Failure to Thrive: To Recognize, to Diagnose and to Treat
*Corresponding Author(s):
Angelo PietrobelliPediatric Unit, Department Of Surgical Sciences, Dentistry, Gynecology And Pediatrics, University Of Verona, Verona, Italy; Pennington Biomedical Research Center, Baton Rouge, LA, United States
Tel:+ 39 0458127125,
Email:angelo.pietrobelli@univr.it
Abstract
Failure to Thrive (FTT) is a condition of abnormal growth pattern due to a state of malnutrition, that may impair child’s future growth.
According with the American Society for Parenteral and Enteral Nutrition (ASPEN), malnutrition, either in excess or in defect, is an imbalance between caloric intake and energy expenditure. Providing an accurate diagnosis and assuring an effective management of this condition appears essential to the clinician. An appropriate treatment is also fundamental to achieve standard growth and to avoid FTT long term effects. However, a common approach to treat, and practical management cannot clearly be recognized in literature yet. Therefore, the purpose of our narrative review is to find reliable and unambiguous indications for optimizing diagnosis, assessment and management of failure to thrive in infants under two years. We will focus on anthropometric tools for diagnosis of FTT, role of anamnesis and physical examination, timing for blood and instrumental exams and first line treatment, to finalize with a common protocol/flow-chart.
Comprehensive electronic literature searches were performed to find all relevant literature reporting diagnostic criteria for FTT. 11 selected papers were then analysed and a flow chart was finally proposed to synthetize the findings and suggesting the clinical approach to FTT.
We found no commonly accepted definition nor a definite pathway to identify FTT in infancy, diagnose it, manage it and follow it up is present in literature. Main limitations of this work are 1: The lack of cohort studies for faltering growth to have reliable indicators; 2: The lack of a proper validation of the proposed flow chart. It would be of extreme interest to start a prospective study, applying the proposed flow chart to assess if efficacious in identifying and successfully managing a child presenting with abnormal growth pattern.
Keywords
Caloric intake; Children; Energy expenditure; Growth; Malnutrition; Nutrition
Introduction
Failure to Thrive (FTT) is a condition of abnormal growth pattern due to a state of malnutrition, that may impair child’s future growth [1-4].
According with the American Society for Parenteral and Enteral Nutrition (ASPEN) [3,5,6], malnutrition, either in excess or in defect, is an imbalance between caloric intake and energy expenditure [7-9]. FTT is due to an insufficient nutrition or impaired nutrient absorption or increased metabolic expenditure [1,2,5,9,10]. The cumulative deficit of nutrients impairs growth, primarily weight, then length and eventually head circumference [1,11]. Aetiology of FTT is commonly classified into non-organic related illness, organic related illness and mixed cases [2]. According with the literature, approximately 80% of FTT cases has not recognized underlying medical conditions [5,6,9,12,13]. The prevalence of FTT seems to be more common in lower socioeconomic communities [3,5,6].
In severe cases faltering growth turned out to be associated with cognitive developmental delay and immune dysfunction [1,5,7,14-18]. Furthermore, nutrition support, prolonged hospitalization and higher health-care costs are proved to be associated with inadequate growth [7,16,19-21].
Providing an accurate diagnosis and assuring an effective management of this condition appears essential to the clinician. Currently, a shared and widely adopted definition of FTT still lacks and several anthropometric parameters are employed to evaluate children’s growth [1,2,11,14,18]. Even though, there is a consensus on applying the 2006 World Health Organization (WHO) charts when evaluating a child’s growth, but there is no general agreement on which statistical tool to employ [2,7,16]. Moreover, the role of a comprehensive anamnesis together with a disease-oriented physical examination [1,10,16,22] and the opportunity of performing tests remain controversial [5,13,16]. An appropriate treatment is also fundamental to achieve standard growth and to avoid FTT long term effects [9,14]. However, a common approach to treat, and practical management cannot clearly be recognized in literature yet.
Therefore, the purpose of our study is to find reliable and unambiguous indications for optimizing diagnosis, assessment and management of failure to thrive in infants under two years. We will focus on anthropometric tools for diagnosis of FTT, role of anamnesis and physical examination, timing for blood and instrumental exams and first line treatment, to finalize with a common protocol/flow-chart. Although, in order to avoid confounding factors, all the studies that considered prematurity or pregnancy-related factors were not taken into consideration in our research.
Materials And Methods
Comprehensive electronic literature searches were performed (April-May 2020) to find all relevant literature reporting diagnostic criteria for FTT. The database PubMed was screened by MM and MCDL, and reviewed by AP. The following search strategy was applied: “Failure to thrive”, “Faltering growth”, “Malnutrition”. The only language limitation was that titles, abstracts and whole paper had to be published in English. The full texts of all articles that appeared to report diagnostic criteria related to failure to thrive in infant populations were evaluated by applying the predetermined PICOS (Population, Intervention, Comparator, Outcome, and Study design) criteria described in table 1.
|
Parameter |
Inclusion |
Exclusion |
|
Population |
Infant populations (1 month-2 years of age), not known disease, |
Population at risk for FTT -e.g congenital heart disease, preterm - , adult, obesity, neonates, hospitalized population |
|
Intervention |
None |
None |
|
Comparator |
None |
None |
|
Outcome |
Setting diagnostic criteria for FTT |
Single parameter analysis; assessment of malnutrition screening tools |
|
Study design |
Clinical and literature reviews, |
None |
|
Guidelines |
Table 1: PICOS criteria for inclusion and exclusion of studies.
11 selected papers were then analysed, and data collected were organized in a table following 14 domains as shown in table 2. A flow chart was finally proposed to synthetize the findings and suggesting the clinical approach to FTT (Figure 1).
|
Author |
Year of publication |
Type of study |
Country |
Populationincluded |
Populationexcluded |
Definition of Failure To Thrive (FTT) |
Diagnosticparameter |
Indicators |
Statistical tool (z score vs p.le) |
Role of Anamnesis |
Role of Physicalexamination |
Blood sample |
Additionaltests |
First line treatment |
|
Bouma S |
2017 |
Review |
USA |
Undernutrition ( childrenaged 1 month to 18 years) |
obese, premature infants, neonates |
Undernutritionas an imbalancebetweennutrientrequirement and intake, resulting in cumulative deficits of energy, protein, or micronutrientsthatmaynegativelyaffectgrowth, development, and otherrelevantoutcomes |
Anthropometricvariables |
Weight-for-height |
Z-score |
Usefuldietaryintake and nutrition and physicalactivityhistory |
Nutritional-focusedphysicalexamination |
NA |
NA |
NA |
|
Cole SZ et al |
2011 |
Guidelines |
USA |
Allchildren |
NA |
Inadequategrowth or the inability to maintaingrowth |
Anthropometricvariables |
Weight for age |
Percentile |
Child’seatinghabits, caloricintake and parent-childinteractions |
Measurements of height, weight, head circumference |
Routine laboratory |
According to clinicalhistory or physicalexamination |
Age-appropriate nutritional |
|
Gahagan S |
2006 |
Review |
USA |
Infants and toddlersyoungerthan 3 years of age |
NA |
Failing to growat a rate consistent with expectedstandards |
Anthropometricvariables |
WeightLength/height |
Percentile |
Complete history (nutritionalhistory, feedingbehaviorhistory, parent-childpatterns of interaction, medicalhistory, family history, social history, history of height and weighttrajectories of parents and siblings) |
Complete physicalexamination: |
Routine laboratorytests are recommended, othersshould be based on hypothesis |
NA |
Nutritional/feedingintervention, treatmedicalcondition |
|
Gonzalez-Viana E. et al |
2017 |
Guidelines |
UK |
Infants and preschoolchildren |
NA |
A pattern of slowerweight gain thanexpected for age and sex |
Anthropometricvariables |
Fall weight for birthweight |
Percentile |
Detailedfeeding or eatinghistory, social assessment |
Clinical and developmentalassessment |
Considerinvestigating for urinarytractinfection and coeliacdisease, furtherinvestigationsifindicated |
Ifindicated |
Behavioral and dietaryintervention |
|
Green Corkins K et al |
2016 |
Review |
USA |
Terminfants to 2 years |
NA |
NA |
Anthropometricvariables, etiology |
Length/height-for-age Weight-for-age |
Z-score |
Chronic and recent |
Nutritional-focusedphysicalexamination |
Role of CRP |
NA |
NA |
|
Homan GJ |
2016 |
Guidelines |
USA |
NA |
NA |
An abnormal pattern of weight gain defined by the lack of sufficientusablenutrition and documented by inadequateweight gain over time |
Clinicalhistory |
Weight for sex and age |
Percentile |
Detailedhistory (nutritionalevaluation and medical, family, and social histories) |
Identifieschronic or acute illness, geneticcondition, assessment for development, and degree of undernutrition |
No standard set of laboratorytestsisrecommended (Ifthereisreasonablesuspicion of a specificunderlyingcondition) |
NA |
Treat the underlying cause |
|
Larson-Nath C et al |
2016 |
Clinicalreview |
USA |
Allchildren |
NA |
A state of |
Anthropometricvariables |
Weight-for-age |
Z-score |
Detailedfeedinghistory |
Suggestsetiology |
Rarelyuncovers |
Rarelyuncovers |
Behavioralapproach, |
|
Mehta NM et al |
2013 |
Review |
USA |
Undernutrition |
obese, neonates |
An imbalancebetween |
Anthropometricvariables |
Weight-for-age |
Z-score |
Definingchronicity (< o > 3 months) |
NA |
CRP and inflammatory |
NA |
NA |
|
Schlaudecker EP et al |
2017 |
Commentary |
Australia, USA, UK, |
First year of life |
NA |
Failure to thrive (FTT) is a descriptiveterm
|
Anthropometricvariables |
Weight-for-length |
Percentile |
NA |
Indicator of FTT |
NA |
NA |
NA |
|
Shields B et al |
2012 |
Clinicalreview |
UK |
NA |
NA |
Failure to thrivehasbeendefined |
Anthropometricvariables |
Weight-for-age |
Percentile |
Excludeunderlyingmedical |
Excludeunderlying |
Not in first place |
Not in first place |
Behavioral and |
|
Wit JM et al |
2019 |
Guidelines |
Netherlands |
Infants and children |
NA |
Growthfailure = |
Anthropometricvariables |
Height-for-age |
Standard deviation |
Detailedmedicalhistory |
Look for |
If no clues: |
Left hand and wrist |
NA |
Table 2: Authors and parameters analysed.
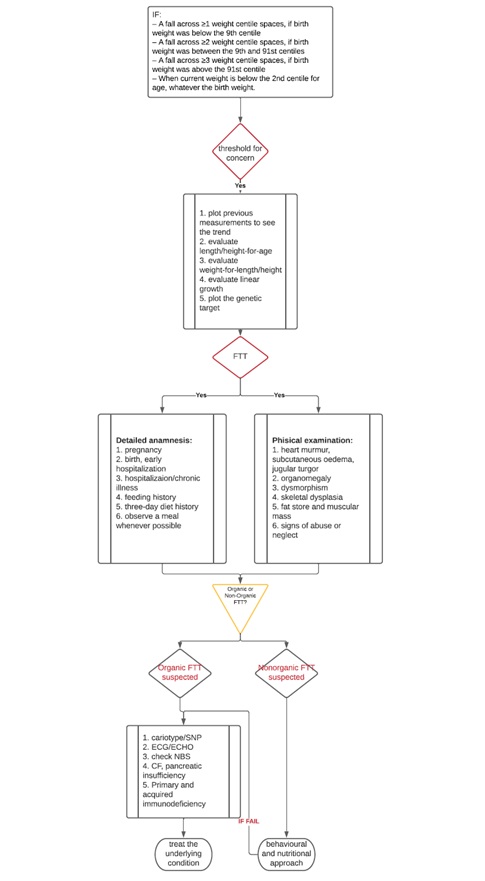 Figure 1: FTT flow chart.
Figure 1: FTT flow chart.
Results
To respect the all-encompassing purpose of the present research, we selected articles, guidelines, review and clinical review. Using fourteen parameters, we considered 11 articles published between 2006 and 2019 (Table 2). 7 studies out of 11 were performed in the USA [1,2,5-7,9,23], 2 in the UK [4,14], 1 in the Netherland [22] and 1 had data collected from different countries [24].
The population included was variable among the studies, but all were comprehensive of the target population, subjects under 2 years of age. In fact, 4 studies out of 11 concentrated on pre-school children [4,6,23,24], 5 were comprehensive of all children, excluding neonates, until 18 years old [2,5,7,9,22], 2 studies did not specify the population included [1,14]. Moreover, two studies focused, specifically, on under nutrition [2,7].
Only two studies out of eleven pointed out the excluded population: children with obesity, neonates and preterm babies [2,7].
As introduced above, definition of failure to thrive is essential. For consideration, all the authors agree that failure to thrive could be defined as an inadequate weight gain, in general or referred to age-references. Some authors highlight the role of calories and nutrients imbalance as common mechanisms leading to faltering growth [1,2,7,9].
Among all studies anthropometric indexes seem to be crucial to make a prompt diagnosis, however, extreme variability exists in which is the most reliable parameter to employ. In fact, the most used is the weight-for-age parameter, usually combined with other indicators. The studies who did not employ the weight-for-age index, one used the weight gain velocity in children younger than 2 years of age and the measure of weight loss in those between 2 and 20 years of age [23]. Another one adopted the evaluation of weight-for-length/height, head circumference, growth velocity to make a correct evaluation of failure to thrive [6].
Despite the indices mentioned, there is not a consensus on which statistical tool would be more appropriate to embrace. In fact, the slight majority of the authors, 6 out of 11, showed to be keener on percentiles [1,4-6,14,24], 4 on z-score [2,7,9,23] and one on standard deviation [22].
On how to collect a correct anamnesis to investigate a child who is not growing properly, the majority of the authors, 8/11, suggested to collect a detailed dietary history [1,4-7,9,14,23], one did not specified what to ask [24], 1 focused on chronicity and possible underlying illnesses [2] and one indicated to collect a detailed general medical history to assess primary or secondary growth failure [22].
When coming to the physical examination, 4 out of eleven suggested to perform a nutritional-focused examination [5,7,23,24], three proposed a complete assessment [1,4,6], two oriented their examination on the possible aetiology [9,14], one suggested to look for syndromic features [22] and one did not specified how to conduct the physical examination [2].
4 out of 11 did not recommend performing blood sample as a first approach but only if guided by specific symptoms [1,5,9,14]. Two focused exams on the research of inflammatory markers [2,23], one recommended always to perform blood sample as a routine [6], one suggested to have exams if no clues for aetiology was suggested by the history and the physical examination [22], one proposed to first exclude urinary tract infection and eventually perform further exams only if clinical suspect was present [4]. Finally, 2 out of 11 did not clarify their position on blood sample investigation [7,24].
Six out of eleven did not suggest to undertaking instrumental exams [1,2,6,7,23,24], four only if a clinical suspect was present [4,5,9,14] and one indicated to have a left hand and wrist X-Ray performed as first assessment [22].
Finally, 5 out of 11 suggested a behavioural and nutritional approach as first line treatment, 5 did not specified a therapy approach and one proposed to treat first the underlying cause.
Having summarized and combined all the above information, a practical flow chart was drawn to provide the Paediatrician with complete and linear indications to approach a child with suspected FTT (Figure 1).
Since weight-for-age is the easiest acquired parameters at GP practice, we decided to use the following as threshold for concern, employing only the weight-for-age:
- A reduction of weight-for-age of one or more percentile space if birth weight was less than 9th p.le
- A reduction of weight-for-age of two or more percentile spaces if birth weight was between 9th and 91st p.le
- A reduction of weight-for-age of three or more percentile spaces if birth weight was above 91st p.le
- Weight-for-age < 2nd percentile, whatever the birth weight had been.
If threshold for concern is reached, then it will be necessary to plot previous measurements on the chart to evaluate the growth trajectory. We also recommend to plot length/height and head circumference to evaluate any discrepancy among these parameters. Evaluate linear growth and plot genetic target as well whenever possible, so not to underestimate any familial short stature.
If applying the most commonly recognized parameters to evaluate FTT (Table 3), [18,25,26], it is ascertained then a detailed anamnesis as well as a thorough physical examination, looking at organic cause of FTT should be undertaken.
|
- Weight <75% of median weight for chronological age (Gomez criterion) |
|
- Weight <80% of median weight for length (Water low criterion) |
|
- Body mass index for chronological age, 5th centile |
|
- Weight for chronological age <5th centile |
|
- Length for chronological age <5th centile |
|
- Weight deceleration crossing more than two major centile lines; centile lines used: 5, 10, 25, 50, 75, 90, 95, from birth until weight within the given age group |
|
- Conditional weight gain = lowest 5%, adjusted for regression towards the mean from birth until weight within the given age group |
Table 3: Commonly applied parameters for FTT.
If an organic cause for FTT is suggested, then clinically oriented investigations must be performed, and underlying condition treated. If FTT does not recognize any causing disease, a behavioural and nutritional approach is recommended.
What is crucial to evaluate is the correct energy intake based upon age-requirements (110 kcal/Kg < 6 months, 100 kcal/Kg from 6 to 12 months [6], 102 kcal/Kg from 1 to 3 years [27]). If the energy intake is adequate for the age but the growth is not satisfying, then an increase in the energy intake should be calculated based upon the caloric needs for age and the ideal weight-for-length/height to enforce the catch-up growth [27]. Conversely, if the energy intake does not reach the needs required, adequate nutritional intake should be provided, and prompt behavioural intervention should be undertaken [4,9,25].
After an efficacious intervention we would expect a recovery in weight gain within four to eight weeks [14]. Frequent weight, on a daily basis, is overall discouraged. As a general rule, infants need to be seen and weighted more frequently than older children [1]. The child should be weighted monthly for the first 6 months of age, two-monthly when 6-12 months and every three months after that [14].
Adequate weight gain depends on age and could be summarised as follows:
25-30 g/day from 0 to 3 months, 20 g/day from 3 to 6 months, 12 g/day from 6 to 12 months, 8 g/day from 12 to 18 months [28].
If adequate weight gain is observed the child continues the follow up as scheduled. If weight growth is still faltering, then a blood sample should be performed to exclude underlying pathological conditions [9].
Discussion
In the United States, FTT is seen in 5 - 10 % of children in primary care settings [4,9] and in 3 - 5% of children in hospital settings [5,10,11]. It is a relevant issue and source of concerns both for parents and for health care providers [4]. In fact, failure to thrive, if not effectively recognized, can lead to malnutrition [5]. It has not only a clear impact on growth, but there is evidence that FTT can impair a proper immune system and neurological development [1,7,14-16]. On a global perspective, childhood nutrition status is a predictor of morbidity and mortality risk [12,16]. In addition, malnutrition is associated with increased health care costs [7,16,19] and prolonged hospitalization17,20,21. Therefore, we decided to analyse literature about FTT, giving indications on how to diagnose and to manage such a relevant and diffused issue. We organized data in a table (Table 2) and suggested a flow chart (Figure 1) for the correct approach to FTT.
Of the papers reviewed, 11 were selected for the purpose of giving shared indications for diagnosis and management of faltering growth (Table 2). The 11 papers selected provided a definition of FTT and suggested methods of diagnosis. Most of them addressed health care providers and paediatricians who, in the first place, can find themselves dealing with a child who grows poorly.
The majority of the papers are guidelines or review about the subject. UK guidelines are based upon a cohort study of 5624 participants recruited from the National Birth Registry in Denmark [18] and a cohort of 1978 healthy term infants in a study conducted in US by Ross E et al. [29]. Population studies are available when speaking of diagnostic tools during hospitalization, but even in that case the sample size of the cohort is insufficient to determine reliability of such tools, which is beyond the interest of this paper [30]. Purpose of this paper is to provide paediatricians with useful and as much unambiguous indication to diagnose and successfully manage a child presenting with poor growth concern as possible. Therefore, employing guidelines and literature review proved to be helpful and of great utility.
Population excluded by the present article and the source of literature reviewed is children with obesity, neonates and preterm babies. For those categories of patients, per se evaluation is indeed required. Even if obesity can be considered a different form of malnutrition, no features of failure to thrive are recognizable. Faltering growth in neonates usually has causes due to maternal status, pregnancy, delivery related issues, initial feeding and underlying condition that deserve a dedicated chapter. Finally, prematurity is itself a major cause for failure to thrive. Preterm babies require specific attention under the nutritional point of view and a dedicated management. Once again, this work aims at giving advice on how to manage a child with faltering growth who has no apparent reason for it.
Even if the topic of failure to thrive is so diffused and relevant, either in terms of prevalence and of consequences, a unique and shared definition still lacks [2,11,24,29]. Most of the authors agree that there is not a one and only parameter to make an accurate diagnosis, but it is mostly a combination of anthropometric parameters [5,18,23]. Besides, the aspect of time seems to be crucial: several observations, even before the actual, help identify a pattern of growth and eventual precise reason for a delay. Before 1985, social aspects, such as neglect and maltreatment, were involved in the definition. A consensus in 1985, though, clarify that the diagnosis of faltering growth must be made on anthropometric parameters only [18].
In common clinical practice FTT is defined as either weight for age <5 centile on multiple occasions or a weight deceleration that crosses two percentile lines [1,5].
Metha N et al. [2], in 2013, made what is now known as the paradigm shift towards aetiology-related definition. Nonetheless, aetiology and chronicity of FTT are used together with anthropometric parameters to classify malnutrition in terms of severity, but again, anthropometrics is essential in identifying those affected or at risk [2,7].
Anthropometric parameters were considered, by all the authors, crucial to make the diagnosis. For the vast majority of them, anthropometrics is sufficient to make a proper diagnosis [4-7,9,14,22,24]. Green-Corkins et al., adds chronicity, mechanism and outcomes to make a comprehensive diagnosis [23], Homan GJ recognized a detailed clinical history and a thorough physical examination as central when making a proper diagnosis, together with anthropometric indicators [1]. Finally, as previously anticipated, in his paradigm shift, Metha N implements aetiology, chronicity, mechanisms and outcomes in the definition of FTT [2].
We decided to adopt anthropometric variables, as well, as the first approach to a child with faltering growth. Measuring a child is indeed the most diffused practice, widely recognized and easy to obtain when visiting a child, without any confounding factors may lead to a misdiagnose.
Weight for age is the only parameter common to each study analysed. In particular, it is an indicator easy to acquire at any visit with a paediatrician [11] and should be taken every time a child is admitted for hospitalization. Furthermore, weight is the first parameter affected in a child with FTT, followed by length if the growths persists faltering [24]. It is extremely important to have a reliable parameter to count on, therefore when weighting a child, it is advisable to meticulously record the unit and the scale employed. After having recorded the weight it is essential to plot it on the WHO growth chart in order to compare the single value with the standard distribution for age and sex. Interestingly, evaluation of FTT relies not on a single observation but seems to require a dynamic analysis. Therefore, whenever possible it is suggested to plot all the previous measurements available to evaluate the trend of the child’s weight, as suggested by Cole S et al. [5]. Weight-for-age and its trend over the years is considered sufficient by some authors to make a diagnosis of FTT and to subsequently start an adequate treatment, if conditions of concerns are present [11].
Nonetheless, weight for age alone does not seem sufficient as a single indicator [5,18,23]. Gonzalez-Viana et al., in the NICE guidelines suggest considering weight as a threshold for concerns, and then weight the child, measure their length, and plot the actual and available previous measurements on WHO growth chart. If concern in child >2 years evaluate BMI [4]. Other commonly employed parameters are weight-for-length/height, which is known to be a measure of wasting or acute malnutrition [12]; length/height for age, a measure of stunting or chronic malnutrition [2,6,7], which usually present later as manifestation of under nutrition [24].
In our flow chart we decided to maintain the UK approach considering inadequate weight for age the trigger for further concern [4,12,18]. It is indeed an easily acquired parameter, a precocious indicator of FTT [23], a measure of underweight or wasting and stunting combined. Moreover, it does not require previous measurements but the weight at birth and maintains the concern regarding the weight-for-age <2nd centile [11]. Besides, the evidence for choosing such parameters derives from a population study, which, as stated above, is very rare for such a huge subject [4].
As UK guidelines, if threshold of concerns is reached, we suggest plotting previous weight measurements on chart to see the trend [15,23], measure length/height and evaluate it for age and in relationship to weight to assess weight-for-length/height change and linear growth over time [6]. Any weight change below the 5th percentile may indicate a child is at risk of FTT. The use of weight velocities allows for rapid assessment of poor weight gain while accounting for age-dependent changes in growth [5,12,23]. For children >2 years BMI should be calculated. If the BMI is below the 2nd centile, be aware this may reflect either under nutrition or a small build; if the BMI is below the 0.4th centile, this suggests probable under nutrition that needs assessment and intervention [4].
Finally, beside evaluating the growth trend, it would be recommended to plot the genetic target of the child in order not to diagnose an absent disorder or misdiagnose a familiar short stature [6,10,11].
Adoption of z-score or percentile when evaluating parameters is a controversial topic. In fact, 4 authors out of 11 adopted z-score, 5 out of 11 adopted percentile and one adopted standard deviation, which can be equated to z-score, since this latter represents how many standard deviations a value is from the mean value of a normal distribution. Z-score is how far from the mean, in standard deviations, a child is compared with reference data for a child of the same age for each parameter23. Some studies claim that z-score can identify the extreme values and, in case of changes, can identify the entity of change in terms of improvement or worsening7. Percentile, instead, can only set a threshold above or below which the value is plotted, not specifying in terms of numbers the entity of an eventual change. Nonetheless, percentile appears to be the most diffused way of considering growth parameters practitioners are used to it. Besides, as shown above, it can be easily adopted as a threshold of suspect and concern [4,11]. However, not showing the entity of change (child could remain <3rd centile even if growth has improved), plotting measurements on the growth chart becomes even more essential to visualize the trend of the parameters and give the idea of improvement or changes [6]. We could summarize that percentile is appropriate to set the threshold of suspect and start approaching the issue; Z-score is appropriate to classify severity of malnutrition2 and possibly describe the changes in case of extreme values [7,9,23].
A complete and detailed anamnesis is essential. Since there is evidence that the first 1000 days of life-period from conception to two years of age- is crucial in terms of factors that can influence growth, such as nutrition, genetics, epigenetics and hormonal aspects [31], we suggest starting from pregnancy history, investigate teratogen exposure and eventual hospitalization at birth [11]. In fact, oligohydramnios can be associated with poor intrauterine growth. Fetal alcohol syndrome is a common cause of FTT, therefore asking for alcohol and drug abuse as well as drugs intake during pregnancy is essential. Early hospitalization at birth puts strain on early parent-child bonding opportunities and in turn represents risk factors for nutritional neglect [10]. Prematurity is a per se cause of FTT, therefore preterm babies require a specific assessment and specific discussion.
History of recent illness and/or hospitalization is to be carefully taken into consideration [1,2,6,14,22,23]. Chronic medical conditions must be highlighted [12,23]. In fact, chronic diseases represent, an independent risk factor for FTT, especially those with nutritional implications [23]. Moreover, recent literature shows that chronically elevated inflammatory indexes, such as CRP and cytokines, play a decisive role in malnutrition [23].
History of recurrent and/or severe respiratory infection, mucocutaneous and urinary tract infection should rise the suspect of primary or acquired immunodeficiency [5].
Majority of the authors, then, suggests collecting a detailed feeding history of the child. For breastfed babies, direct observation of feeding process to ensure proper technique, latch-on, and swallow is strongly recommended. For bottle-fed ones, paediatrician should ensure how formula is prepared, timing of feeding and number of feeds, to monitor parents’ reliability and adequacy together with an objective evaluation of actual energy intake [5]. For older children, reporting eating behaviour, in terms of mealtimes, feeding habits and poor nutritional food assumption, lack of a familiar routine, and distractions during feeding, together with inadequate caretaker responses to the child’s feeding needs, could represent the key for understanding the present condition and subsequently put in place targeted measures [1,4-7,9,14,23]. Requiring and evaluating a three-day dietary diary can be helpful in assessing caloric and nutritional intake [10,25].
In general, whenever the possibility presents, feeding observation is strongly advised [4-6].
Another relevant aspect to be evaluated is the interaction between parents and child. In fact, poor social conditions [13], history of drug abuse and psychiatric disease could lead and suggest parental neglect, a primary cause for FTT [1,4-6,10,14].
All authors highlight the importance of a thorough and meticulous physical examination in order to rule out possible underlying conditions that could determine faltering growth [9,19].
In particular, evidence of heart murmur, subcutaneous oedema and jugular veins distension could suggest a congenital heart disease which requires further investigations [5,14].
Undiagnosed inherited metabolic disorders can present with failure to thrive, therefore a complete physical examination emphasizing neurodevelopmental status, evaluation of skin for neurocutaneous markings and hair for abnormalities, dysmorphic features, research for hepatomegaly/splenomegaly is strongly recommended [6,10]. In case an IMD is suspected, checking newborn screening is one of the first action to undertake [10].
Disproportion of limbs and trunks could suggest a skeletal dysplasia. Distinctive features should lead to rule out genetic syndromes such as Noonan, Silver-Russel and Prader Willi syndrome, and Turner syndrome in females [10].
Nutritional assessment is essential as well to classify the severity of malnutrition [1,6]. A nutritional-focused physical examination should be comprehensive, moving head to toe, and focusing on specific medical history-related aspects. Assessment of fat store and muscular mass with inspection and palpation is crucial alongside looking for micronutrient deficiency reviewing hair, eyes, oral cavity, skin, and nails [1,23].
Finally, clinicians should always be alert and vigilant in seeking any sign of physical abuse or neglect, such as recurrent, unexplained, or pathognomonic injuries [5].
Scientific evidences show that laboratory work up contributes to as few as 1% of FTT diagnoses [1,9,10,13,14].
Therefore, no standard set of exams is recommended [14,25]. A thorough history and a scrupulous physical examination should provide the necessary elements to start a treatment [1,19]. If the child seems well and there are no suggestive signs or symptoms, further investigations are unlikely to reveal an unrecognised cause [4].
The past medical history and the detailed physical examination should lead the clinician to request specific investigations [6].
In case of FTT associated with global developmental delay, autism, multiple congenital anomalies and dysmorphism chromosomal analysis and SNP array are certainly to be considered [10].
Signs of cardiac involvement should lead to chest X ray, cardiological review and, in case of arrhythmias, to ECG and thyroid function assessment [6].
Newborn screening test review and specific metabolic assessment should be requested in case of multiorgan involvement possibly due to IMD [10].
Cystic fibrosis, coeliac disease and pancreatic insufficiency must be investigated in case of evidence of malabsorption [1,6].
A child with recurrent and severe infections should be investigated for primary and acquired immunodeficiency [1,5].
Some authors suggest proceeding with laboratory tests only after behavioural and nutritional interventions have failed [9].
Finally, chronic inflammatory condition can contribute to FTT. In terms of laboratory tests, inflammatory markers seem to be more relevant due to the role that chronic inflammation plays in malnutrition instead of albumin and prealbumin which were adopted in the past as malnutrition indexes. These latter seem to be not reliable since they are influenced by many factors, including inflammatory status itself [7,23].
If an organic cause is recognized, it must be treated as first [5,6], even though behavioural approach could be employed also in patients with known medical cause for FTT [13].
Nonetheless, the first common cause of faltering growth is the insufficient energy intake [1,14] and recognizes non-organic cause. This is the reason why the approach should both focus on behaviour and on caloric intake optimization [6,9,14,19].
The behavioural intervention should guarantee a location of the meal which is appropriate for the developmental status of the child [9]. It is essential that meals and snacks are offered following an age-determined schedule and that are time-limited, e.g. no more than 20-30 minutes for a main meal. Out of hours snacks must be avoided as well as juice or excessive milk consumption for toddlers [5,9,11,14,19]. Optimizing the caloric intake should start assuring that formula is properly made or that, for those breastfed, lactation is appropriate [5,9]. Offering increased caloric beverages is recommended only if behavioural approach fails9. What is suggested is that caloric beverages, added at appropriate time, are offered with meals and snacks [9,11]. In case all the previous strategies have failed, after 3-4 months of intensive treatment or sooner for newborns, hospitalization is strongly recommended [1,6,9]. When considering hospitalization, though, high cost, parental anxiety and risk of hospital acquired infection should always be taken into consideration [14,19].
Follow up for catch up growth is crucial [1,11]. Monitoring should include measurement for weight, length/height. Recovery can be defined once the current centile falls within 1-2 centile spaces of the earlier position, which may take several months [14]. Long term follow-up is needed for two major reasons. The first one is that relapses can occur, especially if a first cause is not clearly identified [1]. The second reason why a long-term monitoring is essential is because children who had suffered from FTT and malnutrition are at higher risk for developmental and behavioural problems [6].
UK guidelines suggest timing of follow up would depend on age of the child and can range 1-6 months follow up on treatment, plus 1-3 months after the treatment has been stopped [19].
Conclusion
As seen above, no commonly accepted definition nor a definite pathway to identify FTT in infancy, diagnose it, manage it and follow it up is present in literature. We reviewed the most recent publications on the theme, selected 11 papers and suggested a Flow Chart to give a structured and practical approach to failure to thrive, on the basis of the most recent publication on the subject. Main limitations of this work are 1: The lack of cohort studies for faltering growth to have reliable indicators; 2: The lack of a proper validation of the proposed flow chart. It would be of extreme interest to start a prospective study, applying the proposed flow chart to assess if efficacious in identifying and successfully managing a child presenting with abnormal growth pattern.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- Homan GJ (2016) Failure to thrive: A practical guide. American Family Physician 94: 295-299.
- Mehta NM, Corkins MR, Lyman B, Malone A, Goday PS, et al. (2013) Defining pediatric malnutrition: A paradigm shift toward etiology-related definitions. JPEN J Parenter Enteral Nutr 37: 460-481.
- de Onis M, Monteiro C, Akre J, Clugston G (1993) The worldwide magnitude of protein-energy malnutrition: An overview from the WHO global database on child growth. Bull World Health Organ 71: 703-712.
- Gonzalez-Viana E, Dworzynski K, Murphy MS, Peek R (2017) Faltering growth in children: Summary of NICE guidance. BMJ 358: 4219.
- Cole SZ, Lanham JS (2011) Failure to thrive: An update. Am Fam Physician 83: 829-834.
- Gahagan S (2006) Failure to thrive: A consequence of undernutrition. Pediatr Rev 27: 1-11.
- Bouma S (2017) Diagnosing pediatric malnutrition: Paradigm shifts of etiology-related definitions and appraisal of the indicators. Nutr Clin Pract 32: 52-67.
- Becker PJ, Bellini SG, Vega MW, Corkins MR, Spear BA, et al. (2020) Validity and reliability of pediatric nutrition screening tools for hospital, outpatient, and community settings: A 2018 evidence analysis center systematic review. J Acad Nutr Diet 120: 288-318.
- Larson-Nath C, Biank VF (2016) Clinical review of failure to thrive in pediatric patients. Pediatr Ann 45: 46-49.
- Rabago J, Marra K, Allmendinger N, Shur N (2015) The clinical geneticist and the evaluation of failure to thrive versus failure to feed. Am J Med Genet C Semin Med Genet 169: 337-348.
- Goh LH, How CH, Ng KH (2016) Failure to thrive in babies and toddlers. Singapore Med J 57: 287-291.
- Wright CM, Garcia AL (2012) Child undernutrition in affluent societies: What are we talking about? Proc Nutr Soc 71: 545-555.
- Larson-Nath C, St Clair N, Goday P (2018) Hospitalization for failure to thrive: A prospective descriptive report. Clin Pediatr 57: 212-219.
- Shields B, Wacogne I, Wright CM (2012) Weight faltering and failure to thrive in infancy and early childhood. BMJ 345: 5931.
- Wright CM, Matthews JNS, Waterston A, Aynsley-Green A (1994) What is a normal rate of weight gain in infancy? Acta Paediatr 83: 351-356.
- Corkins MR (2017) Why Is Diagnosing Pediatric Malnutrition Important? Nutr Clin Pract 32: 15-18.
- Pimenta FS, Oliveira CM, Hattori WT, Teixeira KR (2018) Agreement between subjective global nutritional assessment and the nutritional assessment of the World Health Organization. J Pediatr 94: 602-608.
- Olsen EM, Petersen J, Skovgaard AM, Weile B, Jørgensen T, et al. (2007) Failure to thrive: The prevalence and concurrence of anthropometric criteria in a general infant population. Arch Dis Child 92: 109-114.
- National Guideline Alliance (2017) Faltering growth - recognition and management. National Institute for Health and Care Excellence, London, UK.
- de Oliveira TC, de Albuquerque IZ, Stringhini MLF, Mortoza AS, de Morais BA (2017) The nutritional status of hospitalized children and adolescents: A comparison between two nutritional assessment tools with anthropometric parameters. Rev Paul Pediatr 35: 273-280.
- Hulst JM, Joosten KFM (2018) Nutrition screening: Coding after discharge underestimates the prevalence of undernutrition. J Acad Nutr Diet 118: 33-36.
- Wit JM, Kamp GA, Oostdijk W (2019) Towards a rational and efficient diagnostic approach in children referred for growth failure to the general paediatrician. Horm Res Paediatr 19: 223-240.
- Green Corkins K, Teague EE (2017) Pediatric nutrition assessment: Anthropometrics to zinc. Nutr Clin Pract 32: 40-51.
- Schlaudecker EP, Munoz FM, Bardají A, Boghossian NS, KhalilA, et al. (2017) Small for gestational age: Case definition & guidelines for data collection, analysis, and presentation of maternal immunisation safety data. Vaccine 35: 6518-6528.
- Jaffe AC (2011) Failure to thrive: Current clinical concepts. Pediatr Rev 32: 100-108.
- Daymont C, Hoffman N, Schaefer EW, Fiks AG (2020) Clinician diagnoses of failure to thrive before and after switch to World Health Organization growth curves. Acad Pediatr 20: 405-412.
- Hughes HK, Kahl L (2018) The Harriet Lane Handbook: A Manual for Pediatric House Officers. Elsevier, Philadelphia, USA.
- Kliegman RM, Stanton BF, Geme JS, Schor NF (2015) Nelson Textbook of Pediatrics E-Book. Elsevier Health Sciences, Amsterdam, Netherlands.
- Ross ES, Krebs NF, Shroyer ALW, Dickinson LM, Barrett PH, et al. (2009) Early growth faltering in healthy term infants predicts longitudinal growth. Early Hum Dev 85: 583-588.
- Klanjsek P, Pajnkihar M, MarcunVarda N, PovalejBrzan P (2019) Screening and assessment tools for early detection of malnutrition in hospitalised children: A systematic review of validation studies. BMJ Open. 9: 1-17.
- Pietrobelli A, Agosti M (2017) Nutrition in the first 1000 days: Ten practices to minimize obesity emerging from published science. Int J Environ Res Public Health 14: 1491.
Citation: Messina M, Di Lorenzo MC, Banzato C, Moreno LA, Piacentini G, et al. (2021) Failure to Thrive: To Recognize, to Diagnose and to Treat. J Food Sci Nutr 7: 105.
Copyright: © 2021 Martina Messina, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.