
Journal of Ophthalmology & Clinical Research Category: Clinical
Type: Research Article
Fasanella-Servat Operation for Moderate to Severe Blepharoptosis
*Corresponding Author(s):
Mithra O GonzalezDepartment Of Ophthalmology, University Of Rochester, Rochester, New York, United States
Tel:+1 5852754270,
Email:Mithra_Gonzalez@URMC.Rochester.edu
Received Date: Apr 17, 2017
Accepted Date: Jun 05, 2017
Published Date: Jun 19, 2017
Abstract
Purpose
To determine the efficacy of the Fasanella-Servat operation in patients with moderate to severe blepharoptosis.
Methods
Case-review of 40 eyelids with an upper eyelid to pupillary Margin Reflex Distance (MRD1)
Results
The mean pre-operative MRD1 was 0.02 mm while the mean post-operative MRD1 was 3.14mm. There was one case of eyelid contour abnormality and asymmetry. Three separate complications occurred. One revision was required.
Conclusion
The Fasanella-Servat operation may provide functional improvement and serve as an alternative to traditional surgical options for those with moderate to severe blepharoptosis.
To determine the efficacy of the Fasanella-Servat operation in patients with moderate to severe blepharoptosis.
Methods
Case-review of 40 eyelids with an upper eyelid to pupillary Margin Reflex Distance (MRD1)
Results
The mean pre-operative MRD1 was 0.02 mm while the mean post-operative MRD1 was 3.14mm. There was one case of eyelid contour abnormality and asymmetry. Three separate complications occurred. One revision was required.
Conclusion
The Fasanella-Servat operation may provide functional improvement and serve as an alternative to traditional surgical options for those with moderate to severe blepharoptosis.
Keywords
Blepharoptosis; Fasanella-Servat operation; Ptosis
INTRODUCTION
In 1961, Fasanella and Servat introduced a simplified method for the correction of small amounts of blepharoptosis associated with good levator function [1]. They described the procedure as an excision of tarsoconjunctiva, Müller’s muscle, and the levator palpebrae superioris muscle. The Fasanella–Servat operation has been employed for all types of blepharoptosis, including congenital, myogenic, neurogenic, traumatic, ptosis in Horner’s syndrome, and blepharoptosis of the an ophthalmic socket. Regardless of the type of blepharoptosis, it is generally accepted that this procedure should be reserved forces in which there is at least 10 mm of levator excursion and no more than 3 mm of ptosis present [1-5]. It may also be used in cases of contour abnormalities with little to no ptosis [2].
The procedure gained wide acceptance from the very beginning. However, the surgical technique, the proposed mechanism of action, and its indications have been challenged and modified on several occasions [2,6-8]. The Fasanella-Servat approach was initially regarded as a form of levator resection [9]. Several authors have since reported excellent success rates without resection of the levator aponeurosis or Müller’s muscle, positing that the effect of the Fasanella-Servat procedure is achieved by shortening of the vertical posterior lamella, wound contracture, and advancement of Müller’s muscle along the tarsus [4,6].
Conventionally, the Fasanella-Servat operation has been employed for minimal ptosis with good levator function, and this is reflected in the published literature regarding outcomes of the Fasanella-Servat procedure [1-5,7,10]. We were curious regarding the utility of this operation in patients with moderate to severe ptosis, and we hereby present our experience with the Fasanella-Servat surgical repair of blepharoptosis in these patients.
The procedure gained wide acceptance from the very beginning. However, the surgical technique, the proposed mechanism of action, and its indications have been challenged and modified on several occasions [2,6-8]. The Fasanella-Servat approach was initially regarded as a form of levator resection [9]. Several authors have since reported excellent success rates without resection of the levator aponeurosis or Müller’s muscle, positing that the effect of the Fasanella-Servat procedure is achieved by shortening of the vertical posterior lamella, wound contracture, and advancement of Müller’s muscle along the tarsus [4,6].
Conventionally, the Fasanella-Servat operation has been employed for minimal ptosis with good levator function, and this is reflected in the published literature regarding outcomes of the Fasanella-Servat procedure [1-5,7,10]. We were curious regarding the utility of this operation in patients with moderate to severe ptosis, and we hereby present our experience with the Fasanella-Servat surgical repair of blepharoptosis in these patients.
MATERIALS AND METHODS
We retrospectively reviewed the charts of a single surgeon from June 2003 to December 2009 for all Fasanella-Servat operations performed. The surgical records were collected to determine patient gender, laterality of Fasanella-Servat procedure, blepharoptosis type, date of last follow-up, and availability of postoperative photographs for review.
Inclusion criteria and outcomes measured
Study inclusion criteria included an MRD1 value of <1mm, a levator excursion of >0mm, and no past history of ptosis surgery on the same eye. Those patients with neurogenic, myogenic, or mechanical ptosis were not included in this study.
Post-operative photographs were evaluated by a blinded ophthalmic oculofacial surgeon for eyelid height, contour, symmetry, and overall cosmesis. Before evaluation, the photograph of the patients’ eyes was adjusted such that the horizontal white to white distance was 10mm, then MRD1was calculated.
Outcomes were classified based on a previously published study [11]. Eyelid height was considered excellent if the MRD1 was ≥2.5 and ≤4 mm; satisfactory for MRD1 ≥1 and <2.5mm; and poor for MRD1 <1mm or >4mm. Symmetry was regarded as excellent for equivalent eyelid heights, satisfactory for a height difference of ≤1mm between eyelids, and poor for a difference of >1mm. Eyelid contour was judged on the arch of the upper eyelid margin: excellent results exhibited a flawless, smooth contour; satisfactory results showed minimal eyelid peaking, flattening, or lateral ptosis; and poor results demonstrated significant contour abnormalities. Overall cosmesis was subjectively graded on the patient’s complete postoperative eyelid appearance.
Post-operative photographs were evaluated by a blinded ophthalmic oculofacial surgeon for eyelid height, contour, symmetry, and overall cosmesis. Before evaluation, the photograph of the patients’ eyes was adjusted such that the horizontal white to white distance was 10mm, then MRD1was calculated.
Outcomes were classified based on a previously published study [11]. Eyelid height was considered excellent if the MRD1 was ≥2.5 and ≤4 mm; satisfactory for MRD1 ≥1 and <2.5mm; and poor for MRD1 <1mm or >4mm. Symmetry was regarded as excellent for equivalent eyelid heights, satisfactory for a height difference of ≤1mm between eyelids, and poor for a difference of >1mm. Eyelid contour was judged on the arch of the upper eyelid margin: excellent results exhibited a flawless, smooth contour; satisfactory results showed minimal eyelid peaking, flattening, or lateral ptosis; and poor results demonstrated significant contour abnormalities. Overall cosmesis was subjectively graded on the patient’s complete postoperative eyelid appearance.
Technique
The upper eyelid was everted and approximately 0.5-1.0 cc of 1% lidocaine with 1:100,000 epinephrine was injected subconjunctivally above the superior border of the tarsal plate. The amount of tissue to be resected was based on a modified Putterman and Fett algorithm [12], where moderate ptosis underwent a tissue resection of approximately 8.5mm, and severe cases had +1.0mm additional resection for every 0.5mm change in lid height desired. Two curved hemostats were clamped horizontally tip to tip toward the distal border of the everted lid. Adouble-armed 6-0 nylon suture was passed proximal to the hemostat clamps in a repeating horizontal mattress fashion across the everted lid margin, passing through the tarsal plate, Müller’s muscle, and conjunctiva. The hemostats were then removed, and the excess tissue distal to the horizontal mattress sutures was excised by cutting along the line of tissue compressed by the hemostat clamps. The ends of the sutures on the conjunctival side were passed through the wound edges and out through the lid crease onto the skin. Each end of the suture was tied upon itself in close apposition to the skin.
RESULTS
In our study, the Fasanella-Servat operation was performed by a single surgeon on 40 eyelids of 24 patients. There were 10 female and 14 male patients. Out of the 40 eyelids operated on, 22 were on the right side and 18 were on the left side.
The mean pre-operative MRD1 was 0.02mm and the mean post-operative MRD1 was 3.14mm (Table 1). Inpatients with severe ptosis of MRD1 ≤0 (n=11), the average pre-operative MRD1 was -1.3mm and post-operative MRD1 was +2.5mm (Table 1). The maximum value of pre-operative MRD1 measured in the patients was -3mm and the maximum post-operative MRD1 measured was +4.5mm. On average, approximately 9-10mm of tissue was resected.
The mean pre-operative MRD1 was 0.02mm and the mean post-operative MRD1 was 3.14mm (Table 1). Inpatients with severe ptosis of MRD1 ≤0 (n=11), the average pre-operative MRD1 was -1.3mm and post-operative MRD1 was +2.5mm (Table 1). The maximum value of pre-operative MRD1 measured in the patients was -3mm and the maximum post-operative MRD1 measured was +4.5mm. On average, approximately 9-10mm of tissue was resected.
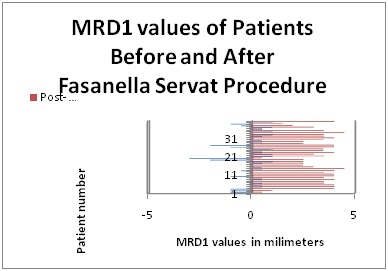
Table 1: MRD1 values of patients before and after Fasanella-Servat procedure.
The table above shows the absolute pre-operative (blue) and post-operative (red) values in millimeters along the x-axis and the patient number along the y-axis.
Excellent procedure outcome as determined by the MRD1 value of ≥2.5 and ≤4mm was seen in 32 cases (80%). A satisfactory outcome with MRD1 of ≥1 and 4mm was seen in 5 cases (12.5%). (Table 2)Analyzing only patients with severe blepharoptosis, 6/11 cases (55%) had excellent surgical outcomes, 3/11 (27%) had satisfactory outcomes, and 2/11 (18%) had poor surgical outcomes (Table 3). Most of the eyelids operated upon had an acceptable outcome based on evaluation by an oculofacial surgeon for eyelid height, contour, symmetry and cosmesis (Figure 1). There was one case of eyelid contour abnormality in the form of lateral peaking, and this required revision. Additional complications included inclusion cysts in two patients and ectopic lashes in one patient.
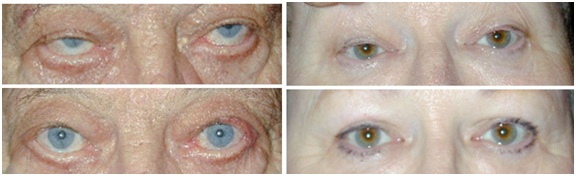
Figure 1: Pre-and post-operative comparison of eyelid position and cosmesis.
2 patients who underwent Fasanella-Servat operation for correction of moderate to severe blepharoptosis. The patient on the left exhibited severe blepharoptosis of the right upper lid with a negative MRD1, and moderate ptosis of the left upper lid. The patient on the right displayed moderate blepharoptosis bilaterally.
Upper row: pre-operative eyelid position. Lower row: post-operative appearance.
Upper row: pre-operative eyelid position. Lower row: post-operative appearance.
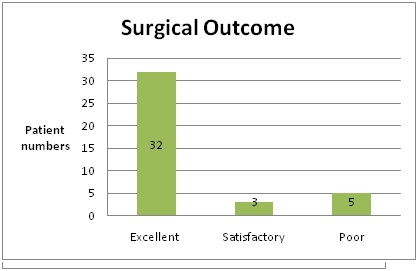
Table 2: Pool data for surgical outcomes following Fasanella-Servat operation for moderate to severe ptosis.
Excellent outcome corresponded to MRD1 value of ≥2.5 and ≤4mm, and was seen in 32 cases (80%). Satisfactory outcome of MRD1 of ≥1 and <2.5mm was seen in 3 cases (7.5%). Poor outcome of MRD1 value either <1mm or >4mm was seen in 5 cases (12.5%).
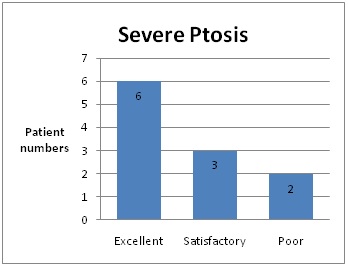
Table 3: Surgical outcomes following Fasanella-Servat operation for patients with severe ptosis with MRD1 ≤0 mm.
6 of 11 cases (55%) had excellent surgical outcomes with MRD1 value of ≥2.5 and ≤4mm. 3 of 11 cases (27%) had satisfactory outcomes of MRD1 ≥1 and <2.5mm. 2 of 11 cases (18%) had poor surgical outcomes with MRD1 either <1mm or >4mm.
DISCUSSION
Blepharoptosis is the drooping of the upper eyelid such that it covers more than the upper 2mm of the cornea. To quantify the degree of ptosis, the vertical palpebral fissure height and distance from the upper eyelid margin to the pupillary light reflex are measured. The resultant MRD1 values can classify blepharoptosis as mild, moderate, or severe.
Historically, a variety of procedures have been employed for the correction of blepharoptosis. Select examples include frontalis suspension by Scarpa in 1806 and frontalis sling by De Wecker in 1882, tarsus and levator palpebrae superior is resection by Bowman in 1884, superior rectus and tarsal coupling by Motais and Parinaud in 1897, and conjunctival-tarsal-mullerectomy by Fasanella and Servat in 1961 [9]. The Fasanella-Servat operation was widely adopted as a faster, less technically demanding surgery for repair of blepharoptosis with predictable results [1,9].
Since its introduction in 1961, the Fasanella-Servat procedure was intended only for cases of minimal ptosis (<3mm) with levator function of more than 10mm [1]. Classically, a Fasanella-Servat procedure was not a preferred surgical option for patients with a moderate to severe degree of ptosis instead, such patients were considered good candidates for levator muscle advancement or levator muscle resection surgeries. Our study aims to demonstrate that the Fasanella-Servat operation can yield favorable outcomes in moderate to severe degrees of blepharoptosis.
In patients with moderate to severe blepharoptosis (MRD1 value of <1mm) with good levator function (levator excursion of >10mm), excellent surgical outcomes as defined by an MRD1 ≥2.5 and ≤4mm were obtained in 32/40 cases (80%) after a Fasanella-Servat operation. Satisfactory outcomes with MRD1 ≥1 and <2.5mm were seen in 3/40 cases (7.5%), and poor surgical outcomes with MRD1 <1mm or >4mm were observed in 5/40 cases (12.5%). With specific attention to cases of severe blepharoptosis, 6/11 cases (55%) had excellent surgical outcomes, while 3/11 (27%) had satisfactory outcomes, and only 2/11 (18%) had poor surgical outcomes. Overall, 35/40 cases (87.5%) had a good outcome regarding eyelid position and cosmesis. Post-operative complications included eyelid contour abnormality (lateral peaking) in one patient requiring surgical revision. Another two patients experienced inclusion cysts and one developed ectopic lashes.
A recent large study showed an average MRD1 elevation of 2mm after undergoing a Fasanella-Servat procedure [2]. However, some patients in our series showed a large post-operative MRD1 improvement of >3-4mm. This may be due to varying degrees of tissue resection; however, this study is based on the work of a single surgeon diagnosing mild, moderate, and severe ptosis and the corresponding amount of tissue resected, and this minimized deviation in tissue excision. Previous studies offer conflicting reasons for the degree of MRD1 improvement after the conjunctival-tarsal-mullerectomy of the Fasanella-Servat operation. Some posit that shortening Müller’s muscle has little to no effect on blepharoptosis repair and that no correlation is found between the amount of tarsus excised and the degree of lid elevation achieved [4]. Histopathologic analysis suggests a perhaps inadvertent combined excision of the posterior layer of levator aponeurosis with mullerectomy [13], though other studies refute levator resection [3,8]. Our cases did not include histopathologic analysis. It is possible that inadvertent excision of the posterior layer of levator occurred, though our findings could also be attributed to the degree of overall shortening of the vertical posterior lamella, wound contracture, and advancement of Müller’s muscle along tarsus [4,6].
It is not uncommon for severe ptosis cases to have concurrent poor levator function. We excluded cases with levator action of <10mm in order to minimize pathologic variables when comparing the efficacy of the Fasanella-Servat procedure in our moderate to severe blepharoptosis patients versus the classic patient with minimal ptosis and good levator function [1]. Future work could assess the utility of a Fasanella-Servat procedure in cases of blepharoptosis with poor levator function.
It should be noted that involutional ptosis exhibits age-dependent changes, and it would be of interest to determine any correlation between our surgical outcomes and patient age. While patient age and its relationship to surgical outcomes was not evaluated in the present study, recent work found no relationship between age and need for reoperation, suggesting a durable surgical outcome across a range of patient ages [14]. Going forward, analysis of surgical outcomes based on patient age and duration of follow-up would be a useful contribution to the literature.
The Fasanella-Servat operation is a fast, powerful and reliable procedure. This data suggests that a Fasanella-Servat procedure may be considered a viable alternative to external levator advancement or levator muscle resection procedures in patients with a pre-operative MRD1 of < mm and good levator function.
Historically, a variety of procedures have been employed for the correction of blepharoptosis. Select examples include frontalis suspension by Scarpa in 1806 and frontalis sling by De Wecker in 1882, tarsus and levator palpebrae superior is resection by Bowman in 1884, superior rectus and tarsal coupling by Motais and Parinaud in 1897, and conjunctival-tarsal-mullerectomy by Fasanella and Servat in 1961 [9]. The Fasanella-Servat operation was widely adopted as a faster, less technically demanding surgery for repair of blepharoptosis with predictable results [1,9].
Since its introduction in 1961, the Fasanella-Servat procedure was intended only for cases of minimal ptosis (<3mm) with levator function of more than 10mm [1]. Classically, a Fasanella-Servat procedure was not a preferred surgical option for patients with a moderate to severe degree of ptosis instead, such patients were considered good candidates for levator muscle advancement or levator muscle resection surgeries. Our study aims to demonstrate that the Fasanella-Servat operation can yield favorable outcomes in moderate to severe degrees of blepharoptosis.
In patients with moderate to severe blepharoptosis (MRD1 value of <1mm) with good levator function (levator excursion of >10mm), excellent surgical outcomes as defined by an MRD1 ≥2.5 and ≤4mm were obtained in 32/40 cases (80%) after a Fasanella-Servat operation. Satisfactory outcomes with MRD1 ≥1 and <2.5mm were seen in 3/40 cases (7.5%), and poor surgical outcomes with MRD1 <1mm or >4mm were observed in 5/40 cases (12.5%). With specific attention to cases of severe blepharoptosis, 6/11 cases (55%) had excellent surgical outcomes, while 3/11 (27%) had satisfactory outcomes, and only 2/11 (18%) had poor surgical outcomes. Overall, 35/40 cases (87.5%) had a good outcome regarding eyelid position and cosmesis. Post-operative complications included eyelid contour abnormality (lateral peaking) in one patient requiring surgical revision. Another two patients experienced inclusion cysts and one developed ectopic lashes.
A recent large study showed an average MRD1 elevation of 2mm after undergoing a Fasanella-Servat procedure [2]. However, some patients in our series showed a large post-operative MRD1 improvement of >3-4mm. This may be due to varying degrees of tissue resection; however, this study is based on the work of a single surgeon diagnosing mild, moderate, and severe ptosis and the corresponding amount of tissue resected, and this minimized deviation in tissue excision. Previous studies offer conflicting reasons for the degree of MRD1 improvement after the conjunctival-tarsal-mullerectomy of the Fasanella-Servat operation. Some posit that shortening Müller’s muscle has little to no effect on blepharoptosis repair and that no correlation is found between the amount of tarsus excised and the degree of lid elevation achieved [4]. Histopathologic analysis suggests a perhaps inadvertent combined excision of the posterior layer of levator aponeurosis with mullerectomy [13], though other studies refute levator resection [3,8]. Our cases did not include histopathologic analysis. It is possible that inadvertent excision of the posterior layer of levator occurred, though our findings could also be attributed to the degree of overall shortening of the vertical posterior lamella, wound contracture, and advancement of Müller’s muscle along tarsus [4,6].
It is not uncommon for severe ptosis cases to have concurrent poor levator function. We excluded cases with levator action of <10mm in order to minimize pathologic variables when comparing the efficacy of the Fasanella-Servat procedure in our moderate to severe blepharoptosis patients versus the classic patient with minimal ptosis and good levator function [1]. Future work could assess the utility of a Fasanella-Servat procedure in cases of blepharoptosis with poor levator function.
It should be noted that involutional ptosis exhibits age-dependent changes, and it would be of interest to determine any correlation between our surgical outcomes and patient age. While patient age and its relationship to surgical outcomes was not evaluated in the present study, recent work found no relationship between age and need for reoperation, suggesting a durable surgical outcome across a range of patient ages [14]. Going forward, analysis of surgical outcomes based on patient age and duration of follow-up would be a useful contribution to the literature.
The Fasanella-Servat operation is a fast, powerful and reliable procedure. This data suggests that a Fasanella-Servat procedure may be considered a viable alternative to external levator advancement or levator muscle resection procedures in patients with a pre-operative MRD1 of < mm and good levator function.
REFERENCES
- Fasanella RM, Servat J (1961) Levator resection for minimal ptosis: another simplified operation. Arch Ophthalmol 65: 493-496.
- Pang NK, Newsom RW, Oestreicher JH, Chung HT, Harvey JT (2008) Fasanella-Servat procedure: indications, efficacy and complications. Can J Ophthalmol 43: 84-88.
- Beard C (1970) Blepharoptosis repair by modified Fasanella-Servat operation. Am J Ophthalmol 69: 850-857.
- Buckman G, Jakobiec FA, Hyde K, Lisman RD, Hornblass A, et al. (1989) Success of the Fasanella-Servat operation independent of Müller’s smooth muscle excision. Ophthalmology 96: 413-418.
- Wiggs EO (1978) The Fasanella-Servat operation. Ophthalmic Surg 9: 48-57.
- Beard C (1966) The surgical treatment of blepharoptosis: a quantitative approach. Trans Am Ophthalmol Soc 64: 401-487.
- Betharia SM, Grover AK, Kalra BR (1983) The Fasanella-Servat operation: a modified simple technique with quantitative approach. Br J Ophthalmol 67: 58-60.
- Putterman AM (1972) A clamp for strengthening Müller’s muscle in the treatment of ptosis. Modification, theory, and clamp for the Fasanella-Servat ptosis operation. Arch Ophthalmol 87: 665-667.
- Gonzalez MO, Durairaj VD (2011) The History of Ptosis Surgery. In: Cohen AJ, Weinberg DA (Eds.). Evaluation and Management of Blepharoptosis. Springer New York, USA, pg no: 5-11.
- Lauring L (1977) Blepharoptosis correction with the sutureless Fasanella-Servat operation. Arch Ophthalmol 95: 671-674.
- Rosenberg C, Lelli GJ Jr, Lisman RD (2009) Early Postoperative Adjustment of the Fasanella-Servat Procedure: Review of 102 Consecutive Cases. Ophthal Plast Reconstr Surg 25: 19-22.
- Putterman AM, Fett DR (1986) Müller's muscle in the treatment of upper eyelid ptosis: a ten-year study. Ophthalmic Surg 17: 354-360.
- Maheshwari R, Maheshwari S (2011) Muller’s muscle resection for ptosis and relationship with levator and Muller’s muscle function. Orbit 30: 150-153.
- Suga H, Ozaki M, Narita K, Shiraishi T, Takushima A, et al. (2017) Preoperative asymmetry is a risk factor for reoperation in involutional blepharoptosis. J Plast Reconstr Aesthet Surg 70: 686-691.
Citation: Gonzalez MO, Singh N, Simmons B, Willoughby B (2017) Fasanella-Servat Operation for Moderate to Severe Blepharoptosis. J Ophthalmic Clin Res 4: 030.
Copyright: © 2017 Mithra O Gonzalez, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
© 2026, Copyrights Herald Scholarly Open Access. All Rights Reserved!

