 6.1(1.5-25.1) respectively and viral load adjusted OR: 6.3, 95%CI: 2.1-18.7. Reasons mentioned by respondents for missed doses included forgetting, alcohol use, poor access to care, work commitments, lack of food, stress and travelling. Of the 112 respondents in the study, 86.6% had unsuppressed viral loads.
Conclusion: Recommendations includes reinforcing use of reminders, automated SMS, establishing treatment supporters and collaborative efforts in reducing active substance use to improve patient adherence.
Keywords
BACKGROUND
Focusing on the study site, in January 2015, the Keetmanshoop Hospital had 1289 adults receiving ART. On average, the clinic serves about 250 to 400 patients in a month. In the period October to December 2014 a total of 933 patients received follow-up care at the study site. Of these patients 53% (n=530) achieved required adherence scores of more than or equal to 95% while approximately 47% (n=403) achieved less than the required 95%. The suboptimal adherence rate in 47% of the patients 36.7% found in January 2015 at the Keetmanshoop Hospital was significantly higher than that reported in the Northern parts of the country. The Health Belief Model (HBM) was the theory of choice in this study due to its applicability to patient adherence and preventative health practices. The HBM has four major components [6,7].
Perceived susceptibility
Perceived benefits and Costs
Motivation
Enabling or modifying factors
RESEARCH METHODS
Population
Target population
Sampling methods
The sample was insufficient and needed additional participants. These were added using review of records method as indicated in the flow chart below figure 2.
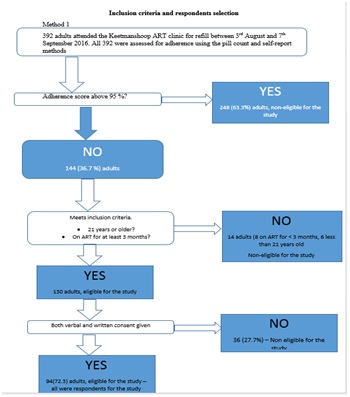
Figure 1: Method 1 sampling procedure.
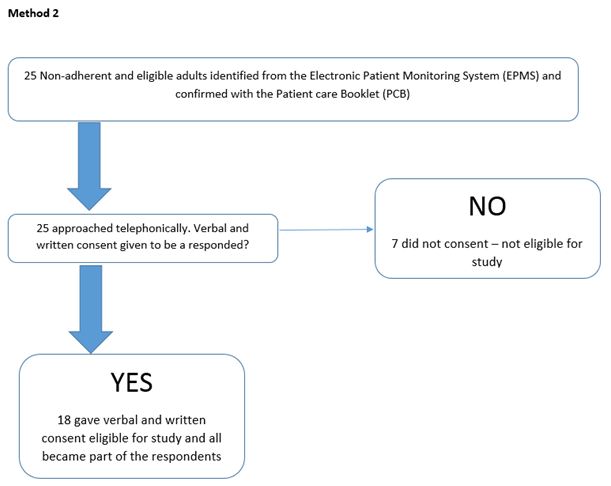
Altogether 112 adults gave a written consent to participate in the study and these made up the study sample.
Data collection approach and method
Development and testing of the data collection instrument
Data collection process
Data analysis
RESULTS
|
Patient Characteristics |
Coding Categories |
Number (%) |
|
Sex |
Male |
49 (43.8%) |
|
Female |
63 (56.3%) |
|
|
Age in completed years |
21-30 |
18 (16.1%) |
|
31-45 |
61 (54.5%) |
|
|
46-64 |
31 (27.7%) |
|
|
65 and above |
2 (1.8%) |
|
|
Ethnicity |
Nama-Damara |
53 (47.3%) |
|
Oshiwambo |
53 (47.3%) |
|
|
Caprivian/Okavango |
5 (4.5%) |
|
|
Otjiherero |
1 (0.9%) |
|
|
Religion |
Catholic |
30 (26.7%) |
|
Orthodox |
63 (56.3%) |
|
|
Protestant |
19 (17%) |
|
|
Islam |
0 |
|
|
Hindu |
0 |
|
|
African tradition |
0 |
|
|
Marital status |
Unmarried |
80 (71.4%) |
|
Married |
25 (22.3%) |
|
|
Separated/Divorced |
5 (4.5%) |
|
|
Widow or widower |
2 (1.8%) |
|
|
Level of education |
Illiterate |
6 (5.4%) |
|
Basic education |
73 (65.2%) |
|
|
Elementary education |
5 (4.5%) |
|
|
College diploma and above |
2 (1.8%) |
|
|
Living condition |
Living alone |
16 (14.3%) |
|
Living with family |
79 (70.5%) |
|
|
Living with friend |
6 (5.4%) |
|
|
Living with others |
11 (9.8%) |
|
|
Source of support |
Self-support |
65 (58%) |
|
Families |
36 (32.1%) |
|
|
NGOS |
7 (6.3%) |
|
|
No support |
4 (3.6%) |
|
|
Current employment status |
Employed |
55 (49.1%) |
|
Unemployed |
57 (50.9%) |
The outcomes of correlation of variables using logistic regression to do univariate and multivariate analysis are shown below in table 2.
|
Variable |
OR |
95% CI |
|
Gender |
2.142 |
0.970-4.734 |
|
Age group* |
1.104 |
0.642-1.909 |
|
Ethnicity |
0.673 |
0.361-1.252 |
|
Religion |
0.601 |
0.330-1.095 |
|
Marital status |
1.281 |
0.723-2.271 |
|
Education |
0.989 |
0.574-1.075 |
|
Living conditions |
0.835 |
0.500-1.394 |
|
Viral load |
5.656 |
2.00-15.96* |
|
Employment |
3.254 |
1.463-7.235* |
|
ART essential |
0.931 |
0.482-1.797 |
|
Comfortable taking ART |
0.842 |
0.563-1.260 |
|
Active substance |
2.484 |
1.142-5.405* |
|
Takes substance |
2.516 |
1.338-4.730* |
|
Disclose to community |
1.855 |
0.783-4.395 |
|
Emotional status |
1.623 |
1.022-2.578* |
|
ARV remind HIV |
1.356 |
0.788-2.334 |
|
Convenient clinic |
1.576 |
0.964-2.576 |
|
Satisfied with care |
1.08 |
0.608-1.920 |
|
Out of stock |
0.588 |
0.3980-0.869* |
|
Experience side effects |
0.714 |
0.391-1.805 |
|
ARV and food |
1.473 |
0.687-3.157 |
Key: *Statistically significant
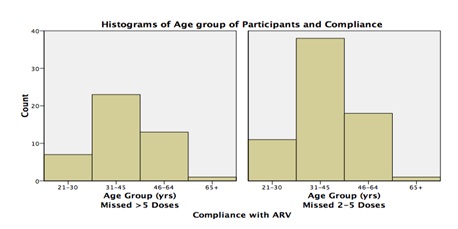
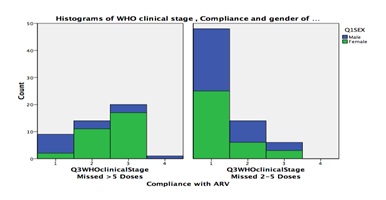
In the univariate analysis the following factors were associated with missing five or more doses: Viral load OR: 5.6, 95%CI: 2.0-16.0, Employment OR: 3.3, 95%CI: 1.5-7.2, Taking active substance OR: 2.5, 95%CI: 1.3-4.7, and Emotional status OR: 1.6, 95%CI: 1.02-2.6. The ART stocks seemed adequate as the OR for out of stock did not lead to missed doses (OR: 0.6, 95%CI: 0.4-0.9). Factors such as gender, education, religion and marital status were not associated with missing five or more doses. After multivariate logistic regression the following factors were associated with missing five or more doses; Taking substance adjusted OR: 3.3, 95%CI: 1.4-7.6; WHO clinical stages 2 and 3 adjusted ORs and 95%CIs: 4.1 (1.2-13.8) and 6.1(1.5-25.1) respectively and viral load adjusted OR: 6.3, 95%CI: 2.1-18.7. Participants taking of active substances and the non-adherence were analyzed and the findings are demonstrated in figure 4 below.
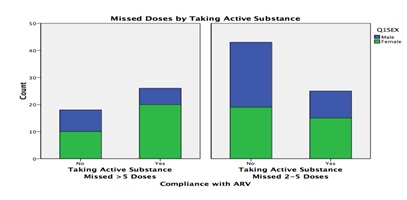
Figure 3 (above) compares missed doses by taking active substances and gender. More women took active substances compared to men and thus were more likely to miss more than five doses compared to men. Those patients who were self and family supported were more likely to miss their doses compared to those supported by NGOs and those who had no support. The participants’ viral load and non-adherence correlation analysis results are illustrated in figure 5 below.
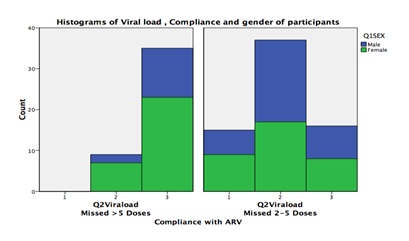
More females had viral load of more than 1000 copies per ml and missed more females missed more than 5 doses compared to males. Figure 6 below shows the outcomes of correlational analysis of participants WHO clinical stage and non-adherence.
All the 112 respondents in the study were asked for the reasons for missed dose/s. Some respondents mentioned more than one reason. The total number of reasons mentioned by the 112 respondents was 142. However, some reasons were recurring among respondents and were summarized together. Reasons mentioned in the order of most common to least commonly were; forgetfulness (21.8%), alcohol use (15.5%), challenges in accessing treatment (9.9%), work commitments (9.9%), transport problems to health facility (7%), lack of food (4.9%), stress (4.2%) and travelling (4.2%). A notable 4.2% of the respondents mentioned discomfort due to ARVs including the side effects as reason for missed dose.
DISCUSSION
The level of non-adherence at the study site
Factors associated with non-adherence
Socio-demographic and economic characteristics
Patient-related factors
Factors which were insignificant to non-adherence included; Patient belief that ART is essential for their HIV care, comfortable to take ART in the presence of others, community disclosure and whether the patient feel taking your ARVs reminds them of the HIV infection. On the other hand, it has been recorded that lack of community disclosure is associated with non-adherence [14]. In addition, Gari et al., have also reported that poor beliefs in the benefits of ARVs were associated with non-adherence [15].
System related factors
Additionally, respondents cited some system related barriers as reason for missed doses. These barriers included transportation costs to the clinic, unfriendly service hours and high healthcare worker-patient ratios and the resultant long waiting hours. Similar findings have been reported in Uganda, where transportation costs accounted for 7.8% of reasons why patients were non-adherent [18]. The association between transport challenges and non-adherence were also reported from other studies [19,20]. As reported in the Presidential Commission of Enquiry, the public health sector suffers from inadequate numbers of staff and availability of equipment and resources [21].
Disease and treatment related factors
While non-adherent respondents would be expected to be sick and with higher WHO clinical stage, only 20% of the respondents reported being sick in the past one month. The results of non-adherence are cumulative over time, thus respondents who were non-adherent during the data collection period might still have been healthy, but with continual non-adherence, a depleted immune system and rising risk of opportunistic infections would eventually become sick patients with time.
Cultural and religious beliefs related factors
Respondent’s last viral load
Respondents WHO clinical stage
Respondents’ responses on the reason/s for ARV missed dose (N=142, Total=100%)
Respondents’ comments
Study recommendations
Perceived severity: Healthcare workers should use results of viral loads to explain resistance at appropriate levels of understanding of patients as a way to promote understanding of the consequences of non-adherence.
Perceived benefits:
• Healthcare workers are advised to plot patients’ biological markers including CD4 and viral loads on a graph to explain benefits of adherence to patients
• Recruitment and the active involvement of “expert patients” these are HIV positive patients who have disclosed their HIV status and trained to motivate other patients and explaining benefits of adhering to treatment and practicing healthy lifestyle while on ART treatment
Perceived barriers:
• Healthcare workers need to strengthen patients’ referral system across the different levels of HIV care so as to make it easier for patients to access continuing care when travelling
• To improve access to ART services for patients in remote areas, ART can be integrated into existing outreach programmes
• Initiate and strengthen effective HIV workplace programs so as to increase awareness among employers on the need for treatment support of employees as well as to reduce stigma which is often experienced at workplaces
• The MoHSS needs to strengthen collaborative efforts with other non-governmental organizations on supportive care for ARV patients such as by providing food support
• Lay counsellors need to be trained in basic communication skills and counselling techniques
Cues to action:
• The MoHSS is recommended to adopt the use of Automated Short Message Service (SMS) as a way of reminding patients their ARVs Self-efficacy
• Healthcare workers should strengthen health education how to manage in case of missed doses
• There is need to anticipate and discuss potential side effects with patients, the time they maybe experienced and importantly how to handle them
ACKNOWLEDGEMENT
The authors would like to firstly thank God through His Holy Spirit and our Lord Jesus Christ who granted us ability to do this article, the Keetmanshoop Hospital for permission to conduct study. Also acknowledge, Dr Arthur T. Chigova, for his psychological support throughout the research. Our sincere gratitude to the research statistician Dr. Lovemore Mahachi.
AUTHOR CONTRIBUTIONS
BLD contributed to the study design particularly the sampling method and data collection method. Both authors revised the manuscript, gave final approval to the version published and they agree to be accountable for all aspects of the article.
REFERENCES
- Ministry of Health and Social Services (2014) National guidelines for antiretroviral therapy (4thedn). Ministry of Health and Social Services, Windhoek, Namibia.
- Uzochukwu BS, Onwujekwe OE, Onoka AC, Okoli C, Uguru NP, et al. (2009) Determinants of non-adherence to subsidized anti-retroviral treatment in southeast Nigeria. Health Policy Plan 24: 189-196.
- Ehlers VJ, Tshisuyi ET (2015) Adherence to antiretroviral treatment by adults in a rural area of Botswana. Curationis 38.
- Gill CJ, Hamer DH, Simon JL, Thea DM, Sabin LL (2005) No room for complacency about adherence to antiretroviral therapy in sub-Saharan Africa. AIDS 19: 1243-1249.
- Tsega B, Srikanth BA, Shewamene Z (2015) Determinants of non-adherence to antiretroviral therapy in adult hospitalized patients, Northwest Ethiopia. Patient Prefer Adherence 9: 373-380.
- Polit DF, Beck CT (2008) Nursing research: Generating and assessing evidence for nursing practice (8thedn). Lippincott Williams & Wilkins, Philadelphia, USA. Pg no: 796.
- Eller LS (2009) Adherence, resistance and antiretroviral therapy. Rutgers, The State University of New Jersey, New York, USA.
- Abdissa AE (2013) Determinant factors affecting adherence to antiretroviral therapy among HIV infected patients in Addis Ababa. University of South Africa, South Africa.
- Nghoshi SS (2016) Assessment of determinants and levels of adherence to antiretroviral therapy in HIV-infected people in Opuwo district, Kunene region, Namibia. University of Namibia, Windhoek, Namibia.
- Nachega JB, Mills EJ, Schechter M (2010) Antiretroviral therapy adherence and retention in care in middle-income and low-income countries: current status of knowledge and research priorities. Curr Opin HIV AIDS 5: 70-77.
- Sasaki Y, Kakimoto K, Dube C, Sikazwe I, Moyo C, et al. (2012) Adherence to antiretroviral therapy (ART) during the early months of treatment in rural Zambia: influence of demographic characteristics and social surroundings of patients. Ann Clin Microbiol Antimicrob 11: 34.
- Campos LN, Guimarães MDC, Remien RH (2010) Anxiety and depression symptoms as risk factors for non-adherence to antiretroviral therapy in Brazil. AIDS Behav 14: 289-299.
- Muessig KE, McLaughlin MM, Nie JM, Cai W, Zheng H, et al. (2014) Suboptimal antiretroviral therapy adherence among HIV-infected adults in Guangzhou, China. AIDS Care 26: 988-995.
- Wasti SP, van Teijlingen E, Simkhada P, Randall J, Baxter S, et al. (2012) Factors influencing adherence to antiretroviral treatment in Asian developing countries: a systematic review. Trop Med Int Health 17: 71-81.
- Gari S, Doig-Acuña C, Smail T, Malungo JR, Martin-Hilber A, et al. (2013) Access to HIV/AIDS care: a systematic review of socio-cultural determinants in low and high income countries. BMC Health Serv Res 13: 198.
- Ministry of Health and Social Services (1998) National drug policy for Namibia. Ministry of Health and Social Services, Windhoek, Namibia.
- De AK, Dalui A (2012) Assessment of factors influencing adherence to anti-retroviral therapy for human immunodeficiency virus positive mothers and their infected children. Indian J Med Sci 66: 247-259.
- Senkomago V, Guwatudde D, Breda M, Khoshnood K (2011) Barriers to antiretroviral adherence in HIV-positive patients receiving free medication in Kayunga, Uganda. AIDS Care 23: 1246-1253.
- Biadgilign S, Deribew A, Amberbir A, Deribe K (2009) Barriers and facilitators to antiretroviral medication adherence among HIV-infected paediatric patients in Ethiopia: A qualitative study. SAHARA J 6: 148-154.
- Tabatabai J, Namakhoma I, Tweya H, Phiri S, Schnitzler P, et al. (2014) Understanding reasons for treatment interruption amongst patients on antiretroviral therapy--a qualitative study at the Lighthouse Clinic, Lilongwe, Malawi. Glob Health Action 7: 24795.
- Ministry of Health and Social Services (2013) Namibia - Demographic and Health Survey 2013. Ministry of Health and Social Services, Government of Namibia, Windhoek, Namibia.
- Drachler Mde L, Drachler CW, Teixeira LB, Leite JC (2016) The scale of self-efficacy expectations of adherence to antiretroviral treatment: A tool for identifying risk for non-adherence to treatment for HIV. PLoS ONE 11: 0147443.
- Loeliger KB, Niccolai LM, Mtungwa LN, Moll A, Shenoi SV (2016) Antiretroviral therapy initiation and adherence in rural South Africa: community health workers' perspectives on barriers and facilitators. AIDS Care 28: 982-993.
- Kaleebu P, Kirungi W, Watera C, Asio J, Lyagoba F, et al. (2015) Virological response and antiretroviral drug resistance emerging during antiretroviral therapy at three treatment centers in Uganda. PLoS ONE 10: 0145536.
- Namibia Statistics Agency (2013) Namibia Population and Housing Census 2011. Namibia Statistics Agency, Government of the Republic of Namibia, Windhoek, Namibia.
Citation: Chigova T, Dolamo BL (2017) Factors Associated with Non-Adherence to Antiretroviral Treatment in Adults at Keetmanshoop District State Hospital in Namibia. J AIDS Clin Res Sex Transm Dis 4: 015.
Copyright: © 2017 Temptation Chigova, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.